Abstract
Objective
The aim of this study was to investigate the relationship between tongue muscle quality index, which was represented as tongue muscle pressure divided by tongue muscle mass, and swallowing speed in community-dwelling older women.
Methods
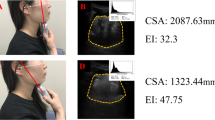
The inclusion criteria for this cross-sectional study were that participants be community-dwelling older women aged 65 years and above without dysphagia. The exclusion criteria were stroke and Parkinson’s disease that directly cause dysphagia. We measured tongue muscle thickness and maximum tongue pressure and the tongue muscle quality index, which was defined as the maximum tongue pressure divided by tongue muscle thickness. We investigated swallowing speed via a 100 ml water swallowing test. To assess the relationship between tongue muscle characteristics and swallowing speed, we performed stepwise multiple regression analysis.
Results
Ninety-three participants were enrolled in this study (mean age: 84.2 ± 4.7 years). A stepwise multiple regression analysis showed that age (β = − 0.292, p < 0.01) and tongue muscle quality index (β = 0.267, p < 0.01) were related to swallowing speed.
Conclusion
We found that tongue muscle quality index was related to swallowing speed in community-dwelling older women. According to our findings, it is possible that the tongue muscle quality index is a useful parameter for assessing swallowing speed in older women without dysphagia.


Similar content being viewed by others
References
Mulheren RW, Azola AM, Kwiatkowski S et al (2018) Swallowing changes in community-dwelling older adults. Dysphagia 33:848–856
Madhavan A, LaGorio LA, Crary MA et al (2016) Prevalence of and risk factors for dysphagia in the community dwelling elderly: a systematic review. J Nutr Health Aging 20:806–815
Baijens LW, Clavé P, Cras P et al (2016) European society for swallowing disorders—European Union geriatric medicine society white paper: oropharyngeal dysphagia as a geriatric syndrome. Clin Interv Aging 11:1403–1428
Humbert I, Robbins A (2008) Dysphagia in the elderly. J Phys Med Rehabil Clin N Am 19:853–866
Mendes AE, Nascimento L, Mansur LL et al (2015) Tongue forces and handgrip strength in normal individuals: association with swallowing. Clinics (Sao Paulo) 70:41–45
Wu MC, Chang YC, Wang TG et al (2004) Evaluating swallowing dysfunction using a 100-ml water swallowing test. Dysphagia 19:43–47
Clavé P, Shaker R (2015) Dysphagia: current reality and scope of the problem. Nat Rev Gastroenterol Hepatol 12:259–270
Robbins J, Humpal NS, Banaszynski K et al (2016) Age-related differences in pressures generated during isometric presses and swallows by healthy adults. Dysphagia 31:90–96
Tamura F, Kikutani T, Tohara T et al (2012) Tongue thickness relates to nutritional status in the elderly. Dysphagia 27:556–561
Butler SG, Stuart A, Leng X et al (2011) The relationship of aspiration status with tongue and handgrip strength in healthy older adults. J Gerontol A Biol Sci Med Sci 66:452–458
Ogawa N, Mori T, Fujishima I et al (2018) Ultrasonography to measure swallowing muscle mass and quality in older patients with sarcopenic dysphagia. J Am Med Dir Assoc 19:516–522
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Writing Group for the European working group on Sarcopenia in older people 2 (EWGSOP2), and the extended group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Aging 48:16–31
Goodpaster BH, Park SW, Harris TB et al (2006) The loss of skeletal muscle strength, mass, and quality in older adults: the health, aging and body composition study. J Gerontol A Biol Sci Med Sci 61:1059–1064
Delmonico MJ, Harris TB, Visser M et al (2009) Health, aging, and body. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr 90:1579–1585
McGregor RA, Cameron-Smith D, Poppitt SD (2014) It is not just muscle mass: a review of muscle quality, composition and metabolism during ageing as determinants of muscle function and mobility in later life. Longev Healthspan 3:9
Barbat-Artigas S, Rolland Y, Zamboni M et al (2012) How to assess functional status: a new muscle quality index. J Nutr Health Aging 16:67–77
Pinto RS, Correa CS, Radaelli R et al (2014) Short-term strength training improves muscle quality and functional capacity of elderly women. Age (Dordr) 36:365–372
Gadelha AB, Neri SGR, Nóbrega OT et al (2018) Muscle quality is associated with dynamic balance, fear of falling, and falls in older women. Exp Gerontol 104:1–6
Sakai K, Nakayama E, Tohara H et al (2017) Tongue strength is associated with grip strength and nutritional status in older adult inpatients of a rehabilitation hospital. Dysphagia 32:241–249
