Abstract
Introduction
Despite the use of the new generation P2Y12 inhibitors (Ticagrelor and Prasugrel) with aspirin is the recommended therapy in acute NSTE-ACS patients, their current use in clinical practice remains quite low and might be related, among several variables, with increased comorbidity burden. We aimed to assess the prevalence of these treatments and whether their use could be associated with comorbidity.
Method
A multicentric prospective registry was conducted at 8 Cardiac Intensive Care Units (October 2017–April 2018) in patients admitted with non ST elevation myocardial infarction. Antithrombotic treatment was recorded and the comorbidity risk was assessed using the Charlson Comorbidity Index. We created a multivariate model to identify the independent predictors of the use of new inhibitors of P2Y12.
Results
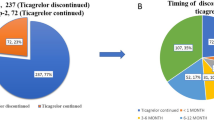
A total of 629 patients were included, median age 67 years, 23.2% women, 359 patients (57.1%) treated with clopidogrel and 40.6% with new P2Y12 inhibitors: ticagrelor (228 patients, 36.2%) and prasugrel (30 patients, 4.8%). Among the patients with very high comorbidity (Charlson Score > 6) clopidogrel was the drug of choice (82.6%), meanwhile in patients with low comorbility (Charlson Score 0–1) was the ticagrelor or prasugrel (63.6%). Independent predictors of the use of ticagrelor or prasugrel were a low Charlson Comorbidity Index, a low CRUSADE score and the absence of prior bleeding.
Conclusion
Antiplatelet treatment with Ticagrelor or Pasugrel was low in patients admitted with NSTE-ACS. Comorbidity calculated with Charlson Comorbidity Index was a powerful predictor of the use of new generation P2Y12 inhibitors in this population.

Similar content being viewed by others
Abbreviations
- NSTE-ACS:
-
Non-ST-segment elevation acute coronary syndrome
- NAAs:
-
P2Y12-inhibitor antiplatelet agents (ticagrelor and prasugrel)
- CICUs:
-
Cardiac intensive care units
References
Yusuf S, Zhao F, Mehta SR et al (2001) Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 345:494–502
Steinhubl SR, Berger PB, Mann JT et al (2002) Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial. JAMA 288:2411–2420
Matetzky S, Shenkman B, Guetta V et al (2004) Clopidogrel resistance is associated with increased risk of recurrent atherothrombotic events in patients with acute myocardial infarction. Circulation 109:3171–3175
Wiviott SD, Braunwald E, McCabe CH et al (2007) Prasugrel versus Clopidogrel in Patients with Acute Coronary Syndromes. N Engl J Med 357:2001–2015
Wallentin L, Becker RC, Budaj A et al (2009) Ticagrelor versus Clopidogrel in Patients with Acute Coronary Syndromes. N Engl J Med 361:1045–1057
Neumann F-J, Sousa-Uva M, Ahlsson A et al (2018) ESC/EACTS Guidelines on myocardial revascularization. EuroIntervention 14:1435–1534
Ferlini M, Musumeci G, Grieco N et al (2018) The paradox of clopidogrel use in patients with acute coronary syndromes and diabetes insight from the diabetes: and acute coronary syndrome registry. Coron Artery Dis 29:309–315
Almendro-Delia M, García-Alcántara Á, de la Torre-Prados MV et al (2017) Safety and efficacy of prasugrel and ticagrelor in acute coronary syndrome. Results of a « real world » multicenter registry. Rev Espanola Cardiol Engl Ed 70:952–959
Sachdev M, Sun JL, Tsiatis AA et al (2004) The prognostic importance of comorbidity for mortality in patients with stable coronary artery disease. J Am Coll Cardiol 43:576–582
Chirinos JA, Veerani A, Zambrano JP et al (2007) Evaluation of comorbidity scores to predict all-cause mortality in patients with established coronary artery disease. Int J Cardiol 117:97–102
Fassa A-A, Urban P, Radovanovic D et al (2010) Impact of comorbidities on clinical presentation, management and outcome of patients with acute coronary syndrome. Cardiovasc Med 13:155–161
Radovanovic D, Seifert B, Urban P et al (2014) Validity of charlson comorbidity index in patients hospitalised with acute coronary syndrome. Insights from the nationwide amis plus registry 2002–2012. Heart Br Card Soc. 100:288–294
