Abstract
Background
Interprofessional collaborative practice (ICP) is currently recommended for the delivery of high-quality integrated care for older people. Frailty prevention and management are key elements to be tackled on a multi-professional level.
Aim
This study aims to develop a consensus-based European multi-professional capability framework for frailty prevention and management.
Methods
Using a modified Delphi technique, a consensus-based framework of knowledge, skills and attitudes for all professions involved in the care pathway of older people was developed within two consultation rounds. The template for the process was derived from competency frameworks collected in a comprehensive approach from EU-funded projects of the European Commission (EC) supported best practice models for health workforce development.
Results
The agreed framework consists of 25 items structured in 4 domains of capabilities. Content covers the understanding about frailty, skills for screening and assessment as well as management procedures for every profession involved. The majority of items focused on interprofessional collaboration, communication and person-centred care planning.
Discussion
This framework facilitates clarification of professionals’ roles and standardizes procedures for cross-sectional care processes. Despite a lack of evidence for educational interventions, health workforce development remains an important aspect of quality assurance in health care systems.
Conclusions
The multi-professional capability framework for frailty prevention and management incorporated interprofessional collaborative practice, consistent with current recommendations by the World Health Organization, Science Advice for Policy by European Academies and the European Commission.
Similar content being viewed by others
Background
People at similar chronological age often present with heterogenous biological ageing phenotypes, due to various factors including different life courses, functional abilities and comorbidity. Consequently, frailty has gained increasing interest among health and social care professionals, scientists, public health experts and care planners, highlighting the diversity in self-care capacity among older adults [1].
In fact, the European Commission (EC) has prioritized frailty within the health policy agenda of the majority of the European Union (EU) member states through its “Joint Action on Frailty Prevention” (ADVANTAGE JA) consortium [2]. Despite the absence of evidence supporting education and training programs for professionals involved within the care pathway for older people [3], the consortium assumed that a common competency framework for different professions would support interprofessional collaborative practice (ICP) for integrated and high-quality care for older people [4]. ICP differs from inter- or multi-professional collaboration in terms of hierarchy, role clarification of team members, responsibilities within the team, communication structures and interactions with patients and relatives. Hierarchy structures in ICP teams are flat with no central leader and clear role description for members. ICP is relationship focused and community based. Based on this concept, a set of general and interprofessional core competencies has been discussed for all professions involved in the health care pathways [4].
Furthermore, Ellis and Sevdalis also recommended the development of frameworks for the management of older people to create a capacity to build strong multi-professional teams for the care of older people in different settings [5].
The current study describes the development of a collaborative and multi-professional capability framework for prevention and management of frailty. The study was developed under the auspices of the ADVANTAGE JA in collaboration with the European Geriatric Medicine Society (EuGMS) and aims at establishing multi-professional training standards for improving quality of care of older people.
Methods
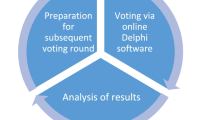
The development of the European Collaborative Interprofessional Capability Framework for Frailty Prevention and Management is based on a consensus process via a modified Delphi technique [6]. A core group of six experts was nominated by the ADVANTAGE JA and the European Geriatric Medicine Society (EuGMS) to guide the process. The group was responsible for the literature survey to develop the template, the conduct of the consensus process, the evaluation of intermediate feedbacks from participants, the communication within the consensus participant panel as well as the summary of results in this publication. This core group consisted of two experts from Austria (RR-W, SL), two experts from Ireland (AL, RC), one expert from United Kingdom (DM) and one expert from Greece (MK).
Selection of experts to run the Delphi survey
Expert choice for creating a consensus was justified upon their involvement in the ADVANTAGE JA and their expertise in the field of frailty management and prevention. Furthermore, members of the Special Interest Group (SIG) in Education and Training of EuGMS were evaluated for their participation in the process. In total, 25 experts from 22 European countries were involved in this process.
