Abstract
Background
The growing “process” of burnout impair performance and quality of professional services, with consequences for physicians, healthcare care organization, and patient’s outcomes.
Aims
We aim to evaluate which strategy of intervention, individual or organization directed, is more effective to reduce physician burnout and to provide management suggestions in terms of actual organizational strategies and intensity leading to reductions in physician burnout.
Methods
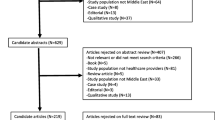
The meta analysis was conducted according to the PRISMA guidelines. We included physicians of any specialty in the primary, secondary, or intensive care setting, including residents and fellows. Eligible interventions were any intervention designed to relieve stress and/or improve the performance of physicians and reported burnout outcomes, including physician-directed interventions and organization-directed interventions. The electronic search strategy applied standard filters for identification of the different studies. Databases searched were the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library), MEDLINE (from inception to September 2018), and EMBASE (from beginning to September 2018). Meta analysis was performed with mixed random effect using DerSimonian and Laird method. The standardized mean difference (SMD) and 95% CI for each outcome were separately calculated for each trial pooling data when needed, according to an intention-to-treat principle.
Results
Pooled interventions were associated with small significant reductions in burnout (SMD = − 0.289; 95% CI, − 0.419 to − 0.159; I2 = 29%) (Fig. 2). Organization-directed interventions were associated with a medium reduction in burnout score (SMD = − 0.446; 95% CI, − 0.619 to − 0.274; I2 = 8%) while physician-directed interventions were associated with a moderate reduction in burnout score (SMD = − 0.178; 95% CI, − 0.322 to − 0.035; I2 = 11%).
Discussion
This systematic review and meta-analysis showed that (1) organization-directed interventions were associated with moderate reduction in burnout score, (2) physician-directed interventions were associated with small reduction in burnout score, (3) organization-directed interventions reduced more the depersonalization than physician-directed interventions, (4) organization-directed interventions were related to a more improvement of the personal accomplishment than physician-directed interventions.
Conclusions
This meta analysis found that physicians could gain important benefits from interventions to reduce burnout, especially from organizational strategies, by viewing burnout rooted in issues related to the working environment and organizational culture.







Similar content being viewed by others
References
Freudenberger HJ (1974) Staff Burn-Out. J Soc Issues 30:159–165
Vargas M, Spinelli G, De Simone S et al (2018) Il Burn-out. In: Marinangeli F, Ciccone A, Ranieri MV (eds) Rischi Medico-legali in Rianimazione e Terapia Intensiva. Responsabilità Professionale in una Sanità che cambia. Momento Medico, Salerno, pp 73–76
De Simone S (2014) A conceptual framework for the organizational analysis in health care contexts. Int J Humanit Soc Sci 4:46–52
De Simone S (2015) Wellbeing at work: a survey on perception of health care workers. Rivista Internazionale di Scienze Sociali 4:412–495
Maslach C, Schaufeli WB, Leiter MP (2001) Job burnout. Annu Rev Psychol 52:397–422
Maslach C, Jackson SE (1981) The measurement of experienced burnout. J Organ Behav 2:99–113
Wallace JE, Lemaire JB, Ghali WA (2009) Physician wellness: a missing quality indicator. Lancet 374:1714–1721
Awa WL, Plaumann M, Walter U (2010) Burnout prevention: a review of intervention programs. Patient Educ Couns 78:184–190
Dyrbye LN, Shanafelt TD (2011) Physician burnout: a potential threat to successful health care reform. JAMA 305:2009–2010
Dewa CS, Loong D, Bonato S et al (2014) How does burnout affect physician productivity? a systematic literature review. BMC Health Serv Res 14:325
Shanafelt TD, Mungo M, Schmitgen J et al (2016) Longitudinal study evaluating the association between physician burnout and changes in professional work effort. Mayo Clin Proc 91:422–431
Shanafelt TD, Balch CM, Bechamps G et al (2010) Burnout and medical errors among American surgeons. Ann Surg 251:995–1000
Bakker AB, Demerouti E, Euwema MC (2005) Job resources buffer the impact of job demands on burnout. J Occup Health Psychol 10:170–180
Bakker AB, Demerouti E, Verbeke W (2004) Using the job demands resources model to predict burnout and performance. Hum Resour Manag 43:83–104
Kalani SD, Azadfallah P, Oreyzi H et al (2018) Interventions for physician Burnout: a systematic review of systematic reviews. Int J Prev Med 9:1–12
Panagioti M, Panagopoulou E, Bower P et al (2017) Controlled interventions to reduce burnout in physicians: a systematic review and meta-analysis. JAMA Intern Med 177:195–205
Higgins JP, Altman DG, Gotzschge PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ 343:d5928
Peters JL, Sutton AJ, Jones DR et al (2006) Comparison of two methods to detect publication bias in meta-analysis. JAMA 295:676–680
Moher D, Liberati A, Tetzlaff J, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097
