Abstract
Background
Heart rate has been found associated with mortality in critically ill patients. However, whether the association differs between the elderly and non-elderly patients was unknown.
Methods
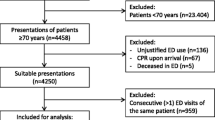
We conducted a retrospective observational study of adult patients admitted to the intensive care unit (ICU) in the United States. Demographic, vital signs, laboratory tests, and interventions were extracted and compared between the elderly and non-elderly patients. The main exposure was heart rate, the proportion of time spent in heart rate (PTS-HR) was calculated. The primary outcome was hospital mortality. The multivariable logistic regression model was performed to assess the relationship between PTS-HR and hospital mortality, and interaction between PTS-HR and age categories was explored.
Results
104,276 patients were included, of which 52,378 (50.2%) were elderly patients and 51,898 (49.8%) were non-elderly patients. The median age was 66 (IQR 54–76) years. After adjusting for confounders, PTS-HR < 60 beats per minute (bpm) (OR 0.972, 95% CI [0.945, 0.998], p = 0.031, Pinteraction = 0.001) and 60–80 bpm (OR 0.925, 95% CI [0.912, 0.938], p < 0.001, Pinteraction = 0.553) were associated with decreased risk of mortality; PTS-HR 80–100 bpm was associated with decreased mortality in the non-elderly patients (OR 0.955, 95% CI [0.941,0.975], p < 0.001) but was associated with increased mortality in the very elderly patients (OR 1.018, 95% CI [1.003,1.029], p = 0.017, Pinteraction < 0.001). PTS-HR > 100 bpm (OR 1.093, 95% CI [1.081,1.105], p < 0.001, Pinteraction = 0.004) was associated with increased mortality.
Conclusions
The effect of heart rate on hospital mortality differs between the elderly and non-elderly critically ill patients.



Similar content being viewed by others
Availability of data and materials
Data analyzed during the present study are currently stored in the eICU database (eicu-crd.mit.edu).
References
Vincent JL, Marshall JC, Namendys-Silva SA et al (2014) Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med 2:380–386. https://doi.org/10.1016/s2213-2600(14)70061-x
Adhikari NKJ, Fowler RA, Bhagwanjee S et al (2010) Critical care and the global burden of critical illness in adults. Lancet 376:1339–1346. https://doi.org/10.1016/s0140-6736(10)60446-1
Illescas AH, Kache PA, Whittemore K et al (2020) Hospitalizations involving an intensive care unit admission among patients aged 65 years and older within New York City Hospitals during 2000–2014. Med Care 58:74–82. https://doi.org/10.1097/mlr.0000000000001224
Chin-Yee N, D'Egidio G, Thavorn K et al (2017) Cost analysis of the very elderly admitted to intensive care units. Crit Care 21:109. https://doi.org/10.1186/s13054-017-1689-y
Ball IM, Bagshaw SM, Burns KE et al (2017) Outcomes of elderly critically ill medical and surgical patients: a multicentre cohort study. Can J Anaesth Journal canadien d'anesthesie 64:260–269. https://doi.org/10.1007/s12630-016-0798-4
Flaatten H, Garrouste-Orgeas M (2015) The very old ICU patient: a never-ending story. Intensive Care Med 41:1996–1998. https://doi.org/10.1007/s00134-015-4052-2
Heyland DK, Garland A, Bagshaw SM et al (2015) Recovery after critical illness in patients aged 80 years or older: a multi-center prospective observational cohort study. Intensive Care Med 41:1911–1920. https://doi.org/10.1007/s00134-015-4028-2
Sacanella E, Perez-Castejon JM, Nicolas JM et al (2011) Functional status and quality of life 12 months after discharge from a medical ICU in healthy elderly patients: a prospective observational study. Crit Care 15:R105. https://doi.org/10.1186/cc10121
Blot S, Koulenti D, Dimopoulos G et al (2014) Prevalence, risk factors, and mortality for ventilator-associated pneumonia in middle-aged, old, and very old critically ill patients*. Crit Care Med 42:601–609. https://doi.org/10.1097/01.ccm.0000435665.07446.50
