Abstract
Background
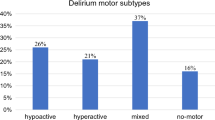
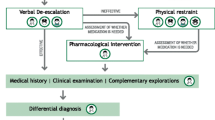
The management of delirium among older in-hospital patients is a challenge, leading to worse outcomes, including death. Specifically, psychomotor agitation, one of the main characteristics of hyperactive delirium, requires a significant amount of medical and nursing surveillance. However, despite its relevance, to date incidence and/or prevalence of psychomotor agitation, its predictors and outcomes have not been studied among Italian older patients admitted in medical units.
Aims
To describe the incidence and the prevalence of psychomotor agitation among patients aged > 65 years admitted to medical units and identify predictors at the individual, nursing care and hospital levels.
Methods
A longitudinal multicentre study was conducted involving 12 medical units in 12 northern Italian hospitals. Descriptive, bivariate and multivariate logistic regression analyses were performed.
Results
Among the 1464 patients included in the study, two hundred (13.6%) have manifested episode(s), with an average of 3.46/patient (95% confidence of interval [CI] 2.73–4.18). In 108 (54.0%) patients, episode(s) were present also in the week prior to hospitalisation: therefore, in-hospital-acquired psychomotor agitation was reported in 92 patients (46%). The multivariate logistic regression analysis explained the 25.4% of the variance and identified the following variables as psychomotor agitation predictors: the risk of falls (relative risk [RR] 1.314, 95% CI 1.218–1.417), the amount of missed nursing care (RR 1.078, 95% CI 1.037–1.12) and the patient’s age (RR 1.018, 95% CI 1.002–1.034). Factors preventing the occurrence of episode(s) were: the amount of care received from graduated nurses (RR 0.978; 95% CI 0.965–0.992) and the lower functional dependence at admission (RR 0.987, 95% CI 0.977–0.997).
Conclusions
A considerable number of elderly patients admitted in medical units develop psychomotor agitation; its predictors need to be identified early to inform decisions regarding the personal care needed to prevent its occurrence, especially by acting on modifiable factors, such as the risk of falls, missed nursing care and functional dependence.
Similar content being viewed by others
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (DSM-5), 5th edn. American Psychiatric Association Publishing, Arlington
Watt D, Budding DE, Koziol LF (2013) Delirium. In: Noggle CA, Dean RS (eds) The neuropsychology of psychopathology. Springer, New York, pp 425–440
Siddiqi N, House A, Holmes J (2006) Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing 35:350–364
Ryan DJ, O’Regan NA, Caoimh RÓ et al (2013) Delirium in an adult acute hospital population: predictors, prevalence and detection. BMJ Open 3:e001772
Witlox J, Eurelings LS, de Jonghe JF et al (2010) Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA 304:443–451
Bail K, Goss J, Draper B et al (2015) The cost of hospital-acquired complications for older people with and without dementia; a retrospective cohort study. BMC Health Serv Res 15:91
Saxena S, Lawley D (2009) Delirium in the elderly: a clinical review. Postgrad Med J 85:405–413
Liptzin B, Levkoff SE (1992) An empirical study of delirium subtypes. Br J Psychiatry 161:843–845
O’Keeffe ST, Lavan JN (1999) Clinical significance of the delirium subtypes in older people. Age Ageing 26:115–119
Avelino-Silva TJ, Campora F, Curiati JAE et al (2018) Prognostic effects of delirium motor subtypes in hospitalized older adults: a prospective cohort study. PLoS ONE 13:e0191092
Weinrebe W, Johannsdottir E, Karaman M et al (2016) What does delirium cost? An economic evaluation of hyperactive delirium. Z Gerontol Geriatr 49:52–58
Palese A, Cuel M, Zanella P et al (2013) Nursing care received by older patients in Italian medical units: findings from an explorative study. Aging Clin Exp Res 25:707–710
