Abstract
Background
Urologists may hesitate to offer transurethral resection of the prostate (TURP) because of increased morbidity in elderly patients.
Aims
We aimed to compare data on postoperative outcomes of elderly men undergoing bipolar transurethral resection of the prostate (B-TURP) as compared to thulium laser vapoenucleation of the prostate (ThuVEP).
Methods
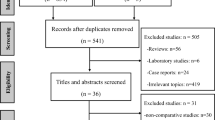
We retrospectively reviewed data of all patients aged ≥ 75 years who underwent benign prostatic hyperplasia surgery. Differences between interventions were estimated using propensity scores (PS) to adjust for different patients characteristics.
Results
Between 2017 and 2020, 275 men were included in the analysis. Propensity score retrieved 65 patients in each group. Median age was 78 (4) years in B-TURP group and 78 (6) in ThuVEP group. Median prostate volume was 63 (35) ml and 54 (24) ml in B-TURP group and ThuVEP group, respectively. Only American Society of Anesthesiologists score was significantly higher in ThuVEP group (p = 0.006). Median operation time, catheterization time, and hospital stay were similar in both groups (55 min, 2 and 3 days). Overall, 84.6% of men had no complications, with no significant differences between the groups (p = 0.234). Only one patient in B-TURP group experienced a Clavien grade IIIb complication. By 1 year, there were a statistically significant differences in International Prostate Symptom Score (p = 0.000) in favor of B-TURP group and in maximal urine flow rate (p = 0.000) in favor of ThuVEP group.
Discussion and conclusions
Both procedures showed excellent functional improvements one year after surgery with a low rate of major complications in men aged ≥ 75 years with small-to-medium sized prostates.
Similar content being viewed by others
Availability of data and materials
The datasets generated and analyzed during the current study are available in the Mendeley Data repository (persistent web link to datasets: Mendeley Data, V1, https://doi.org/10.17632/6hhb9768j3.1. http://dx.doi.org/10.17632/6hhb9768j3.1).
References
Bushman W (2009) Etiology, epidemiology, and natural history. Urol Clin North Am 36:403–415. https://doi.org/10.1016/j.ucl.2009.07.003
Girman CJ, Jacobsen SJ, Guess HA et al (1995) Natural history of prostatism: relationship among symptoms, prostate volume and peak urinary flow rate. J Urol 153:1510–1515
Egan KB (2016) The epidemiology of benign prostatic hyperplasia associated with lower urinary tract symptoms: prevalence and incident rates. Urol Clin North Am 43:289–297. https://doi.org/10.1016/j.ucl.2016.04.001
Platz EA, Smit E, Curhan GC et al (2002) Prevalence of and racial/ethnic variation in lower urinary tract symptoms and non-cancer prostate surgery in U.S. men. Urology 59:877–883. https://doi.org/10.1016/s0090-4295(01)01673-9
Jacobsen SJ, Guess HA, Panser L et al (1993) A population-based study of health care-seeking behavior for treatment of urinary symptoms. The Olmsted County Study of Urinary Symptoms and Health Status Among Men. Arch Fam Med 2:729–735
Mebust WK, Holtgrewe HL, Cockett ATK et al (1989) Transurethral prostatectomy: Immediate and postoperative complications. Cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol 141:243–247
Alexander CE, Scullion MMF, Omar MI et al (2020) Reprint—bipolar vs. monopolar transurethral resection of the prostate for lower urinary tract symptoms secondary to benign prostatic obstruction: a cochrane review. Can Urol Assoc J 14:423–430. https://doi.org/10.5489/cuaj.6464
Castellani D, Pirola GM, Pacchetti A et al (2020) State of the art of thulium laser enucleation and vapoenucleation of the prostate: a systematic review. Urology 136:19–34. https://doi.org/10.1016/j.urology.2019.10.022
