Abstract
Purpose
Limited data are available linking breakfast consumption to Heart Burn Syndrome (HBS). This study was done to investigate to find whether breakfast consumption is associated with HBS. This cross-sectional study was done to investigate the association between breakfast consumption and HBS among Iranian adults.
Methods
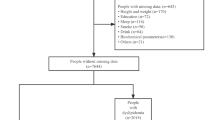
This cross-sectional study was performed among 4763 general adults of Isfahan, Iran. Participants’ patterns of breakfast eating were assessed by asking two questions from them. How often do you eat breakfast in a week?” Participants were able to respond as: "never or 1 day/wk", "2–4 days/wk", "5–6 days/wk", "every day". HBS was defined as the presence of HBS at sometimes, often or always using a Persian version of validated self-administered modified ROME III questionnaire.
Results
Totally, 4763 patients with HBS completed this cross-sectional study, where about 32.4% of them intake breakfast less than one time per week. After controlling for potential confounders, participants who consumed breakfast every day had a 43% lower risk for having HBS as compared with those who had breakfast ≤ 1 times/wk (OR 0.57; 95% CI 0.41–0.80). A significant inverse relationship was found between breakfast consumption and frequent than scare HBS (OR 0.57; 95% CI 0.40–0.77) among the whole population, not in patients with HBS. No significant association was observed between breakfast intake and severity of HBS (OR 0.56; 95% CI 0.31–1.04).
Conclusion
We found an inverse association between frequency of breakfast consumption and odds of HBS as well as the frequency of HBS among the adult population. Prospective studies are required to confirm these findings.
Level of evidence
Level V, cross-sectional descriptive study.


Similar content being viewed by others
References
Leu HB, Chen JW, Wu TC, Ding YA, Lin SJ, Charng MJ (2005) Effects of fluvastatin, an HMG-CoA reductase inhibitor, on serum levels of interleukin-18 and matrix metalloproteinase-9 in patients with hypercholesterolemia. Clin Cardiol 28(9):423–428. https://doi.org/10.1002/clc.4960280907
Panichi V, Paoletti S, Mantuano E, Manca-Rizza G, Filippi C, Santi S, Taccola D, Donadio C, Tramonti G, Innocenti M, Casto G, Consani C, Sbragia G, Franzoni F, Galetta F, Panicucci E, Barsotti G (2006) In vivo and in vitro effects of simvastatin on inflammatory markers in pre-dialysis patients. Nephrol Dial Transpl 21(2):337–344. https://doi.org/10.1093/ndt/gfi224
Bruni F, Pasqui AL, Pastorelli M, Bova G, Cercignani M, Palazzuoli A, Sawamura T, Gioffre WR, Auteri A, Puccetti L (2005) Different effect of statins on platelet oxidized-LDL receptor (CD36 and LOX-1) expression in hypercholesterolemic subjects. Clin Appl Thromb Hemost 11(4):417–428. https://doi.org/10.1177/107602960501100408
Sola S, Mir MQ, Rajagopalan S, Helmy T, Tandon N, Khan BV (2005) Statin therapy is associated with improved cardiovascular outcomes and levels of inflammatory markers in patients with heart failure. J Card Fail 11(8):607–612. https://doi.org/10.1016/j.cardfail.2005.05.011
Ray KK, Cannon CP, Cairns R, Morrow DA, Rifai N, Kirtane AJ, McCabe CH, Skene AM, Gibson CM, Ridker PM, Braunwald E (2005) Relationship between uncontrolled risk factors and C-reactive protein levels in patients receiving standard or intensive statin therapy for acute coronary syndromes in the PROVE IT-TIMI 22 trial. J Am Coll Cardiol 46(8):1417–1424. https://doi.org/10.1016/j.jacc.2005.08.024
Damas JK, Boullier A, Waehre T, Smith C, Sandberg WJ, Green S, Aukrust P, Quehenberger O (2005) Expression of fractalkine (CX3CL1) and its receptor, CX3CR1, is elevated in coronary artery disease and is reduced during statin therapy. Arterioscler Thromb Vasc Biol 25(12):2567–2572. https://doi.org/10.1161/01.ATV.0000190672.36490.7b
Nakaya R, Uzui H, Shimizu H, Nakano A, Mitsuke Y, Yamazaki T, Ueda T, Lee JD (2005) Pravastatin suppresses the increase in matrix metalloproteinase-2 levels after acute myocardial infarction. Int J Cardiol 105(1):67–73. https://doi.org/10.1016/j.ijcard.2004.12.024
Meredith IT, Plunkett JC, Worthley SG, Hope SA, Cameron JD (2005) Systemic inflammatory markers in acute coronary syndrome: association with cardiovascular risk factors and effect of early lipid lowering. Coron Artery Dis 16(7):415–422