Development of the template
The items used in the template for the Delphi process were derived from programs which had been identified as best practice models for frailty prevention in Europe by the ADVANTAGE JA [7]: Capability Framework for Frailty Prevention–UK [8], Sunfrail Project [9], Frailty 360 ° Project [10], FACET Project [11], Frailty training events–UK [12], National Frailty Education Programme–Ireland [13], Frailty for Healthcare Professionals–UK [14], Frailty Training Programs–France [15], Education Module Frailty–UK [16], Postgraduate Certificate in Acute Care of the Older Person with Frailty–UK [17], MSc Specialist Practice Frail older Adults for Health and Social Care–UK [18], Training Programme for Health Care Professionals on detecting pre-frailty and recognizing the initial steps of frailty on primary care–Spain [19], +AGIL–Spain [20], Medical Science Frailty and Integrated Care–UK [21], Perssilaa Project [22] and Frailty Risk Screening in community dwelling older People–France [23]. The single capabilities outlined in the given curricula and catalogues were listed and merged by the core group (data not shown). This exhaustive approach enabled the inclusion and consideration of multiple professions for successful frailty prevention and management, such as geriatricians, physicians, psychologists, public health specialists, dieticians and nursing scientists. Table 1 shows the template for the first round of the Delphi Survey.
Delphi process
The core group pre-defined a consensus rate of > 70% for the integration of a competency into the framework. In this Delphi survey, participants were instructed to rate “yes” or “no” for each item, denoting the inclusion into or exclusion from the framework and to comment on the current wording or suggest new items (Table 1). Free comments were considered, if the item concerned was rated “yes” and/or a reference to the current wording of the item was given by more than 10% of the participants [6]. The participants in the consensus process were granted a deadline of 2 weeks for replying and possibly discussing the items within their institutional teams during each Delphi round.
First Delphi round
Following an implied consent via a reply from an email invitation, the first Delphi round was conducted in February 2019 using the paper-based questionnaire as shown in Table 1. The survey included 6 items on general considerations in the first domain, 4 items on identification of frailty-associated signs and symptoms in the second domain, 6 items on multi-professional collaboration in the third domain and 13 items on management and leadership skills in the fourth domain.
Evaluation of first Delphi round
Responses were counted and feedback of the participants was evaluated by the core group. Items with < 70% acceptance were excluded from the template or re-evaluated in the core group, especially if items nearly reached the threshold of 70%. Additional comments and suggestions were evaluated, revised and integrated within the relevant domains by the core group. The following guiding principles were taken into account during this process:
- I.
Improve the wording and language
- II.
Requests for adding a new item or
- III.
Requests for deleting an item or aspect of it and
- IV.
Requests for merging different items or aspects. The expert group ensured that any modification did not result in the omission of an objective that was considered relevant by the majority of the Delphi panel.
Second Delphi round
The second Delphi round was conducted in March 2019. Participants received an update of the first Delphi round, which consists of 19 items (data not shown). The same procedure of rating and analysis was used as in the first Delphi round.
Results
Altogether, 25 raters, consisting of 20 experts invited to participate in the Delphi process, and 5 experts of the core group, confirmed their willingness to participate in the Delphi survey which was conducted in 2 rounds. In the first round, the experts nominally rated 29 items attributed to 4 domains and 13 sub-domains whether they are regarded important enough to be included in a European Collaborative Interprofessional Framework or not.
The agreed recommendations for a collaborative interprofessional capability framework for prevention and management of frailty are summarized in Table 2. It contains 25 items structured in 4 domains and 13 sub-domains of capabilities.
Domain 1 (six items), covers the understanding of frailty. All items achieved a consensus level greater than 70% in round one. All items (six items) rephrased in round one, achieved full consensus in round two (range between 84 and 100%) without further comments.
Domain 2 (three items) covers the knowledge and skills for screening, assessment and early diagnosis of frailty. One item was excluded at round one due to low consensus (52%). Three items were rephrased, and reached full consensus in the second round (84–100% consensus).