Buehring B, Hind J, Fidler E et al (2013) Tongue strength is associated with jumping mechanography performance and handgrip strength but not with classic functional tests in older adults. J Am Geriatr Soc 61:418–422
Suzuki M, Koyama S, Kimura Y et al (2018) Relationship between characteristics of skeletal muscle and oral function in community-dwelling older women. Arch Gerontol Geriatr 79:171–175
Chantaramanee A, Tohara H, Nakagawa K et al (2019) Association between echo intensity of the tongue and its thickness and function in elderly subjects. J Oral Rehabil 46:634–639
Tombaugh TN, McIntyre NJ (1992) The mini-mental state examination: a comprehensive review. J Am Geriatr Soc 40:922–935
Mori T, Fujishima I, Wakabayashi H et al (2017) Development, reliability, and validity of a diagnostic algorithm for sarcopenic dysphagia. JCSM Clin Rep 2:1–10
Newman AB, Haggerty CL, Goodpaster B et al (2003) Health aging and body composition research group. Strength and muscle quality in a well-functioning cohort of older adults: the health, aging and body composition study. J Am Geriatr Soc 51:323–330
Yamada M, Kimura Y, Ishiyama D et al (2017) Differential characteristics of skeletal muscle in community-dwelling older adults. J Am Med Dir Assoc 18:807.e9–807.e16
Wakabayashi H, Kayashita J (2014) Translation, reliability, and validity of the Japanese version of the 10-item Eating Assessment Tool (EAT-10) for the screening of dysphagia. JJSPEN 29:871–876 (in Japanese)
Watanabe Y, Hirano H, Arai H et al (2017) Relationship between frailty and oral function in community-dwelling elderly adults. J Am Geriatr Soc 65:66–76
Tanaka T, Takahashi K, Hirano H et al (2018) Oral frailty as a risk factor for physical frailty and mortality in community-dwelling elderly. J Gerontol A Biol Sci Med Sci 73:1661–1667
Posner BM, Jette AM, Smith KW et al (1993) Nutrition and health risks in the elderly: the nutrition screening initiative. Am J Public Health 83:972–978
Sugiura Y, Tanimoto Y, Imbe A et al (2016) Association between functional capacity decline and nutritional status based on the nutrition screening initiative checklist: a 2-year cohort study of Japanese community-dwelling elderly. PLoS ONE 11:e0166037
Fujimoto K, Honda T, Suito H et al (2018) Tongue thickness and its clinical significance. J Oral Health Biosci 31:32–38
Furuya H, Tamura F, Yoshida M et al (2016) Tongue muscle mass and strength relate to whole-body muscle in the community-dwelling elderly. J Jpn Assoc Oral Rehabil 29:1–9 (in Japanese)
Miller JL, Watkin KL, Chen MF (2002) Muscle, adipose, and connective tissue variations in intrinsic musculature of the adult human tongue. J Speech Lang Hear Res 45:51–65
Fujishima I, Fujiu-Kurachi M, Arai H et al (2019) Sarcopenia and dysphagia: position paper by four professional organizations. Geriatr Gerontol Int. https://doi.org/10.1111/ggi.13591
McKenna Victoria S, Zhang Bin, Haines Morgan B et al (2017) A systematic review of isometric lingual strength-training programs in adults with and without dysphagia. Am J Speech Lang Pathol 26:524–539
Nicosia MA, Hind JA, Roecker EB et al (2000) Age effects on the temporal evolution of isometric and swallowing pressure. J Gerontol A Biol Sci Med Sci 55:M634–M640
Steele CM (2013) Optimal approaches for measuring tongue-pressure functional reserve. J Aging Res 2013:542909
Todd JT, Lintzenich CR, Butler SG (2013) Isometric and swallowing tongue strength in healthy adults. Laryngoscope 123:2469–2473
Robbins J, Humpal NS, Banaszynski K et al (2016) Age-related differences in pressures generated during isometric presses and swallows by healthy adults. Dysphagia 31:90–96
Hughes TA, Wiles CM (1996) Clinical measurement of swallowing in health and in neurogenic dysphagia. QJM 89:109–116
Nathadwarawala KM, Nicklin J, Wiles CM (1992) A timed test of swallowing capacity for neurological patients. J Neurol Neurosurg Psychiatry 55:822–825
Patterson JM, McColl E, Carding PN et al (2009) Swallowing performance in patients with head and neck cancer: a simple clinical test. Oral Oncol 45:904–907
Acknowledgements
The authors acknowledge Mr. Buichi Tanaka and Mr. Yasuhito Obuchi for their contributions to the data collection.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest statement
The authors have no conflict of interest.
Statement of human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Suzuki, M., Koyama, S., Kimura, Y. et al. Relationship between tongue muscle quality and swallowing speed in community-dwelling older women. Aging Clin Exp Res 32, 2073–2079 (2020). https://doi.org/10.1007/s40520-019-01388-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01388-z