Aldecoa C, Bettelli G, Bilotta F et al (2017) European society of anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol 34:192–214
Barr J, Fraser GL, Puntillo K et al (2013) Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med 41:263–306
Riker RR, Fraser GL (2013) The new practice guidelines for pain, agitation, and delirium. Am J Crit Care 22:153–157
Davis D, Searle SD, Tsui A (2019) The Scottish Intercollegiate Guidelines Network: risk reduction and management of delirium. Age Ageing. https://doi.org/10.1093/ageing/afz036
Solberg LM, Plummer CE, May KN et al (2013) A quality improvement program to increase nurses’ detection of delirium on an acute medical unit. Geriatr Nurs 34:75–79
Bauernfreund Y, Butler M, Ragavan S et al (2018) TIME to think about delirium: improving detection and management on the acute medical unit. BMJ Open Qual 7:e000200
McCusker J, Cole M, Dendukuri N (2001) Delirium in older medical inpatients and subsequent cognitive and functional status: a prospective study. CMAJ 165:575–583
Ahmed S, Leurent B, Sampson EL (2014) Risk factors for incident delirium among older people in acute hospital medical units: a systematic review and meta-analysis. Age Ageing 43:326–333
Inouye SK, Westendorp RG, Saczynski JS (2014) Delirium in elderly people. Lancet 383:911–922
Bellelli G, Morandi A, Di Santo SG et al (2016) “Delirium Day”: a nationwide point prevalence study of delirium in older hospitalized patients using an easy standardized diagnostic tool. BMC Med 14:106
Fortini A, Morettini A, Tavernese G et al (2014) Delirium in elderly patients hospitalized in internal medicine wards. Intern Emerg Med 9:435–441
Goldberg A, Straus SE, Hamid JS, Wong CL (2015) Room transfers and the risk of delirium incidence amongst hospitalized elderly medical patients: a case-control study. BMC Geriatr 15:69
Inouye SK, Bogardus ST Jr, Charpentier PA et al (1999) A multicomponent intervention to prevent delirium in hospitalized older patients. N Engl J Med 340:669–676
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel Index. Md State Med J 14:61–65
Conley D, Schultz AA, Selvin R (1999) The challenge of predicting patients at risk for falling: development of the Conley Scale. Medsurg Nurs 8:348–354
Bergstrom N, Braden BJ, Laguzza A et al (1987) The Braden Scale for predicting pressure sore risk. Nurs Res 36:205–210
Kalisch BJ, Williams RA (2009) Development and psychometric testing of a tool to measure missed nursing care. J Nurs Adm 39:211–219
Sist L, Contini C, Bandini A et al (2017) MISSCARE survey—Italian version: findings from an Italian validation study. Ig Sanita Pubbl 73:29–45
Juma S, Taabazuing MM, Montero-Odasso M (2016) Clinical frailty scale in an acute medicine unit: a simple tool that predicts length of stay. Can Geriatr J 19:34–39
Oo M, Tencheva A, Khalid N et al (2013) Assessing frailty in acute medical admission of elderly patients. J R Coll Physicians Edinb 43:301–308
Kim H, Chung S, Joo YH et al (2016) The major risk factors for delirium in a clinical setting. Neuropsychiatr Dis Treat 12:1787–1793
Evans SJ, Sayers M, Mitnitski A, Rockwood K (2014) The risk of adverse outcomes in hospitalized older patients in relation to a frailty index based on a comprehensive geriatric assessment. Age Ageing 43:127–132
Martinez JA, Belastegui A, Basabe I et al (2012) Derivation and validation of a clinical prediction rule for delirium in patients admitted to a medical ward: an observational study. BMJ Open 2:e001599
Carrasco MP, Villarroel L, Andrade M et al (2014) Development and validation of a delirium predictive score in older people. Age Ageing 43:346–351
Newman MW, O’Dwyer LC, Rosenthal L (2015) Predicting delirium: a review of risk-stratification models. Gen Hosp Psychiatry 37:408–413
Ranhoff AH, Rozzini R, Sabatini T et al (2006) Delirium in a sub-intensive care unit for the elderly: occurrence and risk factors. Aging Clin Exp Res 18:440–445
Ford AH (2016) Preventing delirium in dementia: managing risk factors. Maturitas 92:35–40
