Abstract
Background
It has been suggested that a balanced nutritional intake may be useful in preventing or even reversing sarcopenia.
Aim
To describe cross-sectional associations between dietary nutrient intake and sarcopenia.
Methods
Subjects recruited from the SarcoPhAge study population completed a food frequency questionnaire. The micronutrient and macronutrient intake was evaluated in both sarcopenic and non-sarcopenic participants. The Nutritional Belgian Recommendations of 2016 were used, i.e., adequate intake and estimated average requirement (EAR). For micronutrients, the prevalence of insufficient intake was estimated as the proportion of subjects whose intake was below the EAR.
Results
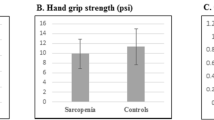
A total of 331 subjects (mean age of 74.8 ± 5.9 years, 58.9% women) had complete data and were included in this study. Among them, 51 were diagnosed with sarcopenia (15.4%). In the fully adjusted model, analyses revealed that sarcopenic subjects consumed significantly lower amounts of two macronutrients (proteins, lipids) and five micronutrients (potassium, magnesium, phosphorus, iron, and vitamin K) than non-sarcopenic subjects (all p values < 0.005). A significantly increased prevalence of insufficiency was found for sarcopenic subjects compared to non-sarcopenic subjects for potassium, magnesium, iron, calcium and vitamins E and C (all p values < 0.005). The prevalence of sarcopenic subjects who were also below the Nutritional Belgian Recommendations for protein and lipids was significantly higher than that of non-sarcopenic subjects.
Discussion and conclusions
Sarcopenic subjects seem to consume significantly reduced amounts of many micronutrients and macronutrients compared to non-sarcopenic subjects. These results suggest that a poorly balanced diet may be associated with sarcopenia and poor musculoskeletal health, although prospective studies are needed to confirm these findings.

Similar content being viewed by others
References
Cruz-Jentoft AJ, Baeyens JP, Bauer JM et al (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on sarcopenia in older people. Age Ageing 39:412–423. https://doi.org/10.1093/ageing/afq034
Studenski SA, Peters KW, Alley DE et al (2014) The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci 69:547–558. https://doi.org/10.1093/gerona/glu010
Cesari M, Fielding RA, Pahor M et al (2012) Biomarkers of sarcopenia in clinical trials-recommendations from the International Working Group on Sarcopenia. J Cachexia Sarcopenia Muscle 3:181–190. https://doi.org/10.1007/s13539-012-0078-2
Cruz-Jentoft AJ, Bahat G, Bauer J et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 48:16–31. https://doi.org/10.1093/ageing/afy169
Cao L, Morley JE, Rosenberg H et al (2016) sarcopenia is recognized as an independent condition by an international classification of disease, tenth revision, clinical modification (ICD-10-CM) code. J Am Med Dir Assoc 17:675–677. https://doi.org/10.1016/j.jamda.2016.06.001
Cruz-Jentoft AJ, Landi F, Schneider SM et al (2014) Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the international sarcopenia initiative (EWGSOP and IWGS). Age Ageing 43:748–759. https://doi.org/10.1093/ageing/afu115
Beaudart C, Rizzoli R, Bruyère O et al (2014) Sarcopenia: burden and challenges for public health. Arch Public Health. https://doi.org/10.1186/2049-3258-72-45
Beaudart C, Zaaria M, Pasleau F et al (2017) Health outcomes of sarcopenia: a systematic review and meta-analysis. PLoS One. https://doi.org/10.1371/journal.pone.0169548
Visser M, Schaap LA (2011) Consequences of sarcopenia. Clin Geriatr Med 27:387–399. https://doi.org/10.1016/j.cger.2011.03.006