Verrier RL, Tan A (2009) Heart rate, autonomic markers, and cardiac mortality. Heart Rhythm 6:S68–75. https://doi.org/10.1016/j.hrthm.2009.07.017
Fox KM, Ferrari R (2011) Heart rate: a forgotten link in coronary artery disease? Nat Rev Cardiol 8:369–379. https://doi.org/10.1038/nrcardio.2011.58
Caetano J, Delgado Alves J (2015) Heart rate and cardiovascular protection. Eur J Intern Med 26:217–222. https://doi.org/10.1016/j.ejim.2015.02.009
Sander O, Welters ID, Foëx P et al (2005) Impact of prolonged elevated heart rate on incidence of major cardiac events in critically ill patients with a high risk of cardiac complications*. Crit Care Med 33:81–88. https://doi.org/10.1097/01.ccm.0000150028.64264.14
Hayashi M, Taniguchi A, Kaku R et al (2019) Prolonged tachycardia with higher heart rate is associated with higher ICU and in-hospital mortality. Acta Med Okayama 73:147–153. https://doi.org/10.18926/amo/56650
Sandfort V, Johnson AEW, Kunz LM et al (2018) Prolonged elevated heart rate and 90-day survival in acutely ill patients: data from the MIMIC-III database. J Intensive Care Med. https://doi.org/10.1177/0885066618756828
Park S, Kim DG, Suh GY et al (2011) Significance of new-onset prolonged sinus tachycardia in a medical intensive care unit: a prospective observational study. J Crit Care 26:e531–e538. https://doi.org/10.1016/j.jcrc.2011.01.001
Zimmerman JE, Kramer AA, McNair DS et al (2006) Acute physiology and chronic health evaluation (APACHE) IV: hospital mortality assessment for today's critically ill patients. Crit Care Med 34:1297–1310. https://doi.org/10.1097/01.CCM.0000215112.84523.F0
Le Gall JR, Klar J, Lemeshow S et al (1996) The logistic organ dysfunction system. A new way to assess organ dysfunction in the intensive care unit. ICU Scoring Group. JAMA 276:802–810. https://doi.org/10.1001/jama.276.10.802
Le Gall JR, Loirat P, Alperovitch A et al (1984) A simplified acute physiology score for ICU patients. Crit Care Med 12:975–977. https://doi.org/10.1097/00003246-198411000-00012
Li K, Yao C, Yang X et al (2017) Effect of resting heart rate on all-cause mortality and cardiovascular events according to age. J Am Geriatr Soc 65:989–994. https://doi.org/10.1111/jgs.14714
Pollard TJ, Johnson AEW, Raffa JD et al (2018) The eICU collaborative research database, a freely available multi-center database for critical care research. Sci Data 5:180178. https://doi.org/10.1038/sdata.2018.178
Lanspa MJ, Krinsley JS, Hersh AM et al (2019) Percentage of time in range 70 to 139 mg/dL Is associated with reduced mortality among critically Ill patients receiving IV insulin infusion. Chest 156:878–886. https://doi.org/10.1016/j.chest.2019.05.016
Krinsley JS, Preiser JC (2015) Time in blood glucose range 70 to 140 mg/dl >80% is strongly associated with increased survival in non-diabetic critically ill adults. Crit Care 19:179. https://doi.org/10.1186/s13054-015-0908-7
Zhou DW, Li ZM, Zhang SL et al (2020) The optimal peripheral oxygen saturation may be 95–97% for post-cardiac arrest patients: a retrospective observational study. Am J Emerg Med. https://doi.org/10.1016/j.ajem.2020.01.038
Andrews TC, Fenton T, Toyosaki N et al (1993) Subsets of ambulatory myocardial ischemia based on heart rate activity. Circadian distribution and response to anti-ischemic medication. The Angina and Silent Ischemia Study Group (ASIS). Circulation 88:92–100. https://doi.org/10.1161/01.cir.88.1.92
Heidland UE, Strauer BE (2001) Left ventricular muscle mass and elevated heart rate are associated with coronary plaque disruption. Circulation 104:1477–1482. https://doi.org/10.1161/hc3801.096325
Custodis F, Schirmer SH, Baumhakel M et al (2010) Vascular pathophysiology in response to increased heart rate. J Am Coll Cardiol 56:1973–1983. https://doi.org/10.1016/j.jacc.2010.09.014