Ali NA, Hammersley J, Hoffmann SP et al (2011) Midwest Critical Care Consortium. Continuity of care in intensive care units: a cluster-randomized trial of intensives staffing. Am J Respir Crit Care Med 184:803–808
Amutio A, Martinez-Taboada C, Delgado LC et al (2015) Acceptability and effectiveness of a long-term educational intervention to reduce physicians’ stress-related conditions. J Contin Educ Health Prof 35:255–260
Asuero AM, Queralt JM, Pujol-Ribera E et al (2014) Effectiveness of a mindfulness education program in primary health care professionals: a pragmatic controlled trial. J Contin Educ Health Prof 34:4–12
Bragard I, Etienne AM, Merckaert I et al (2010) Efficacy of a communication and stress management training on medical residents’ self-efficacy, stress to communicate and burnout. J Health Psychol 15:1075–1081
Butow P, Brown R, Aldridge J et al (2015) Can consultation skills training change doctors’ behaviour to increase involvement of patients in making decisions about standard treatment and clinical trials: a randomized controlled trial. Health Expect 18:2570–2583
Butow P, Cockburn J, Girgis A et al (2008) CUES Team. Increasing oncologists’ skills in eliciting and responding to emotional cues: evaluation of a communication skills training program. Psychooncology 17:209–218
Garland A, Roberts D, Graff L (2012) Twenty-four-hour intensivist presence: a pilot study of effects on intensive care unit patients, families, doctors, and nurses. Am J Respir Crit Care Med 185:738–743
Gunasingam N, Burns K, Edwards J et al (2015) Reducing stress and burnout in junior doctors: the impact of debriefing sessions. Postgrad Med J 91:182–187
Linzer M, Poplau S, Grossman E et al (2015) A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: results from the Healthy Work Place (HWP) study. J Gen Intern Med 30:1105–1111
Lucas BP, Trick WE, Evans AT et al (2012) Effects of 2- vs 4-week attending physician inpatient rotations on unplanned patient revisits, evaluations by trainees, and attending physician burnout: a randomized trial. JAMA 308:2199–2207
Margalit APA, Glick SM, Benbassat J et al (2005) Promoting a biopsychosocial orientation in family practice: effect of two teaching programs on the knowledge and attitudes of practising primary care physicians. Med Teach 27:613–618
Martins AE, Davenport MC, Del Valle MP et al (2011) Impact of a brief intervention on the burnout levels of pediatric residents. J Pediatr 87:493–498
Milstein JM, Raingruber BJ, Bennett SH et al (2009) Burnout assessment in house officers: evaluation of an intervention to reduce stress. Med Teach 3:338–341
Parshuram CS, Amaral ACKB, Ferguson ND et al (2015) Canadian Critical Care Trials Group. Patient safety, resident well-being and continuity of care with different resident duty schedules in the intensive care unit: a randomized trial. CMAJ 187:321–329
Ripp JA, Bellini L, Fallar R et al (2015) The impact of duty hours restrictions on job burnout in internal medicine residents: a three-institution comparison study. Acad Med 90:494–499
Shea JA, Bellini LM, Dinges DF et al (2014) Impact of protected sleep period for internal medicine interns on overnight call on depression, burnout, and empathy. J Grad Med Educ 6:256–263
Verweij H, Waumans RC, Smeijers D et al (2016) Mindfulness-based stress reduction for GPs: results of a controlled mixed methods pilot study in Dutch primary care. Br J Gen Pract 66:99–105
Weight CJ, Sellon JL, Lessard-Anderson CR et al (2013) Physical activity, quality of life, and burnout among physician trainees: the effect of a team-based, incentivized exercise program. Mayo Clin Proc 88:1435–1442
West CP, Dyrbye LN, Rabatin JT et al (2014) Intervention to promote physician well-being, job satisfaction, and professionalism: a randomized clinical trial. JAMA Intern Med 174:527–533
Ireland MJ, Clough BC, Gill K et al (2017) A randomized controlled trial of mindfulness to reduce stress and burnout among intern medical practitioners. Med Teach. https://doi.org/10.1080/0142159X.2017.1294749
De Simone S (2013) Organizational climate and organizational behaviour, in XIV Workshop dei docenti e dei Ricercatori di Organizzazione Aziendale Organizing in turbulent times: the challenges ahead. Sapienza, Rome, pp 30–31
De Simone S (2016) Leadership behaviors in organizations. Int J Bus Soc Sci 7(4):59–64
Korczak D, Huber B, Kister C (2010) Differential diagnostic of the burnout syndrome. GMS Health Technol Assess 6:1–9
Funding
This work was supported by the National Research Council of Italy (CNR), Research Project “Aging: molecular and technological innovations for improving the health of the elderly population” (Prot. MIUR 2867 25.11.2011)”
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
Not required since this a systematic review.
Human and animal rights
All procedures performed in the included studies involving human participants were in accordance with the ethical standard.
Informed consent
Not required since this a systematic review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
De Simone, S., Vargas, M. & Servillo, G. Organizational strategies to reduce physician burnout: a systematic review and meta-analysis. Aging Clin Exp Res 33, 883–894 (2021). https://doi.org/10.1007/s40520-019-01368-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01368-3