ter Avest E, Abbink EJ, Holewijn S, de Graaf J, Tack CJ, Stalenhoef AF (2005) Effects of rosuvastatin on endothelial function in patients with familial combined hyperlipidaemia (FCH). Curr Med Res Opin 21(9):1469–1476. https://doi.org/10.1185/030079905x61910
Verma A, Ranganna KM, Reddy RS, Verma M, Gordon NF (2005) Effect of rosuvastatin on C-reactive protein and renal function in patients with chronic kidney disease. Am J Cardiol 96(9):1290–1292. https://doi.org/10.1016/j.amjcard.2005.06.074
Milionis HJ, Gazi IF, Filippatos TD, Tzovaras V, Chasiotis G, Goudevenos J, Seferiadis K, Elisaf MS (2005) Starting with rosuvastatin in primary hyperlipidemia–Is there more than lipid lowering? Angiology 56(5):585–592. https://doi.org/10.1177/000331970505600510
Stalenhoef AF, Ballantyne CM, Sarti C, Murin J, Tonstad S, Rose H, Wilpshaar W (2005) A comparative study with rosuvastatin in subjects with metabolic syndrome: results of the COMETS study. Eur Heart J 26(24):2664–2672. https://doi.org/10.1093/eurheartj/ehi482
Yamamichi N, Mochizuki S, Asada-Hirayama I, Mikami-Matsuda R, Shimamoto T, Konno-Shimizu M, Takahashi Y, Takeuchi C, Niimi K, Ono S (2012) Lifestyle factors affecting gastroesophageal reflux disease symptoms: a cross-sectional study of healthy 19864 adults using FSSG scores. BMC Med 10(1):45. https://doi.org/10.1186/1741-7015-10-45
ter Avest E, Abbink EJ, de Graaf J, Tack CJ, Stalenhoef AF (2005) Effect of rosuvastatin on insulin sensitivity in patients with familial combined hyperlipidaemia. Eur J Clin Invest 35(9):558–564. https://doi.org/10.1111/j.1365-2362.2005.01549.x
Takebayashi K, Matsumoto S, Wakabayashi S, Inukai Y, Matsutomo R, Aso Y, Inukai T (2005) The effect of low-dose atorvastatin on circulating monocyte chemoattractant protein-1 in patients with type 2 diabetes complicated by hyperlipidemia. Metabolism 54(9):1225–1229. https://doi.org/10.1016/j.metabol.2005.04.008
Li JJ, Fang CH (2005) Effects of 4 weeks of atorvastatin administration on the antiinflammatory cytokine interleukin-10 in patients with unstable angina. Clin Chem 51(9):1735–1738. https://doi.org/10.1373/clinchem.2005.049700
Okopien B, Krysiak R, Kowalski J, Madej A, Belowski D, Zielinski M, Herman ZS (2005) Monocyte release of tumor necrosis factor-alpha and interleukin-1beta in primary type IIa and IIb dyslipidemic patients treated with statins or fibrates. J Cardiovasc Pharmacol 46(3):377–386
Adibi P, Keshteli AH, Esmaillzadeh A, Afshar H, Roohafza H, Bagherian-Sararoudi R, Daghaghzadeh H, Soltanian N, Feinle-Bisset C, Boyce P (2012) The study on the epidemiology of psychological, alimentary health and nutrition (SEPAHAN): overview of methodology. J Res Med Sci 17(2):292–298
Charan J, Biswas T (2013) How to calculate sample size for different study designs in medical research? Indian J Psychol Med 35(2):121
Policy PA (2009) Health improvement directorate. The General Practice Physical Activity Questionnaire (GPPAQ) A screening tool to assess adult physical activity levels, within primary care London: Department of Health. https://www.gov.uk
Oguma Y, Shinoda-Tagawa T (2004) Physical activity decreases cardiovascular disease risk in women: review and meta-analysis. Am J Prev Med 26(5):407–418. https://doi.org/10.1016/j.amepre.2004.02.007
Aminianfar S, Saneei P, Nouri M, Shafiei R, Hassanzadeh-Keshteli A, Esmaillzadeh A, Adibi P (2015) Validation study of self-reported anthropometric indices among the staff of the Isfahan University of Medical Sciences, Isfahan. Iran J Isfahan Med Sch 33(346):1318–1327
Ebrahimi-Mameghani M, Sabour S, Khoshbaten M, Arefhosseini SR, Saghafi-Asl M (2017) Total diet, individual meals, and their association with gastroesophageal reflux disease. Health Promot Perspect 7(3):155
Sethi S, Richter JE (2017) Diet and gastroesophageal reflux disease: role in pathogenesis and management. Curr Opin Gastroenterol 33(2):107–111. https://doi.org/10.1097/MOG.0000000000000337
Salari-Moghaddam A, Keshteli AH, Mousavi SM, Afshar H, Esmaillzadeh A, Adibi P (2019) Adherence to the MIND diet and prevalence of psychological disorders in adults. J Affect Disord 256:96–102
Sakaguchi K, Yagi T, Maeda A, Nagayama K, Uehara S, Saito-Sakoguchi Y, Kanematsu K, Miyawaki S (2014) Association of problem behavior with sleep problems and gastroesophageal reflux symptoms. Pediatr Int 56(1):24–30. https://doi.org/10.1111/ped.12201
Takeshita E, Furukawa S, Sakai T, Niiya T, Miyaoka H, Miyake T, Yamamoto S, Senba H, Yamamoto Y, Arimitsu E (2017) Eating behaviours and prevalence of gastroesophageal reflux disease in japanese patients with type 2 diabetes mellitus: the dogo study. Can J Diabetes. https://doi.org/10.1016/j.jcjd.2017.07.007