Omlor AJ, Trudzinski FC, Alqudrah M et al (2019) Time-updated resting heart rate predicts mortality in patients with COPD. Clin Res Cardiol: official journal of the German Cardiac Society. https://doi.org/10.1007/s00392-019-01572-1
Hillis GS, Woodward M, Rodgers A et al (2012) Resting heart rate and the risk of death and cardiovascular complications in patients with type 2 diabetes mellitus. Diabetologia 55:1283–1290. https://doi.org/10.1007/s00125-012-2471-y
Aune D, Sen A, o’Hartaigh B et al (2017) Resting heart rate and the risk of cardiovascular disease, total cancer, and all-cause mortality—a systematic review and dose-response meta-analysis of prospective studies. Nutrition, metabolism, and cardiovascular diseases. NMCD 27:504–517. https://doi.org/10.1016/j.numecd.2017.04.004
Jensen MT, Marott JL, Lange P et al (2013) Resting heart rate is a predictor of mortality in COPD. Eur Respir J 42:341–349. https://doi.org/10.1183/09031936.00072212
Anselmino M, Ohrvik J, Ryden L (2010) Resting heart rate in patients with stable coronary artery disease and diabetes: a report from the euro heart survey on diabetes and the heart. Eur Heart J 31:3040–3045. https://doi.org/10.1093/eurheartj/ehq368
Aladin AI, Whelton SP, Al-Mallah MH et al (2014) Relation of resting heart rate to risk for all-cause mortality by gender after considering exercise capacity (the Henry Ford exercise testing project). Am J Cardiol 114:1701–1706. https://doi.org/10.1016/j.amjcard.2014.08.042
Sharashova E, Wilsgaard T, Løchen M-L et al (2017) Resting heart rate trajectories and myocardial infarction, atrial fibrillation, ischaemic stroke and death in the general population: the tromsø study. Eur J Prev Cardiol 24:748–759. https://doi.org/10.1177/2047487316688983
Grander W, Mullauer K, Koller B et al (2013) Heart rate before ICU discharge: a simple and readily available predictor of short- and long-term mortality from critical illness. Clin Res Cardiol: official journal of the German Cardiac Society 102:599–606. https://doi.org/10.1007/s00392-013-0571-4
Hoke RS, Muller-Werdan U, Lautenschlager C et al (2012) Heart rate as an independent risk factor in patients with multiple organ dysfunction: a prospective, observational study. Clin Res Cardiol: official journal of the German Cardiac Society 101:139–147. https://doi.org/10.1007/s00392-011-0375-3
Whelton SP, Narla V, Blaha MJ et al (2014) Association between resting heart rate and inflammatory biomarkers (high-sensitivity C-reactive protein, interleukin-6, and fibrinogen) (from the Multi-Ethnic Study of Atherosclerosis). Am J Cardiol 113:644–649. https://doi.org/10.1016/j.amjcard.2013.11.009
Whelton SP, Blankstein R, Al-Mallah MH et al (2013) Association of resting heart rate with carotid and aortic arterial stiffness: multi-ethnic study of atherosclerosis. Hypertension 62:477–484. https://doi.org/10.1161/HYPERTENSIONAHA.113.01605
Knaus WA, Wagner DP, Draper EA et al (1991) The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest 100:1619–1636. https://doi.org/10.1378/chest.100.6.1619
Palatini P, Julius S (1997) Heart rate and the cardiovascular risk. J Hypertens 15:3–17. https://doi.org/10.1097/00004872-199715010-00001
Saxena A, Minton D, Lee DC et al (2013) Protective role of resting heart rate on all-cause and cardiovascular disease mortality. Mayo Clin Proc 88:1420–1426. https://doi.org/10.1016/j.mayocp.2013.09.011
Benetos A, Thomas F, Bean K et al (2003) Resting heart rate in older people: a predictor of survival to age 85. J Am Geriatr Soc 51:284–285. https://doi.org/10.1046/j.1532-5415.2003.51080.x
Oksanen T, Tiainen M, Vaahersalo J et al (2018) Lower heart rate is associated with good one-year outcome in post-resuscitation patients. Resuscitation 128:112–118. https://doi.org/10.1016/j.resuscitation.2018.05.001