Morichi V, Fedecostante M, Morandi A (2018) A point prevalence study of delirium in Italian nursing homes. Dement Geriatr Cogn Disord 46:27–41
van Velthuijsen EL, Zwakhalen SMG, Mulder WJ et al (2018) Detection and management of hyperactive and hypoactive delirium in older patients during hospitalization: a retrospective cohort study evaluating daily practice. Int J Geriatr Psychiatry 33:1521–1529
Freeman S, Hallett C, McHugh G (2016) Physical restraint: experiences, attitudes and opinions of adult intensive care unit nurses. Nurs Crit Care 21:78–87
Lee EA, Gibbs NE, Fahey L et al (2013) Making hospitals safer for older adults: updating quality metrics by understanding hospital-acquired delirium and its link to falls. Perm J 17:32–36
Guthrie PF, Rayborn S, Butcher HK (2018) Evidence-based practice guideline: delirium. J Gerontol Nurs 44:14–24
Pendlebury ST, Lovett N, Smith SC et al (2016) Delirium risk stratification in consecutive unselected admissions to acute medicine: validation of externally derived risk scores. Age Ageing 45:60–65
Leslie DL, Marcantonio ER, Zhang Y et al (2008) One-year health care costs associated with delirium in the elderly population. Arch Intern Med 168:27–32
Leslie DL, Inouye SK (2011) The importance of delirium: economic and societal costs. J Am Geriatr Soc 59:S241–S243
Lakatos BE, Capasso V, Mitchell MT et al (2009) Falls in the general hospital: association with delirium, advanced age, and specific surgical procedures. Psychosomatics 50:218–226
Hshieh TT, Yue J, Oh E et al (2015) Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med 175:512–520
Faught DD (2014) Delirium: the nurse’s role in prevention, diagnosis, and treatment. Medsurg Nurs 23:301–305
Öztürk Birge A, Bedük T (2018) The relationship of delirium and risk factors for cardiology intensive care unit patients with the nursing workload. J Clin Nurs 27:2109–2119
Queijo AF, Martins RS, Andolhe R et al (2013) Nursing workload in neurological intensive care units: cross-sectional study. Intensive Crit Care Nurs 29:112–116
Palese A, Bassi E, Tommasini C et al (2018) Missed nursing care and italian nursing practice: preliminary finding of a consensus conference. Assist Inferm Ric 37:164–171
Baker ND, Taggart HM, Nivens A et al (2015) Delirium: why are nurses confused? Medsurg Nurs 24:15–22
Fero LJ, Witsberger CM, Wesmiller SW et al (2009) Critical thinking ability of new graduate and experienced nurses. J Adv Nurs 65:139–148
Voyer P, Richard S, Doucet L et al (2008) Detection of delirium by nurses among long-term care residents with dementia. BMC Nurs 7:4
Meagher DJ, O’Hanlon D, O’Mahony E et al (2000) Relationship between symptoms and motoric subtype of delirium. J Neuropsychiatry Clin Neurosci 12:51–56
Adamis D, Devaney A, Shanahan E, McCarthy G, Meagher D (2015) Defining ‘recovery’ for delirium research: a systematic review. Age Ageing 2:318–321
Acknowledgements
ESAMED Team: Annamaria Guarnier, Paolo Barelli, Paola Zambiasi, Elisabetta Allegrini, Letizia Bazoli, Paola Casson, Meri Marin, Marisa Padovan, Michele Picogna, Patrizia Taddia, Daniele Salmaso, Paolo Chiari, Tiziana Frison, Oliva Marognolli, Federica Canzan, Elisa Ambrosi, Luisa Saiani.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that they have no conflict of interest.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Ethical statement
An appropriate approval from the Ethical Committee of the Coordinator Centre (Ospedale of Verona, Italy) has been obtained.
Informed consent
The written informed consent was also the study or collected from all individual participants included in from their reference caregiver.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mansutti, I., Venturini, M., Palese, A. et al. Episodes of psychomotor agitation among medical patients: findings from a longitudinal multicentre study. Aging Clin Exp Res 32, 1101–1110 (2020). https://doi.org/10.1007/s40520-019-01293-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01293-5