Zhao Y, Zhang Y, Hao Q et al (2019) Sarcopenia and hospital-related outcomes in the old people: a systematic review and meta-analysis. Aging Clin Exp Res 31:5–14. https://doi.org/10.1007/s40520-018-0931-z
Nieuwenhuizen WF, Weenen H, Rigby P, Hetherington MM (2010) Older adults and patients in need of nutritional support: review of current treatment options and factors influencing nutritional intake. Clin Nutr 29:160–169. https://doi.org/10.1016/j.clnu.2009.09.003
Malafarina V, Uriz-Otano F, Gil-Guerrero L, Iniesta R (2013) The anorexia of ageing: physiopathology, prevalence, associated comorbidity and mortality. A systematic review. Maturitas 74:293–302. https://doi.org/10.1016/j.maturitas.2013.01.016
Hedman S, Nydahl M, Faxén-Irving G (2016) Individually prescribed diet is fundamental to optimize nutritional treatment in geriatric patients. Clin Nutr 35:692–698. https://doi.org/10.1016/j.clnu.2015.04.018
Beaudart C, Gillain S, Petermans J et al (2014) Sarcopenia: what’s new in 2014. Rev Med Liege 69:251–257
Cruz-Jentoft AJ, Kiesswetter E, Drey M, Sieber CC (2017) Nutrition, frailty, and sarcopenia. Aging Clin Exp Res 29:43–48. https://doi.org/10.1007/s40520-016-0709-0
Penninx BWJH, Pahor M, Cesari M et al (2004) Anemia is associated with disability and decreased physical performance and muscle strength in the elderly. J Am Geriatr Soc 52:719–724. https://doi.org/10.1111/j.1532-5415.2004.52208.x
Sgrò P, Sansone M, Sansone A et al (2018) Physical exercise, nutrition and hormones: three pillars to fight sarcopenia. Aging Male. https://doi.org/10.1080/13685538.2018.1439004
Beaudart C, Dawson A, Shaw SC et al (2017) Nutrition and physical activity in the prevention and treatment of sarcopenia: systematic review. Osteoporos Int. https://doi.org/10.1007/s00198-017-3980-9
Denison HJ, Cooper C, Sayer AA, Robinson SM (2015) Prevention and optimal management of sarcopenia: a review of combined exercise and nutrition interventions to improve muscle outcomes in older people. Clin Interv Aging 10:859–869. https://doi.org/10.2147/CIA.S55842
Beaudart C, Rabenda V, Simmons M et al (2017) Effects of protein, essential amino acids, B-hydroxy B-methylbutyrate, creatine, dehydroepiandrosterone and fatty acid supplementation on muscle mass, muscle strength and physical performance in older people aged 60 years and over. A systematic review of the literature. J Nutr Heal Aging. https://doi.org/10.1007/s12603-017-0934-z
Nowson C, O’Connell S (2015) Protein requirements and recommendations for older people: a review. Nutrients 7:6874–6899. https://doi.org/10.3390/nu7085311
Cawood AL, Elia M, Stratton RJ (2012) Systematic review and meta-analysis of the effects of high protein oral nutritional supplements. Ageing Res Rev 11:278–296. https://doi.org/10.1016/j.arr.2011.12.008
Beaudart C, Buckinx F, Rabenda V et al (2014) The effects of vitamin D on skeletal muscle strength, muscle mass and muscle power: a systematic review and meta-analysis of randomized controlled trials. J Clin Endocrinol Metab 99:4336–4345. https://doi.org/10.1210/jc.2014-1742
Beaudart C, Reginster JYY, Petermans J et al (2015) Quality of life and physical components linked to sarcopenia: the SarcoPhAge study. Exp Gerontol 69:103–110. https://doi.org/10.1016/j.exger.2015.05.003
Baumgartner RN, Koehler KM, Gallagher D et al (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147:755–763
Schaap LA, Fox B, Henwood T et al (2016) Grip strength measurement: towards a standardized approach in sarcopenia research and practice. Eur Geriatr Med. https://doi.org/10.1016/j.eurger.2015.11.012
Guralnik JM, Ferrucci L, Pieper CF et al (2000) Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci 55:M221–M231
Arnault N (2013) Table de Composition des Aliments, étude NutriNet-Santé. [Food Composition Table, NutriNet-Santé Study]. Les éditions INSERM/Economica, Paris (in French)