Thomsen JH, Nielsen N, Hassager C et al (2016) Bradycardia during targeted temperature management: an early marker of lower mortality and favorable neurologic outcome in comatose out-of-hospital cardiac arrest patients. Crit Care Med 44:308–318. https://doi.org/10.1097/ccm.0000000000001390
Staer-Jensen H, Sunde K, Olasveengen TM et al (2014) Bradycardia during therapeutic hypothermia is associated with good neurologic outcome in comatose survivors of out-of-hospital cardiac arrest. Crit Care Med 42:2401–2408. https://doi.org/10.1097/ccm.0000000000000515
London MJHK, Schwartz GG, Henderson WG (2013) Association of perioperative β-blockade with mortality and cardiovascular morbidity following major noncardiac surgery. JAMA 309(16):1704–1713
Morelli A, Singer M, Ranieri VM et al (2016) Heart rate reduction with esmolol is associated with improved arterial elastance in patients with septic shock: a prospective observational study. Intensive Care Med 42:1528–1534. https://doi.org/10.1007/s00134-016-4351-2
Morelli A, Donati A, Ertmer C et al (2013) Microvascular effects of heart rate control with esmolol in patients with septic shock: a pilot study. Crit Care Med 41:2162–2168. https://doi.org/10.1097/CCM.0b013e31828a678d
Morelli A, Ertmer C, Westphal M et al (2013) Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: a randomized clinical trial. JAMA 310:1683–1691. https://doi.org/10.1001/jama.2013.278477
Doty E, Stone DJ, McCague N et al (2019) Counterintuitive results from observational data: a case study and discussion. BMJ open 9:e026447. https://doi.org/10.1136/bmjopen-2018-026447
Benetos A, Rudnichi A, Thomas F et al (1999) Influence of heart rate on mortality in a French population: role of age, gender, and blood pressure. Hypertension 33:44–52. https://doi.org/10.1161/01.hyp.33.1.44
Tadic M, Cuspidi C, Grassi G (2018) Heart rate as a predictor of cardiovascular risk. Eur J Clin Invest. https://doi.org/10.1111/eci.12892
Funding
This study was supported by grants from ‘Beijing Municipal Science and Technology Commission-Capital clinical application research’ (Z181100001718068).
Author information
Authors and Affiliations
Contributions
DZ and JZ conceived this study. DZ extracted the data. DZ, and ZL designed the statistical analyses. DZ, JZ performed the statistical analyses. DZ and ZL wrote the first draft of the manuscript. GS and JZ reviewed and modified the final manuscript. All authors read, critically reviewed, and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
None of the authors has declared a conflict of interest.
Ethical approval
The schema of eICU database was established in collaboration with Privacert (Cambridge, MA), who certified the re-identification risk as meeting safe harbor standards (HIPAA Certification no. 1031219-2). All tables in eICU database were deidentified to meet the safe harbor provision of the US HIPAA. Due to the HIPAA compliant de-identification in this database, our institutional review board requirement was waived.
Statement of human and animal rights
This article is a secondary data analysis from the eICU database, and all necessary permissions were obtained to access and use the data. The present work adhered to the rules regulating research for humans and was conducted strictly according to the Declaration of Helsinki.
Informed consent
Informed consent from participants was waived because the study was retrospective, and the eICU database contains de-identified information, which does not affect the rights and welfare of the participants.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhou, D., Li, Z., Shi, G. et al. Effect of heart rate on hospital mortality in critically ill patients may be modified by age: a retrospective observational study from large database. Aging Clin Exp Res 33, 1325–1335 (2021). https://doi.org/10.1007/s40520-020-01644-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01644-7