Oelke M, Bachmann A, Descazeaud A et al (2013) EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 64:118–140. https://doi.org/10.1016/j.eururo.2013.03.004
Culkin DJ, Exaire EJ, Green D et al (2014) Anticoagulation and antiplatelet therapy in urological practice: ICUD/AUA review paper. J Urol 192:1026–1034. https://doi.org/10.1016/j.juro.2014.04.103
Dellabella M, Castellani D (2018) Anatomical control of adenoma technique: an accurate surgical approach to thulium laser enucleation of the prostate. Urology 113:252. https://doi.org/10.1016/j.urology.2017.11.037
Nesbit RM (1951) Transurethral prostatic resection: a discussion of some principles and problems. J Urol 66:362–372. https://doi.org/10.1016/s0022-5347(17)74350-9
Bach T, Wölbling F, Gross AJ et al (2017) Prospective assessment of perioperative course in 2648 patients after surgical treatment of benign prostatic obstruction. World J Urol 35:285–292. https://doi.org/10.1007/s00345-016-1866-7
Yang Z, Liu T, Wang X (2016) Comparison of thulium laser enucleation and plasmakinetic resection of the prostate in a randomized prospective trial with 5-year follow-up. Lasers Med Sci 31:1797–1802. https://doi.org/10.1007/s10103-016-2052-2
Bozzini G, Seveso M, Melegari S et al (2017) Thulium laser enucleation (ThuLEP) versus transurethral resection of the prostate in saline (TURis): a randomized prospective trial to compare intra and early postoperative outcomes. Actas Urol Esp 41:309–315. https://doi.org/10.1016/j.acuro.2016.06.010
Yang Z, Wang X, Liu T (2013) Thulium laser enucleation versus plasmakinetic resection of the prostate: a randomized prospective trial with 18-month follow-up. Urology 81:396–400. https://doi.org/10.1016/j.urology.2012.08.069
Nordling J (2002) The aging bladder-a significant but underestimated role in the development of lower urinary tract symptoms. Exp Gerontol 37:991–999
Scott MC, Winters ME (2015) Congestive heart failure. Emerg Med Clin North Am 33:553–562. https://doi.org/10.1016/j.emc.2015.04.006
Castellani D, Di Rosa M, Gasparri L et al (2020) Thulium laser vapoenucleation of the prostate (ThuVEP) in men at high cardiovascular risk and on antithrombotic therapy: a single-center experience. J Clin Med 9:917. https://doi.org/10.3390/jcm9040917
Castellani D, Pirola GM, Gasparri L et al (2019) Are outcomes of thulium laser enucleation of the prostate different in men aged 75 and over? A propensity score analysis. Urology 132:170–176. https://doi.org/10.1016/j.urology.2019.06.025
Orimo H, Ito H, Suzuki T et al (2006) Reviewing the definition of “elderly.” Geriatr Gerontol Int 6:149–158. https://doi.org/10.1111/j.1447-0594.2006.00341.x
World Health Organization (2015) Significant loss of functional ability, and care dependence. In: World Rep. Aging Heal. http://apps.who.int/iris/bitstream/handle/10665/186463/9789240694811_eng.pdf;jsessionid=2342855AC115632C5C15C1B21BAC57F9?sequence=1. Accessed 8 Feb 2021
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by GP, ER, MG, GMP, and LG. MDR performed statistical analysis. The first draft of the manuscript was written by DC and all authors commented on previous versions of the manuscript. AA and MD supervised the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Human/animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments.
Ethical approval
The study has been approved by a IRCCS INRCA Ethical Board (DGEN 421/2017).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Castellani, D., Di Rosa, M., Pace, G. et al. Comparison between thulium laser vapoenucleation and plasmakinetic resection of the prostate in men aged 75 years and older in a real-life setting: a propensity score analysis. Aging Clin Exp Res 33, 1757–1763 (2021). https://doi.org/10.1007/s40520-021-01868-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-021-01868-1