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 40:373–383
Valgimigli M, Bueno H, Byrne RA et al (2018) 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTSThe Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 39:213–260
Blin P, Dureau-Pournin C, Benichou J et al (2018) Secondary prevention of acute coronary events with antiplatelet agents (SPACE-AA): one-year real-world effectiveness and safety cohort study in the French nationwide claims database. Atherosclerosis 281:98–106
Alexopoulos D, Xanthopoulou I, Deftereos S et al (2016) Contemporary antiplatelet treatment in acute coronary syndrome patients undergoing percutaneous coronary intervention: 1-year outcomes from the GReek AntiPlatElet (GRAPE) Registry. J Thromb Haemost JTH 14:1146–1154
Beigel R, Iakobishvili Z, Shlomo N et al (2017) Real-World Use of Novel P2Y12 Inhibitors in Patients with Acute Myocardial Infarction: a Treatment Paradox. Cardiology 136:21–28
Ariza-Solé A, Sánchez-Salado JC, Lorente V et al (2014) Is it possible to separate ischemic and bleeding risk in patients with non-ST segment elevation acute coronary syndromes? Int J Cardiol 171:448–450
Lorente V, Ariza-Solé A, Jacob J et al (2019) Criteria for admitting elderly patients with acute coronary syndrome to critical care units from Spanish hospital emergency departments: a LONGEVO-SCA cohort study. Emerg Rev Soc Espanola Med Emerg 31:154–160
Subherwal S, Bach RG, Chen AY et al (2009) Baseline risk of major bleeding in non-ST-segment-elevation myocardial infarction: the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA Guidelines) Bleeding Score. Circulation 119:1873–1882
Costa F, van Klaveren D, James S et al (2017) Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet 389:1025–1034
Baber U, Mehran R, Giustino G et al (2016) Coronary Thrombosis and Major Bleeding After PCI With Drug-Eluting Stents: risk Scores From PARIS. J Am Coll Cardiol 67:2224–2234
Ariza-Solé A, Formiga F, Lorente V et al (2014) Efficacy of bleeding risk scores in elderly patients with acute coronary syndromes. Rev Espanola Cardiol Engl Ed 67:463–470
Alonso Salinas GL, Sanmartín Fernández M et al (2016) Frailty predicts major bleeding within 30 days in elderly patients with Acute Coronary Syndrome. Int J Cardiol 222:590–593
Spencer FA, Moscucci M, Granger CB et al (2007) Does comorbidity account for the excess mortality in patients with major bleeding in acute myocardial infarction? Circulation 116:2793–2801
Montalescot G, Bolognese L, Dudek D et al (2013) Pretreatment with prasugrel in non-ST-segment elevation acute coronary syndromes. N Engl J Med 369:999–1010
Ariza-Solé A, Formiga F, Bardají A et al (2018) Clinical characteristics and prognosis of very elderly patients with acute coronary syndrome treated with ticagrelor: insights from the LONGEVO-SCA Registry. Rev Espanola Cardiol Engl Ed. 72:263–266
Raposeiras-Roubín S, Faxén J, Íñiguez-Romo A et al (2018) Development and external validation of a post-discharge bleeding risk score in patients with acute coronary syndrome: the BleeMACS score. Int J Cardiol 254:10–15
Sim DS, Jeong MH, Kim HS et al (2018) Utility of GRACE and ACUITY-HORIZONS risk scores to guide dual antiplatelet therapy in Korean patients with acute myocardial infarction undergoing drug-eluting stenting. J Cardiol 72:411–419
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Statement of human and animal rights
Authors declare all the procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent to participate in the study was obtained from participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aboal, J., Llaó, I., García García, C. et al. Comorbidity and low use of new antiplatelets in acute coronary syndrome. Aging Clin Exp Res 32, 1525–1531 (2020). https://doi.org/10.1007/s40520-019-01348-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01348-7