Abstract
Background
The aim was to identify fall predictors in elderly suffering from chronic pain (CP) and to test their applicability among patients with other chronic conditions.
Methods
1,379 non-institutionalized patients aged 65 years and older who were suffering from CP (S.AGE CP sub-cohort) were monitored every 6 months for 1 year. Socio-demographic, clinical and pain data and medication use were assessed at baseline for the association with falls in the following year. Falls were assessed retrospectively at each study visit. Logistic regression analyses were performed to identify fall predictors. The derived model was applied to two additional S.AGE sub-cohorts: atrial fibrillation (AF) (n = 1,072) and type-2 diabetes mellitus (T2DM) (n = 983).
Results
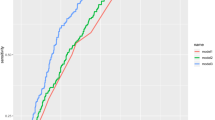
Four factors predicted falls in the CP sub-cohort: fall history (OR: 4.03, 95 % CI 2.79–5.82), dependency in daily activities (OR: 1.81, 95 % CI 1.27–2.59), age ≥75 (OR: 1.53, 95 % CI 1.04–2.25) and living alone (OR: 1.73, 95 % CI 1.24–2.41) (Area Under the Curve: AUC = 0.71, 95 % CI 0.67–0.75). These factors were relevant in AF (AUC = 0.71, 95 % CI 0.66–0.75) and T2DM (AUC = 0.67, 95 % CI 0.59–0.73) sub-cohorts. Fall predicted probability in CP, AF and T2DM sub-cohorts increased from 7, 7 and 6 % in patients with no risk factors to 59, 66 and 45 % respectively, in those with the four predictors. Fall history was the strongest predictor in the three sub-cohorts.
Conclusion
Fall history, dependency in daily activities, age ≥75 and living alone are independent fall predictors in CP, AF and T2DM patients.

Similar content being viewed by others
References
Leveille SG, Jones RN, Kiely DK, Hausdorff JM, Shmerling RH, Guralnik JM, Kiel DP, Lipsitz LA, Bean JF (2009) Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA 302(20):2214–2221
Becquemont L, Benattar-Zibi L, Bertin P, Berrut G, Corruble E, Danchin N, Delespierre T, Derumeaux G, Falissard B, Forette F, Hanon O, Pasquier F, Pinget M, Ourabah R, Piedvache C (2013) National observatory on the therapeutic management in ambulatory care patients aged 65 and over, with type 2 diabetes, chronic pain or atrial fibrillation. The S.AGES cohort, design and baseline characteristics of the study population. Therapie 68(4):1–19
Stubbs B, Binnekade T, Eggermont L, Sepehry AA, Patchay S, Schofield P (2014) Pain and the risk for falls in community-dwelling older adults: systematic review and meta-analysis. Arch Phys Med Rehabil 95(1):175–187e179
Kannus P, Sievanen H, Palvanen M, Jarvinen T, Parkkari J (2005) Prevention of falls and consequent injuries in elderly people. Lancet 366(9500):1885–1893
Tromp AM, Pluijm SM, Smit JH, Deeg DJ, Bouter LM, Lips P (2001) Fall-risk screening test: a prospective study on predictors for falls in community-dwelling elderly. J Clin Epidemiol 54(8):837–844
Wood BH, Bilclough JA, Bowron A, Walker RW (2002) Incidence and prediction of falls in Parkinson’s disease: a prospective multidisciplinary study. J Neurol Neurosurg Psychiatry 72(6):721–725
Stanmore EK, Oldham J, Skelton DA, O’Neill T, Pilling M, Campbell AJ, Todd C (2013) Risk factors for falls in adults with rheumatoid arthritis: a prospective study. Arthritis Care Res (Hoboken) 65(8):1251–1258
Harlein J, Dassen T, Halfens RJ, Heinze C (2009) Fall risk factors in older people with dementia or cognitive impairment: a systematic review. J Adv Nurs 65(5):922–933
Baetens T, De Kegel A, Calders P, Vanderstraeten G, Cambier D (2011) Prediction of falling among stroke patients in rehabilitation. J Rehabil Med 43(10):876–883
Hung C-Y, Wu T-J, Wang K-Y, Huang J-L, Loh E-W, Chen Y-M, Lin C-S, Chen D-Y, Tang Y-J (2013) Falls and Atrial Fibrillation in Elderly Patients. Acta Cardiol Sin 29:436–443
Maurer MS, Burcham J, Cheng H (2005) Diabetes mellitus is associated with an increased risk of falls in elderly residents of a long-term care facility. J Gerontol A Biol Sci Med Sci 60(9):1157–1162