Domain 3 (four items) covers non-technical skills for person-centred care and collaborative working in multi-professional teams. Two items were excluded at round one due to low consensus (68% each). All items (four items) rephrased in round one, achieved full consensus in round two (88–100%) without further comments.
Domain 4 (12 items) covers the knowledge and skills to be achieved by all professionals for taking preventive actions on micro–, meso and macrolevel to prevent and tackle frailty. Interestingly, items included in domain 4 raised the highest level of discussion and, therefore, need for change during rounds one and two: one item did not reach level of significance in round one and was excluded. Six items of round one had to be rephrased. Six items had been suggested by participants for direct inclusion during round one without any rephrasing necessary. Suggestions for those items included in the second Delphi round were raised by many participants simultaneously. The core group revised the suggested phrases. All items reached full consensus in round two, with 84–96% agreement.
Discussion
There is a clear commitment by the “Science Advice for Policy by European Academies” (SAPEA) for European-wide changes in health and social care delivery based on integrated care throughout the whole life span to effectively impact on healthy lifetime [24]. Similar recommendations have been given by WHO in 2015 where “Integration” addresses longitudinal care pathways for citizens themselves as well as horizontal integration of care interventions through linkage of processes currently delivered in a fragmented way in many health care systems and health care delivery is oriented towards individualized and person-centred treatment goals [25]. This approach implies a strong alignment of professionals integrated in the care of patients at any age, particularly of importance for patients with complex care needs, such as old and vulnerable groups.
The ADVANTAGE JA aims at building a shared understanding among policy makers and stakeholders to develop a common European approach to frailty prevention. Task 8.1 (WP8) was asked to critically appraise the current evidence in the field of education/training for health professionals in the prevention of frailty across the European member states. The consortium showed the absence of evidence for the benefit of educational interventions of staff involved into the care process [3].
Based on this previous work [4, 5], it was assumed by members of the consortium of the ADVANTAGE JA that shared values, knowledge and skills would also serve the goals outlined in the SAPEA report and would actively support the quality of care for people with complex care needs across Europe. It was, therefore, the aim of the group to make use of the broad spectrum of best practice models detected throughout Europe during the work of the Joint Action and to validate content from training programs in the best practice settings and build evidence for a multi-professional European Capability Framework for the care of older citizens using a consensus approach (Table 1). This framework should then serve as common key element for further implementation of management recommendations delivered by the JA and to facilitate the translation of results delivered by the ADVANTAGE JA in EU member states. This approach has also been previously supported by the World Health Organization (WHO) [26].
Table 2 highlights that the final agreed capability framework for frailty prevention and management includes four different domains. Besides a common understanding of frailty as a concept, skills to identify frailty were included in the recommendation (Domains 1 and 2 of the framework, Table 2). The majority of capabilities, however, address person-centred, collaborative and integrated working as communication skills, leadership qualities and awareness for innovation and community development are all non-technical skills. This result of this Pan-European consensus process is aligned with strong representation of non-technical skills needed for interprofessional collaborative practice [5]. Equipping professionals with skills for goal-oriented and smooth communication pathways and adapting flat hierarchies within teams and inbetween teams around older people will build social and human bridges, supporting integrated care.
A main link for the collaborative practice in care for older people is “screening” as well as “comprehensive geriatric assessment” (CGA). Those instruments are major backbones for integration of functionality into standard medical care for older people with complex care needs [27]. Especially CGA has been proven effective for health outcomes and functionality in groups of older people in hospital setting [28]. By nature, geriatricians coordinate teams around older people and see CGA as the gold standard of their clinical management. Furthermore, geriatric medicine nowadays has proven the concept of CGA as core element of evidence for integrated complex care management of older patients [29]. By implementing CGA in different care settings for older people within the public health system, it will be possible to align integrated clinical care as well as corresponding research settings [30].
