Abstract
Background
Since oral organs function in the first stage of the swallowing process, it is possible that decline in swallowing function can be partly related to oral frailty.
Aims
The purpose of this study was to investigate the association between swallowing function and oral function among community-dwelling elderly Japanese and to propose cut-off values for screening of decline in swallowing function.
Methods
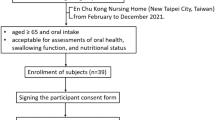
A total of 188 participants were included in the analysis. The number of present teeth and functioning teeth were counted. Bacteria counts in tongue coat, oral wettability, tongue pressure, oral diadochokinesis (ODK), masticatory ability and bite force were examined. Swallowing function was assessed using the 10-item Eating Assessment Tool (EAT-10). Receiver operating characteristic curves were used to determine the cut-off points of each oral function parameter. A logistic regression model was performed to determine the combination of parameters with the highest accuracy for differentiating decline in swallowing function from normal.
Results
Subjects with ODK /pa/ sound < 6.2 times/second had higher prevalence of swallowing problems than those with 6.2 times/second or more. EAT-10 scores of one or more were significantly related to older age (≥ 71 years old; odds ratio [OR] 4.321) and reduced ODK /pa/ sound (< 6.2 times/second; OR 2.914).
Conclusions
Among community-dwelling elderly Japanese, those who were suspected of having decline in swallowing function had lower oral function than those who did not, and the cut-off values were 71 years of age and ODK /pa/ sound 6.2 times/s.

Similar content being viewed by others
References
Pitts T (2014) Airway protective mechanism. Lung 192:27–31
Sasegbon A, Hamdy S (2017) The anatomy and physiology of normal and abnormal swallowing in oropharyngeal dysphagia. Neurogastroenterol Motil. https://doi.org/10.1111/nmo.13100
Pandolfino JE, Gawron AJ (2015) Achalasia: a systematic review. JAMA 313:1841–1852
Forti E, Bonato G, Dioscoridi L et al (2018) A smooth esophageal stricture causing dysphagia. Dysphagia 33:399–402
Kertscher B, Speyer R, Palmieri M et al (2014) Bedside screening to detect oropharyngeal dysphagia in patients with neurological disorders: an updated systematic review. Dysphagia 29:204–212
Takizawa C, Gemmell E, Kenworthy J et al (2016) A systematic review of the prevalence of oropharyngeal dysphagia in stroke, Parkinson’s disease, Alzheimer’s disease, head injury, and pneumonia. Dysphagia 31:434–441
Sura L, Madhavan A, Carnaby G et al (2012) Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging 7:287–298
Lorenzo-López L, Maseda A, Labra C et al (2017) Nutritional determinants of frailty in older adults: a systematic review. BMC Geriatr. https://doi.org/10.1186/s12877-017-0496-2
Iijima K (2015) Upstream preventive strategy for age-related sarcopenia in the elderly: why do the elderly fall into inadequate nutrition? Ann Jpn Prosthodont Soc 7:92–101 (Japanese)
Kera T, Kawai H, Yoshida H et al (2017) Classification of frailty using the Kihon checklist: a cluster analysis of older adults in urban areas. Geriatr Gerontol Int 17:69–77
Watanabe Y, Hirano H, Arai H et al (2017) Relationship between frailty and oral function in community-dwelling elderly adults. J Am Geriatr Soc 65:66–76
Japanese Society of Gerodontology Academic Committee (2016) Deterioration of oral function in the elderly the position paper from Japanese Society of Gerodontology in 2016. Jpn J Gerodontology 31:81–99 (Japanese)
Hara S, Miura H, Kawanishi K et al (2015) The relationship between articulation and probability of aspiration in the rural community-dwelling elderly. Jpn J Gerodontology 30:97–102 (Japanese)
Reddy NP, Costarella BR, Grotz RC et al (1990) Biomedical measurement to characterize the oral phase of dysphagia. IEEE Trans Biomed Eng 37:392–397
Cook IJ, Kahrilas PJ (1999) Aga technical review on management of oropharyngeal dysphagia. Gastroenterology 116:455–478
Belafsky PC, Mouadeb DA, Rees CJ et al (2008) Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol 117:919–924
Matsuo K, Taniguchi H, Nakagawa K et al (2016) Relationships between deterioration of oral functions and nutritional status in elderly patients in an Acute Hospital. Jpn J Gerodontology 31:123–133 (Japanese)
Suzuki A, Kaneko H (2017) Relationship between voluntary cough intensity and the respiratory, physical, oral and swallowing functions of the community-dwelling elderly. J Phys Ther Sci 32:521–525 (Japanese)
Sakayori T, Maki Y, Hirata S et al (2013) Evaluation of a Japanese “Prevention of long-term care” project for the improvement in oral function in the high-risk elderly. Geriatr Gerontol Int 13:451–457
Aoki Y, Oota K (2014) The relationship between tongue pressure and swallowing function in dysphagic patients. Jpn J Dysphagia Rehabil 18:239–248 (Japanese)
Hiraoka A, Yoshikawa M, Nakamori M et al (2017) Maximum tongue pressure is associated with swallowing dysfunction in ALS patients. Dysphagia 32:542–547
Fukada J, Kamlakura Y, Kitake T (2002) Factors related to swallowing function of elderly persons living at home. Jpn J Dysphagia Rehabil 6:38–48 (Japanese)
Okamoto N, Morikawa M, Komatsu M et al (2016) Relationship between loss of teeth and dysphagia, serum albumin, and all-cause mortality in independent elderly-Fujiwara-kyo study. Pre Symptomatic Med Anti Aging 25:28–33 (Japanese)
Tan ECK, Lexomboon D, Sandborgh-Englund G et al (2018) Medicines that cause dry mouth as an adverse effect in older people: a systematic review and meta-analysis. J Am Geriatr Soc 66:76–84
Ando A, Kishi M, Aizawa F et al (2003) The relationship between regular dental check-up and oral health behavior. J Dent Health 53:3–7 (Japanese)
Tanoue H, Ohta K, Kokubo A et al (2008) The influence of a change of posture on swallowing function-change of swallowing function with posture of neck, trunk and lower limbs. Jpn J Dysphagia Rehabil 12:207–213 (Japanese)
Nishiyama K, Sugimoto R, Ebisumoto K et al (2014) A clinical study of the relationship between the swallowing function and physical strength. Deglutition 3:67–74 (Japanese)
Yamaguchi S, Wakayama N, Hideka K et al (2017) Influence of cognitive function on swallowing function. J Jpn Bronchoesophagol Soc 65:441–446 (Japanese)
Acknowledgements
The authors specially thank all participants of the study.
Funding
This work was supported by Japan Society for the Promotion of Science, JSPS KAKENHI grant number 17K12046 and 17H04421.
Author information
Authors and Affiliations
Contributions
NT and MM designed the study, and wrote the initial draft of the manuscript. NT and DE contributed to analysis and interpretation of data, and assisted in the preparation of the manuscript. NS have contributed to data collection. All authors have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
The study protocol was approved by the Ethics Committee of the Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences (No. 1708-028).
Informed consent
All participants provided written informed consent for study participation.
Consent for publication
I confirm that all authors agree with publication in the journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Takeuchi, N., Sawada, N., Ekuni, D. et al. Oral diadochokinesis is related to decline in swallowing function among community-dwelling Japanese elderly: a cross-sectional study. Aging Clin Exp Res 33, 399–405 (2021). https://doi.org/10.1007/s40520-020-01547-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-020-01547-7