Stubbs B, Schofield P, Binnekade T, Patchay S, Sepehry A, Eggermont L (2014) Pain is associated with recurrent falls in community-dwelling older adults: evidence from a systematic review and meta-analysis. Pain Med 15(7):1115–1128
Pokela N, Bell JS, Lihavainen K, Sulkava R, Hartikainen S (2010) Analgesic use among community-dwelling people aged 75 years and older: A population-based interview study. Am J Geriatr Pharmacother 8(3):233–244
Bertin P, Becquemont L, Corruble E, Derumeaux G, Falissard B, Hanon O, Pinget M, Forette F (2013) The therapeutic management of chronic pain in ambulatory care patients aged 65 and over in France: the S.AGES Cohort. Baseline data. J Nutr Health Aging 17(8):681–686
Tinetti ME, Speechley M, Ginter SF (1988) Risk factors for falls among elderly persons living in the community. N E J Med 319(26):1701–1707
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW (1963) Studies of illness in the aged. the index of ADL: a standardized measure of biological and psychosocial function. JAMA 185:914–919
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Marc LG, Raue PJ, Bruce ML (2008) Screening performance of the 15-item geriatric depression scale in a diverse elderly home care population. Am J Geriatr Psychiatry 16(11):914–921
Bueno-Cavanillas A, Padilla-Ruiz F, Jimenez-Moleon JJ, Peinado-Alonso CA, Galvez-Vargas R (2000) Risk factors in falls among the elderly according to extrinsic and intrinsic precipitating causes. Eur J Epidemiol 16(9):849–859
Chu LW, Chi I, Chiu AY (2005) Incidence and predictors of falls in the chinese elderly. Ann Acad Med Singapore 34(1):60–72
Bloch F, Thibaud M, Dugue B, Breque C, Rigaud AS, Kemoun G (2010) Episodes of falling among elderly people: a systematic review and meta-analysis of social and demographic pre-disposing characteristics. Clinics (Sao Paulo) 65(9):895–903
von Heideken Wagert P, Gustafson Y, Kallin K, Jensen J, Lundin-Olsson L (2009) Falls in very old people: the population-based Umea 85+ study in Sweden. Arch Gerontol Geriatr 49(3):390–396
Langlois JA, Smith GS, Nelson DE, Sattin RW, Stevens JA, DeVito CA (1995) Dependence in activities of daily living as a risk factor for fall injury events among older people living in the community. J Am Geriatr Soc 43(3):275–278
Blyth FM, Cumming R, Mitchell P, Wang JJ (2007) Pain and falls in older people. Eur J Pain 11(5):564–571
Wickham C, Cooper C, Margetts BM, Barker DJ (1989) Muscle strength, activity, housing and the risk of falls in elderly people. Age Ageing 18(1):47–51
Buatois S, Perret-Guillaume C, Gueguen R, Miget P, Vancon G, Perrin P, Benetos A (2010) A simple clinical scale to stratify risk of recurrent falls in community-dwelling adults aged 65 years and older. Phys Ther 90(4):550–560
Kharicha K, Iliffe S, Harari D, Swift C, Gillmann G, Stuck AE (2007) Health risk appraisal in older people 1: are older people living alone an “at-risk” group? Br J Gen Pract 57(537):271–276
Leveille SG, Ling S, Hochberg MC, Resnick HE, Bandeen-Roche KJ, Won A, Guralnik JM (2001) Widespread musculoskeletal pain and the progression of disability in older disabled women. Ann Intern Med 135(12):1038–1046
Bekibele CO, Gureje O (2010) Fall incidence in a population of elderly persons in Nigeria. Gerontology 56(3):278–283
Muraki S, Akune T, Oka H, En-Yo Y, Yoshida M, Nakamura K, Kawaguchi H, Yoshimura N (2011) Prevalence of falls and the association with knee osteoarthritis and lumbar spondylosis as well as knee and lower back pain in Japanese men and women. Arthritis Care Res (Hoboken) 63(10):1425–1431
Patel KV, Phelan EA, Leveille SG, Lamb SE, Missikpode C, Wallace RB, Guralnik JM, Turk DC (2014) High prevalence of falls, fear of falling, and impaired balance in older adults with pain in the United States: findings from the 2011 national health and aging trends study. J Am Geriatr Soc 62(10):1844–1852
Stubbs B, Eggermont L, Patchay S, Schofield P (2014) Older adults with chronic musculoskeletal pain are at increased risk of recurrent falls and the brief pain inventory could help identify those most at risk. Geriatr Gerontol Int. doi:10.111/ggi.12357
Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, Marra CA (2009) Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 169(21):1952–1960
Leipzig RM, Cumming RG, Tinetti ME (1999) Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc 47(1):30–39
Leipzig RM, Cumming RG, Tinetti ME (1999) Drugs and falls in older people: a systematic review and meta-analysis: II. Cardiac and analgesic drugs. J Am Geriatr Soc 47(1):40–50
Santos AC, Nobre MR, Nussbacher A, Rodrigues GH, Gebara OC, Azul JB, Wajngarten M (2012) Predictors of the risk of falls among elderly with chronic atrial fibrillation. Clinics (Sao Paulo) 67(4):305–311
Azidah AK, Hasniza H, Zunaina E (2012) Prevalence of falls and Its associated factors among elderly diabetes in a tertiary center, Malaysia. Curr Gerontol Geriatr Res 2012:539073. doi:10.1155/2012/539073
Quandt SA, Stafford JM, Bell RA, Smith SL, Snively BM, Arcury TA (2006) Predictors of falls in a multiethnic population of older rural adults with diabetes. J Gerontol A Biol Sci Med Sci 61(4):394–398
Stubbs B, Eggermont LH, Patchay S, Schofield PA (2014) Pain interference is associated with psychological concerns related to falls in community-dwelling older adults: multisite observational study. Phys Ther 94(10):1410–1420
Conflict of interest
Lazkani A: no conflict of interest. Becquemont L: received consulting fees from Sanofi-Aventis, Pfizer and Servier and lecture fees from Genzyme, GlaxoSmithKline, Bristol-Myers Squibb and Merck Sharp & Dohme. Close family member working at Sanofi France. Delespierre T: no conflict of interest. Benattar-Zibi L: no conflict of interest. Bauduceau B: received consulting fees from Sanofi-Aventis, Bristol-Myers Squibb, Merck Sharp & Dohme, Roche and Novo Nordisk. Bertin P: received consulting fees from Sanofi-Aventis, Pfizer, Ethypharm and Reckitt Benckiser and speaking fees from Genevrier, Roche, Bristol-Myers Squibb and Merck Sharp & Dohme. Berrut G: received fees from Sanofi, Lundbeck, Eisai, Novartis, MSD, Amgen, Boehringer Ingelheim and Bayer. Corruble E: received consulting fees from Servier, Lundbeck, Sanofi-Aventis, Bristol Myers Squibb and Eisai. Danchin N: received consulting or speaking fees from AstraZeneca, BMS, Boehringer Ingelheim, Daiichi Sankyo, Eli Lilly, GSK, MSD Schering-Plough, Novartis, Novo Nordisk, Pierre Fabre, Pfizer, Roche, Sanofi-Aventis, Servier, Takeda and The Medicines Company. Derumeaux G: received consulting or speaking fees from Actelion, Boehringer Ingelheim, Pfizer, Sanofi-Aventis and Servier. Research grant from Actelion and AstraZeneca. Doucet J: received speaking fees from Novo Nordisk, consulting fees from Sanofi-Aventis, Novo Nordisk and Merck Serono and has a research partnership with Lilly. Falissard B: received consulting fees from Sanofi-Aventis, Servier, Roche, AstraZeneca, Grünenthal, Lilly, HRA, Boehringer Ingelheim, Bayer, Novartis, Genzyme, Stallergenes, Daiichi, Otsuka and BMS. Forette F: received speaking and consulting fees from AstraZeneca, Bayer, BMS, Esaï, Exonhit, Fabre, Ipsen, Janssen-Cilag, Lilly, Lundbeck, Novartis, MSD, Merz, Pfizer, Roche, Sanofi-Aventis, Servier, Schwartz Pharma, Specia, Warner–Lambert and Wyeth. Hanon O: received speaking and consulting fees from AstraZeneca, Bayer, BMS, Boehringer, Esaï, Exonhit, Janssen-Cilag, Lundbeck, Novartis, Pfizer, Sanofi-Aventis and Servier. Pasquier F: Investigator for Eisai, Exonhit, Novartis, Ipsen, Medivation, Pfizer, Bayer, Noscira, Sanofi, Roche and GE Healthcare. Received consulting fees from Lilly, Bayer, Janssen and Sanofi. Pinget M: received speaking and consulting fees from Asdia, AstraZeneca, BMS, Medtronic, MSD, Novo Nordisk, Novartis, Roche Diagnostic and Ypsomed. Ourabah R: no conflict of interest. Piedvache C: no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lazkani, A., Delespierre, T., Bauduceau, B. et al. Predicting falls in elderly patients with chronic pain and other chronic conditions. Aging Clin Exp Res 27, 653–661 (2015). https://doi.org/10.1007/s40520-015-0319-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-015-0319-2