The capability framework presented and developed under the auspices of the Joint Action ADVANTAGE and EuGMS will allow definition of the specific roles of professionals involved into the process of CGA for different settings. Furthermore, this role clarification will allow standardization procedures for all care processes and give insight into efficacy and effectiveness of integrated care of older people in different settings. In a systematic review currently submitted for publication, the authors showed that there is evidence for efficacy of multi-professional team care when including doctors, nurses and physiotherapists in care teams for older people [31]. This makes the current work outstanding as only few publications in the literature currently address the effect of inclusion of different professions in the care teams, such as dieticians, social workers and others. However, many domains included in the CGA touch upon expertise of those professions not initially included in a multi-professional team and only little information is available on role modelling and responsibilities within the multi-professional care teams.
Research shows interprofessional collaboration improves patient outcomes, patient safety, and staff morale while decreasing hospital admissions, length of hospital stays, and staff turnover [32]. Most probably, this is one of the reasons why the current European Health Programme [33] includes a strong focus on integrated care, aiming to improve patient experience and outcomes of care and effectiveness of health systems. Within this concept, it is expected that involved team members must collaborate effectively to achieve sustainability of cross-sectoral complex care interventions. In this context, the framework presented here is pioneering work. It includes shared knowledge, skills and attitudes for many professions involved in the integrated care pathway for many older citizens.
The Joint Action ADVANTAGE provides a European guide on how to preserve capacity in ageing societies on a public health level. However, the multi-dimensional nature of frailty and functional decline raises the need for a holistic and multi-dimensional approach and increases the need for involvement of different stakeholders in distinct care settings. Basic knowledge but also the capability to work in synchrony with frail older peoples’ and their families’ values and goals are necessary [34]. The work presented provides the framework in which all professions around older people should be trained and may, therefore, serve as hallmark for translation of the results of the JA ADVANTAGE in many health and social care systems across Europe. The work presented here is aligned with recommendations on evidence-based management for integrated care for older people (ICOPE) in community to avoid loss of intrinsic capacity, recently launched by WHO [35]. The translation of the recommendations from ICOPE guidelines as well as the capability framework, presented in this publication, into curricula of different professions will be the next step to foster integration of the capabilities into daily practice. Ideally, interprofessional education is used for future training [36].
Developing the health and social care workforce needed for future generations of European citizens is demanding. It is important to see health workforce planning as a process that engages the main stakeholders in assessing needs for change and in devising strategies to achieve those changes. Addressing and focusing on regional and national needs implies more than producing more workers; scaling up can be achieved by improving competences, changing skills mix and by augmenting productivity. For sustainability of these developments, it will be necessary to evaluate the intervention set and to see health work force development as part of quality assurance in health care systems.
The main strength of this study is the attainment of a consensus from a broad spectrum of European stakeholders, ranging from political representatives, to experts in the field of ageing and health, academia as well as practitioners of different settings and care systems across European countries. Working in harmony between professions towards commonly shared therapeutic goals and adapting therapeutic targets in an integrated way throughout lifespan of older citizens will help to personalize care as recommended by many official bodies. The applicability of this agreed framework outside the EU is currently unclear, hypothesis generating and may represent a potential limitation of this study.
Conclusion
The study describes one of the first, if not “the first” agreed Pan-European multi-professional capability framework for frailty prevention and management developed and supported by the JA ADVANTAGE and the European Geriatric Medicine Society (EuGMS). This framework potentially offers the possibility to many European stakeholders involved in the care process of older citizens on all public health levels to integrate the capabilities outlined into curricula and foster integrated care delivery for older people across Europe.
The framework has a strong focus on person-centred, collaborative and integrated working as communication skills, leadership qualities and awareness for innovation and community development are all non- technical skills. Implementing these capabilities in curricula will be the next step. Working together in daily clinical practice but also on a transnational level and tailoring educational programs for many professions involved into older care will be the focus of the work for the incoming decade.