Carriquiry AL (1999) Assessing the prevalence of nutrient inadequacy. Public Health Nutr 2:23–33
Tombaugh TN, McIntyre NJ (1992) The mini-mental state examination: a comprehensive review. J Am Geriatr Soc 40:922–935
Yesavage JA, Brink TL, Rose TL et al (1982) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17:37–49
Voorrips LE, Ravelli AC, Dongelmans PC et al (1991) A physical activity questionnaire for the elderly. Med Sci Sports Exerc 23:974–979
ter Borg S, de Groot LCPGM, Mijnarends DM et al (2016) Differences in nutrient intake and biochemical nutrient status between sarcopenic and nonsarcopenic older adults—results from the maastricht sarcopenia study. J Am Med Dir Assoc 17:393–401. https://doi.org/10.1016/j.jamda.2015.12.015
Borack MS, Volpi E (2016) Efficacy and safety of leucine supplementation in the elderly. J Nutr 146:2625S–2629S. https://doi.org/10.3945/jn.116.230771
Leenders M, van Loon LJ (2011) Leucine as a pharmaconutrient to prevent and treat sarcopenia and type 2 diabetes. Nutr Rev 69:675–689. https://doi.org/10.1111/j.1753-4887.2011.00443.x
Houston DK, Nicklas BJ, Ding J et al (2008) Dietary protein intake is associated with lean mass change in older, community-dwelling adults: the health, aging, and body composition (Health ABC) study. Am J Clin Nutr 87:150–155
Beasley JM, LaCroix AZ, Larson JC et al (2014) Biomarker-calibrated protein intake and bone health in the women’s health initiative clinical trials and observational study. Am J Clin Nutr 99:934–940. https://doi.org/10.3945/ajcn.113.076786
McLean RR, Mangano KM, Hannan MT et al (2016) Dietary protein intake is protective against loss of grip strength among older adults in the framingham offspring cohort. J Gerontol Ser A Biol Sci Med Sci 71:356–361. https://doi.org/10.1093/gerona/glv184
de Baaij JHF, Hoenderop JGJ, Bindels RJM (2015) Magnesium in man: implications for health and disease. Physiol Rev 95:1–46. https://doi.org/10.1152/physrev.00012.2014
Lukaski HC (2000) Magnesium, zinc, and chromium nutriture and physical activity. Am J Clin Nutr 72:585S–593S. https://doi.org/10.1093/ajcn/72.2.585S
Clausen T, Everts ME (1989) Regulation of the Na, K-pump in skeletal muscle. Kidney Int 35:1–13
Beard JL (2001) Iron biology in immune function, muscle metabolism and neuronal functioning. J Nutr 131:568S–580S. https://doi.org/10.1093/jn/131.2.568S
van Dronkelaar C, van Velzen A, Abdelrazek M et al (2018) Minerals and sarcopenia; the role of calcium, iron, magnesium, phosphorus, potassium, selenium, sodium, and zinc on muscle mass, muscle strength, and physical performance in older adults: a systematic review. J Am Med Dir Assoc 19:6.e3–11.e3. https://doi.org/10.1016/j.jamda.2017.05.026
Veronese N, Berton L, Carraro S et al (2014) Effect of oral magnesium supplementation on physical performance in healthy elderly women involved in a weekly exercise program: a randomized controlled trial. Am J Clin Nutr 100:974–981. https://doi.org/10.3945/ajcn.113.080168
Verlaan S, Aspray TJ, Bauer JM et al (2017) Nutritional status, body composition, and quality of life in community-dwelling sarcopenic and non-sarcopenic older adults: a case–control study. Clin Nutr 36:267–274. https://doi.org/10.1016/J.CLNU.2015.11.013
Verlaan S, Aspray TJ, Bauer JM et al (2015) Nutritional status, body composition, and quality of life in community-dwelling sarcopenic and non-sarcopenic older adults: a case–control study. Clin Nutr. https://doi.org/10.1016/j.clnu.2015.11.013
Waters DL, Wayne SJ, Andrieu S et al (2014) Sexually dimorphic patterns of nutritional intake and eating behaviors in community-dwelling older adults with normal and slow gait speed. J Nutr Health Aging 18:228–233. https://doi.org/10.1007/s12603-014-0004-8