Nicklas TA, O’neil C, Myers L, (2004) The importance of breakfast consumption to nutrition of children, adolescents, and young adults. Nutr Today 39(1):30–39. https://doi.org/10.1097/00017285-200401000-00009
Otaki N, Obayashi K, Saeki K, Kitagawa M, Tone N, Kurumatani N (2017) Relationship between breakfast skipping and obesity among elderly: Cross-sectional analysis of the HEIJO-KYO study. J Nutr Health Aging 21(5):501–504. https://doi.org/10.1007/s12603-016-0792-0
Milajerdi A, Keshteli A, Esmaillzadeh A, Roohafza H, Afshar H, Adibi P (2018) Breakfast consumption in relation to lowered risk of psychological disorders among Iranian adults. Public Health. https://doi.org/10.1016/j.puhe.2018.05.020
Schubert ML (2008) Hormonal regulation of gastric acid secretion. Curr Gastroenterol Rep 10(6):523–527. https://doi.org/10.1007/s11894-008-0097-5
Gardner JD (2010) GERD: increased gastric acid secretion as a possible cause of GERD. Nat Rev Gastroenterol Hepatol 7(3):125–126. https://doi.org/10.1038/nrgastro.2009.240
Watanabe Y, Saito I, Henmi I, Yoshimura K, Maruyama K, Yamauchi K, Matsuo T, Kato T, Tanigawa T, Kishida T (2014) Skipping breakfast is correlated with obesity. J Rural Med 9(2):51–58. https://doi.org/10.2185/jrm.2887
Horikawa C, Kodama S, Yachi Y, Heianza Y, Hirasawa R, Ibe Y, Saito K, Shimano H, Yamada N, Sone H (2011) Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: a meta-analysis. Prev Med 53(4):260–267. https://doi.org/10.1016/j.ypmed.2011.08.030
Tanaka Y, Sakata Y, Hara M, Kawakubo H, Tsuruoka N, Yamamoto K, Itoh Y, Hidaka H, Shimoda R, Iwakiri R (2017) Risk factors for helicobacter pylori infection and endoscopic reflux esophagitis in healthy young Japanese volunteers. Intern Med. https://doi.org/10.2169/internalmedicine.8669-16
Mousavi SM, Shayanfar M, Rigi S, Mohammad-Shirazi M, Sharifi G, Esmaillzadeh A (2020) Adherence to the Mediterranean dietary pattern in relation to glioma: a case-control study. Clin Nutr. https://doi.org/10.1016/j.clnu.2020.05.022
McFarlin B, Carpenter K, Henning A, Venable A (2017) Consumption of a high-fat breakfast on consecutive days alters preclinical biomarkers for atherosclerosis. Eur J Clin Nutr 71(2):239–244. https://doi.org/10.1038/ejcn.2016.242
Nas A, Mirza N, Hägele F, Kahlhöfer J, Keller J, Rising R, Kufer TA, Bosy-Westphal A (2017) Impact of breakfast skipping compared with dinner skipping on regulation of energy balance and metabolic risk. Am J Clin Nutr 105(6):1351–1361. https://doi.org/10.3945/ajcn.116.151332
Kim JJ, Kim N, Choi YJ, Kim JS, Jung HC (2016) Increased TRPV1 and PAR2 mRNA expression levels are associated only with the esophageal reflux symptoms, but not with the extraesophageal reflux symptoms. Medicine. https://doi.org/10.1097/MD.0000000000004387
Asl SF, Mansour-Ghanaei F, Samadi H, Joukar F (2015) Evaluations of life style factors and the severity of gastroesophageal reflux disease; a case-control study. Int J Mol Epidemiol Genet 6(1):27
Acknowledgements
The authors acknowledge their staff, the fieldworkers, and SEPAHAN project participants that without them this work would not have been possible. This study was supported by the Vice Chancellery for Research and Technology, Isfahan University of Medical Sciences (IUMS).
Funding
SEPAHAN was financially supported by the Vice Chancellery for Research and Technology, Isfahan University of Medical Sciences (IUMS). This study was supported by funding from Isfahan University of Medical Sciences (Grant Number: 627002).
Author information
Authors and Affiliations
Contributions
AM and SMM wrote the manuscript. AE analyzed and interpreted the data. AHK, HR, HA, PA, and AE designed the study and contributed to data collection and interpretation. PA and AE revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
Ethical approval of the study was provided by the Medical Research Ethics Committee of Isfahan University of Medical Sciences (IUMS).
Informed consent
Informed consent was obtained from all participants in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Milajerdi, A., Bagheri, F., Mousavi, S.M. et al. Breakfast skipping and prevalence of heartburn syndrome among Iranian adults. Eat Weight Disord 26, 2173–2181 (2021). https://doi.org/10.1007/s40519-020-01065-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-020-01065-5