References
Clegg A, Young J, Iliffe S et al (2013) Frailty in elderly people. Lancet (London, England) 381:752–762. https://doi.org/10.1016/s0140-6736(12)62167-9
Rodríguez-Mañas L, García-Sánchez I, Hendry A et al (2018) Key messages for a frailty prevention and management policy in Europe from the Advantage Joint Action Consortium. J Nutr Health Aging. https://doi.org/10.1007/s12603-018-1064-y
Windhaber T, Koula ML, Ntzani E et al (2018) Educational strategies to train health care professionals across the education continuum on the process of frailty prevention and frailty management: a systematic review. Aging Clin Exp Res 30:1409–1415. https://doi.org/10.1007/s40520-018-0918-9
Schmitt M, Blue A, Aschenbrener CA et al (2011) Core competencies for interprofessional collaborative practice: reforming health care by transforming health professionals’ education. Acad Med 86:1351. https://doi.org/10.1097/acm.0b013e3182308e39
Ellis G, Sevdalis N (2019) Understanding and improving multidisciplinary team working in geriatric medicine. Age Ageing 48:498–505. https://doi.org/10.1093/ageing/afz021
Vernon W (2009) The Delphi technique: A review. International Journal of Therapy and Rehabilitation 16:69–76. https://doi.org/10.12968/ijtr.2009.16.2.38892
Roller-Wirnsberger R, Windhaber T, Koula ML (2017) Building workforce capacity on frailty prevention. ADVANTAGE joint action
Health Education England, NHS England, skills for health (2018) Frailty. A framework for core capabilities
Sunfrail Project overview (2019) http://www.sunfrail.eu/project-overview/. Accessed 10 Jan 2019
Frailty360 Frailty training for all (2019) https://frailty360.org/. Accessed 10 Jan 2019
Facet Facet (2019)https://www.eithealth.eu/facet. Accessed 10 Jan 2019
Fusion48 frailty training events. http://www.fusion48.net/frailty/frailty-training. Accessed 10 Jan 2019
The Irish longitudinal study on ageing (TILDA) National Frailty Education Programme (2019) https://tilda.tcd.ie/ppi/frailty-education/. Accessed 18 Oct 2019
St. Wilfrid’s Hospice Frailty for Healthcare Professionals (2019) https://stwh.co.uk/education/frailty-for-healthcare-professionals. Accessed 10 Jan 2019
Ministère des affaires sociales de la santé et des droits des femmes Plan national d’Action de prévention de la perte d’autonomie. https://solidarites-sante.gouv.fr/IMG/pdf/plan_national_daction_de_prevention_de_la_perte_dautonomie.pdf. Accessed 10 Jan 2019
NHS Camden Education Module – Frailty (2019) https://gps.camdenccg.nhs.uk/education-module-frailty. Accessed 10 Jan 2019
Oxford Brookes University Acute Care of the Older Person with Frailty (2019) https://www.brookes.ac.uk/courses/postgraduate/acute-care-of-the-older-person-with-frailty/. Accessed 10 Jan 2019
University of Lincoln Programme Specification. Specialist Practice Frail Older Adults for Health and Social Care https://www.lincoln.ac.uk/about/courses/nursppms_2018-19.pdf. Accessed 10 Jan 2019
European Innovation Partnership on Active and Healthy Ageing Training program for health care professionals on detecting pre-frailty and recognising the initial steps of frailty in primary care. https://ec.europa.eu/eip/ageing/commitments-tracker/a3/training-program-health-care-professionals-detecting-pre-frailty-and_en. Accessed 10 Jan 2019
Inzitari M, Pérez LM, Enfedaque MB et al (2018) Integrated primary and geriatric care for frail older adults in the community: Implementation of a complex intervention into real life. Eur J Intern Med 56:57–63. https://doi.org/10.1016/j.ejim.2018.07.022
Keele University Medical Science (Frailty and Integrated Care) https://www.keele.ac.uk/pgtcourses/medicalsciencefrailtyandintegratedcare/. Accessed 10 Jan 2019
Perssilaa The Personalised ICT Supported Service for Independent Living and Active Ageing https://perssilaa.com/. Accessed 10 Jan 2019
Anaïs Formation Dépistage de la fragilité et prévention de la dépendance à domicile https://www.anaisformation.com/360-31-ehpad-et-ch-formation-en-intra-accueil-soin-prevention-urgences-evaluation. Accessed 10 Jan 2019
SAPEA (2019) Transforming the Future of Ageing. SAPEA, Berlin. https://doi.org/10.26356/ageing
Gilbert JH, Yan J, Hoffman SJ (2010) A WHO report: framework for action on interprofessional education and collaborative practice. J Allied Health 39:196–197
