Abstract
Background
Statins therapy in the secondary prevention of coronary artery disease (CAD) is associated with a lower risk of adverse cardiovascular events. However, little is known regarding the association of elderly patients with nutritional risk on statin therapy.
Aims
To investigate whether older patients with CAD who were at nutritional risk gain similar survival benefit from statins therapy as their counterparts without nutritional risk.
Methods
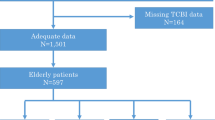
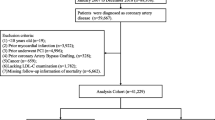
We conducted a retrospective hospital-based cohort study among 1705 patients with CAD who were older than 65 years of age, using coronary heart disease database from 2008 to 2012. Nutritional status of included patients was gauged using the geriatric nutritional risk index. After stratification by nutritional status, the hazard of all-cause death was compared between those with or without statins therapy.
Results
Of the 1705 patients included in the study (mean age 72 years; 73% male), all-cause death occurred in 146 (9.2%) patients with statins use and in 33 (26.2%) patients without statins use. The rate of all-cause death was higher in patients not receiving statins irrespective of nutritional status. After adjustments for potential confounders, the HR with statins use was 0.33 (95% CI 0.20–0.55) in patients without nutritional risk and 0.47 (95% CI 0.22–1.00) in patients with nutritional risk. No interaction effect was detected between nutritional status and statins use in relation to all-cause death (P value for interaction effect 0.516).
Conclusion
Despite of the patient’s nutritional status, statins therapy as a secondary prevention in elderly CAD patients was associated with decreased risk of all-cause death.



Similar content being viewed by others
References
Bibbins-Domingo K, Grossman DC, Curry SJ et al (2016) Statin use for the primary prevention of cardiovascular disease in adults: US preventive services task force recommendation statement. JAMA 316:1997–2007
Catapano AL, Graham I, De Backer G et al (2016) 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J 37:2999–3058
Jacobson TA, Ito MK, Maki KC et al (2014) National lipid association recommendations for patient-centered management of dyslipidemia: part 1—executive summary. J Clin Lipidol 8:473–488
Jellinger PS, Handelsman Y, Rosenblit PD et al (2017) American association of clinical endocrinologists and American college of endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract 23:1–87
Baigent C, Blackwell L, Emberson J et al (2010) Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 376:1670–1681
Mallery LH, Moorhouse P, McLean Veysey P et al (2017) Severely frail elderly patients do not need lipid-lowering drugs. Cleve Clin J Med 84:131–142
Yamada K, Furuya R, Takita T et al (2008) Simplified nutritional screening tools for patients on maintenance hemodialysis. Am J Clin Nutr 87:106–113
Bouillanne O, Morineau G, Dupont C et al (2005) Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr 82:777–783
Abd-El-Gawad WM, Abou-Hashem RM, El Maraghy MO et al (2014) The validity of Geriatric Nutrition Risk Index: simple tool for prediction of nutritional-related complication of hospitalized elderly patients. Comparison with mini nutritional assessment. Clin Nutr 33:1108–1116
Cereda E, Klersy C, Pedrolli C et al (2015) The Geriatric Nutritional Risk Index predicts hospital length of stay and in-hospital weight loss in elderly patients. Clin Nutr 34:74–78
Pilotto A, Gallina P, Panza F et al (2016) Relation of statin use and mortality in community-dwelling frail older patients with coronary artery disease. Am J Cardiol 118:1624–1630
Pilotto A, Panza F, Copetti M et al (2015) Statin treatment and mortality in community-dwelling frail older patients with diabetes mellitus: a retrospective observational study. PLoS One 10:e0130946
Galindo-Ocana J, Bernabeu-Wittel M, Formiga F et al (2012) Effects of renin-angiotensin blockers/inhibitors and statins on mortality and functional impairment in polypathological patients. Eur J Intern Med 23:179–184
Eaton CB, Lapane KL, Murphy JB et al (2002) Effect of statin (HMG-Co-A-Reductase Inhibitor) use on 1-year mortality and hospitalization rates in older patients with cardiovascular disease living in nursing homes. J Am Geriatr Soc 50:1389–1395
Peeters G, Tett SE, Hollingworth SA et al (2017) Associations of guideline recommended medications for acute coronary syndromes with fall-related hospitalizations and cardiovascular events in older women with ischemic heart disease. J Gerontol A Biol Sci Med Sci 72:259–265
Kutner JS, Blatchford PJ, Taylor DH Jr et al (2015) Safety and benefit of discontinuing statin therapy in the setting of advanced, life-limiting illness: a randomized clinical trial. JAMA Intern Med 175:691–700
Thai M, Hilmer S, Pearson SA et al (2015) Prevalence of potential and clinically relevant statin–drug interactions in frail and robust older inpatients. Drugs Aging 32:849–856
Gnjidic D, Le Couteur DG, Blyth FM et al (2013) Statin use and clinical outcomes in older men: a prospective population-based study. BMJ Open 3:e002333
Rossello X, Pocock SJ, Julian DG (2015) Long-Term use of cardiovascular drugs: challenges for research and for patient care. J Am Coll Cardiol 66:1273–1285
Funding
This work was supported by the National Natural Science Foundation of China under Grant (numbers: 81370219 and 81400267, Beijing, China); the Supporting Project of Sichuan Provincial Department of Science and Technology under Grant (number 2014SZ0004, Sichuan, China); and the Sichuan province Science and Technology Innovation Team under Grant (number 2017TD0004, Sichuan, China).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Research involving human participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Huang, Bt., Huang, Fy., Pu, Xb. et al. No modifying effect of nutritional status on statins therapy in relation to all-cause death in older patients with coronary artery disease. Aging Clin Exp Res 30, 1071–1077 (2018). https://doi.org/10.1007/s40520-017-0881-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-017-0881-x