Scott D, Blizzard L, Fell J et al (2010) Associations between dietary nutrient intake and muscle mass and strength in community-dwelling older adults: the tasmanian older adult cohort study. J Am Geriatr Soc 58:2129–2134. https://doi.org/10.1111/j.1532-5415.2010.03147.x
Bartali B, Frongillo EA, Guralnik JM et al (2008) Serum micronutrient concentrations and decline in physical function among older persons. JAMA 299:308–315. https://doi.org/10.1001/jama.299.3.308
Martin H, Aihie Sayer A, Jameson K et al (2011) Does diet influence physical performance in community-dwelling older people? Findings from the Hertfordshire cohort study. Age Ageing 40:181–186. https://doi.org/10.1093/ageing/afq175
Chen Y-L, Yang K-C, Chang H-H et al (2014) Low serum selenium level is associated with low muscle mass in the community-dwelling elderly. J Am Med Dir Assoc 15:807–811. https://doi.org/10.1016/J.JAMDA.2014.06.014
Beck J, Ferrucci L, Sun K et al (2007) Low serum selenium concentrations are associated with poor grip strength among older women living in the community. BioFactors 29:37–44. https://doi.org/10.1002/biof.5520290104
Lauretani F, Semba RD, Bandinelli S et al (2007) Association of low plasma selenium concentrations with poor muscle strength in older community-dwelling adults: the InCHIANTI Study. Am J Clin Nutr 86:347–352. https://doi.org/10.1093/ajcn/86.2.347
Galaris D, Pantopoulos K (2008) Oxidative stress and iron homeostasis: mechanistic and health aspects. Crit Rev Clin Lab Sci 45:1–23. https://doi.org/10.1080/10408360701713104
Baumann CW, Kwak D, Liu HM, Thompson LV (2016) Age-induced oxidative stress: how does it influence skeletal muscle quantity and quality? J Appl Physiol 121:1047–1052. https://doi.org/10.1152/japplphysiol.00321.2016
Hashemi R, Motlagh AD, Heshmat R et al (2015) Diet and its relationship to sarcopenia in community dwelling Iranian elderly: a cross sectional study. Nutrition 31:97–104. https://doi.org/10.1016/J.NUT.2014.05.003
Bollwein J, Diekmann R, Kaiser MJ et al (2013) Dietary quality is related to frailty in community-dwelling older adults. J Gerontol Ser A Biol Sci Med Sci 68:483–489. https://doi.org/10.1093/gerona/gls204
Talegawkar SA, Bandinelli S, Bandeen-Roche K et al (2012) A higher adherence to a mediterranean-style diet is inversely associated with the development of frailty in community-dwelling elderly men and women. J Nutr 142:2161–2166. https://doi.org/10.3945/jn.112.165498
Acknowledgements
We would first thank all participants of the SarcoPhAge study for the time they dedicated in our research and for their fidelity over the years. We would like to acknowledge Pr. Michèle Guillaume, head of the Department of Public Health of the University of Liège for her help and support in designing our Food Frequency Questionnaire. Moreover, we thank Nathalie Arnault, biostatistician from the «Equipe de Recherche en Epidémiologie Nutritionnelle (EREN, UMR U1153 Inserm/U1125 Inra/Cnam/Universités Paris 5, 7 et 13, Centre de Recherche en Epidémiologie et Statistiques Sorbonne Paris Cité (CRESS)» for their support in analysing results of the Food Frequency Questionnaire.
Funding
CB and ML are supported by a fellowship from the FNRS (Fonds National de la Recherche Scientifique de Belgique—FRSFNRS—http://www.frs-fnrs.be).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee as well as with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Beaudart, C., Locquet, M., Touvier, M. et al. Association between dietary nutrient intake and sarcopenia in the SarcoPhAge study. Aging Clin Exp Res 31, 815–824 (2019). https://doi.org/10.1007/s40520-019-01186-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-019-01186-7