World Health Organization (2016) Health workforce for ageing populations. Switzerland, Geneva
Roller-Wirnsberger R, Thurner B, Pucher C et al (2019) The clinical and therapeutic challenge of treating older patients in clinical practice. Br J Clin Pharmacol. https://doi.org/10.1111/bcp.14074
Ellis G, Whitehead MA, O’Neill D et al (2011) Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd006211.pub2
Ellis G, Gardner M, Tsiachristas A et al (2017) Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.cd006211.pub3
Pilotto A, Veronese N, Quispe Guerrero KL et al (2019) Development and validation of a self-administered multidimensional prognostic index to predict negative health outcomes in community-dwelling persons. Rejuvenation Res 22(4):299–305. https://doi.org/10.1089/rej.2018.2103
Platzer E, Singler K, Dovjak P, et al. (2019) Evidence of Inter–and multiprofessional interventions for geriatric patients: a systematic review. accepted for publication
Health Professions Network Nursing and Midwifery Office Department Human of Resources for Health of the World Health Organization (2010) Framework for Action on Interprofessional Education & Collaborative Practice. World Health Organization, Department of Human Resources for Health, Geneva, Switzerland
European Commission EU Health Programme 2014–2020. https://ec.europa.eu/health/funding/programme/2014–2020_en. Accessed 21 Oct 2019
D’Avanzo B, Shaw R, Riva S et al (2018) Correction: stakeholders’ views and experiences of care and interventions for addressing frailty and pre-frailty: a meta-synthesis of qualitative evidence. PLOS ONE 13:e0191763. https://doi.org/10.1371/journal.pone.0191763
World Health Organization (2017) Integrated care for older people: Guidelines on community-level interventions to manage declines in intrinsic capacity. World Health Organization, Geneva
Keijsers CJPW, Dreher R, Tanner S et al (2016) Interprofessional education in geriatric medicine. Eur Geriatr Med 7:306–314. https://doi.org/10.1016/j.eurger.2016.01.011
Acknowledgements
Open access funding provided by Medical University of Graz.
Funding
This work was funded by the European Commission under the umbrella of the European Union’s Health Programme (2014–2020), Grant Agreement Number 724099 and virtually supported by the Special Interest Group on Education and Training of the European Geriatric Medicine Society (EuGMS).
Author information
Authors and Affiliations
Contributions
RR-W, AL, RC, DM and MK were in charge of the scientific support of the project including all preparatory work published elsewhere. SL supported the project in terms of administrative work and helped to prepare the draft manuscript. The six persons named also formed the core group evaluating data from the feedbacks during the Delphi rounds. All other authors listed gave feedback during the process, read and approved the manuscript in its current version.
Corresponding author
Ethics declarations
Conflict of interest
This work was supported by the European Commission, Grant Agreement Number 724099. None of the authors has any other potential conflict of interest.
Statement of human and animal rights
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of article, formal consent is not required. All partners involved gave their willingness to participate in the consensus process per email.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
On behalf of the Joint Action ADVANTAGE, funded by the European Commission under the umbrella of the European Union’s Health Programme (2014–2020), Grant Agreement Number 724099 and the Special Interest Group on Education and Training of the European Geriatric Medicine Society (EuGMS).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Roller-Wirnsberger, R., Lindner, S., Liew, A. et al. European Collaborative and Interprofessional Capability Framework for Prevention and Management of Frailty—a consensus process supported by the Joint Action for Frailty Prevention (ADVANTAGE) and the European Geriatric Medicine Society (EuGMS). Aging Clin Exp Res 32, 561–570 (2020). https://doi.org/10.1007/s40520-019-01455-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01455-5