Abstract
Purposes
Aberrant eating patterns are frequently observed in bariatric patients. Since bariatric operations produce alterations in food transit and in appetite/satiety balance, postoperative eating behavior changes are not surprising.
Methods
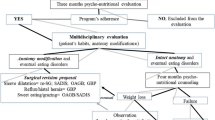
88 consecutive obese patients undergoing Roux-en-Y gastric bypass (RYGBP, 50 cases) and Sleeve Gastrectomy (SG, 38 cases) were retrospectively evaluated. Beside anthropometric data measurement, eating behavior was assessed by direct interview prior to the operation and at the first and second postoperative years: patients were considered as eating disordered (ED) when referred habitual occurrence of binge eating and nibbling/grazing. Weight loss was assessed by percent of BMI loss (% Δ BMI). Together with standard follow-up, patients received additional behavioral/dietetic support upon request.
Results
Postoperative ED patients showed lower % Δ BMI than the not ED ones at one (30.7% ± 8,5 vs. 26.8% ± 10, p < 0.02) and two (32% ± 10.3 vs. 27.4% ± 12.9, p < 0.05) years after operation, the follow-up rate being 82% and 76%, respectively, without differences between RYGBP and SG group. After RYGBP, an improvement of eating behavior was observed (ED patients from 75 to 28% at 1 year and to 27% at 2 years), while no changes were observed after SG. In SG patients, the number of additional behavioral/dietetic support sessions throughout the follow-up was positively associated with % Δ BMI.
Discussion
The postoperative normalization of eating pattern has a role in weight loss after bariatric surgery. Behavioral/dietetic support is indicated in all SG patient, while after RYGBP is useful only when weight loss is unsatisfactory.
Level of evidence
III: retrospective cohort study.


Similar content being viewed by others
References
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737. https://doi.org/10.1001/jama.292.14.1724
Puzziferri N, Roshek TB 3rd, Mayo HG, Gallagher R, Belle SH, Livingston EH (2014) Long-term follow-up after bariatric surgery: a systematic review. JAMA 312:934–942. https://doi.org/10.1001/jama.2014.10706
le Roux CW, Welbourn R, Werling M, Osborne A, Kokkinos A, Laurenius A et al (2007) Gut hormones as mediators of appetite and weight loss after Roux-en-Y gastric bypass. Ann Surg 246(5):780–785. https://doi.org/10.1097/sla.0b013e3180caa3e3
Malin SK, Kashyap SR (2015) Differences in weight loss and gut hormones: Rouen-Y gastric bypass and sleeve gastrectomy surgery. Curr Obes Rep. 4:279–286. https://doi.org/10.1007/s13679-015-0151-1
Benaiges D, Más-Lorenzo A, Goday A, Ramon JM, Chillarón JJ, Pedro-Botet J, Flores-Le Roux JA (2015) Laparoscopic sleeve gastrectomy: more than a restrictive bariatric surgery procedure? World J Gastroenterol 21:11804–11814. https://doi.org/10.3748/wjg.v21.i41.11804
Niego SH, Kofman MD, Weiss JJ, Geliebter A (2007) Binge eating in the bariatric surgery population: a review of the literature. Int J Eat Disord 40:349–359. https://doi.org/10.1002/eat.20376
Opozda M, Chur-Hansen A, Wittert G (2016) Changes in problematic and disordered eating after gastric bypass, adjustable gastric banding and vertical sleeve gastrectomy: a systematic review of pre-post studies. Obes Rev 17:770–792. https://doi.org/10.1111/obr.12425
Li W, Richard D (2017) Effects of bariatric surgery on energy homeostasis. Can J Diabetes 41:426–431. https://doi.org/10.1016/j.jcjd.2017.05.002
Sjöström L, Peltonen M, Jacobson P, Sjöström CD, Karason K, Wedel H et al (2012) Bariatric surgery and long-term cardiovascular events. JAMA 307:56–65. https://doi.org/10.1001/jama.2011.1914
Cardoso L, Rodrigues D, Gomes L, Carrilho F (2017) Short- and long-term mortality after bariatric surgery: a systematic review and meta-analysis. Diabetes Obes Metab 19:1223–1232. https://doi.org/10.1111/dom.12922
Pizato N, Botelho PB, Gonçalves VSS, Dutra ES, de Carvalho KMB (2017) Effect of grazing behavior on weight regain post-bariatric surgery: a systematic review. Nutrients 9(pii):E1322. https://doi.org/10.3390/nu9121322
Karmali S, Brar B, Shi X, Sharma AM, de Gara C, Birch DW (2013) Weight recidivism post-bariatric surgery: a systematic review. Obes Surg 23:1922–1933. https://doi.org/10.1007/s11695-013-1070-4
Fried M, Yumuk V, Oppert JM, Scopinaro N, Torres A, Weiner R, Yashkov Y, Frühbeck G, International Federation for Surgery of Obesity and Metabolic Disorders-European Chapter (IFSO-EC), European Association for the Study of Obesity (EASO), European Association for the Study of Obesity Obesity Management Task Force (EASO OMTF) (2014) Interdisciplinary European guidelines on metabolic and bariatric surgery. Obes Surg 24:42–55. https://doi.org/10.1007/s11695-013-1079-8
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders (DSM-4), 4th edn. American Psychiatric Association, Washington, p 202
Colles SL, Dixon JB, O’Brien PE (2008) Loss of control is central to psychological disturbance associated with binge eating disorder. Obesity (Silver Spring) 16:608–614. https://doi.org/10.1038/oby.2007.99
Opolski M, Chur-Hansen A, Wittert G (2015) The eating-related behaviours, disorders and expectations of candidates for bariatric surgery. Clin Obes 5:165–197. https://doi.org/10.1111/cob.12104
Parker K, Brennan L (2015) Measurement of disordered eating in bariatric surgery candidates: a systematic review of the literature. Obes Res Clin Pract 9:12–25. https://doi.org/10.1016/j.orcp.2014.01.005
Conceição EM, Utzinger LM, Pisetsky EM (2015) Eating disorders and problematic eating behaviours before and after bariatric surgery: characterization, assessment and association with treatment outcomes. Eur Eat Disord Rev 23:417–425. https://doi.org/10.1002/erv.2397
Meany G, Conceição E, Mitchell JE (2014) Binge eating, binge eating disorder and loss of control eating: effects on weight outcomes after bariatric surgery. Eur Eat Disord Rev 22:87–91. https://doi.org/10.1002/erv.2273
de Zwaan M, Hilbert A, Swan-Kremeier L, Simonich H, Lancaster K, Howell LM et al (2010) Comprehensive interview assessment of eating behavior 18–35 months after gastric bypass surgery for morbid obesity. Surg Obes Relat Dis 6:79–85. https://doi.org/10.1016/j.soard.2009.08.011
Hsu LK, Sullivan SP, Benotti PN (1997) Eating disturbances and outcome of gastric bypass surgery: a pilot study. Int J Eat Disord 21:385–390 (PMID: 9138051)
El Chaar M, McDeavitt K, Richardson S, Gersin KS, Kuwada TS, Stefanidis D (2011) Does patient compliance with preoperative bariatric office visits affect postoperative excess weight loss? Surg Obes Relat Dis 7:743–748. https://doi.org/10.1016/j.soard.2010.10.020
Galioto R, Gunstad J, Heinberg LJ, Spitznagel MB (2013) Adherence and weight loss outcomes in bariatric surgery: does cognitive function play a role? Obes Surg 23:1703–1710. https://doi.org/10.1007/s11695-013-1060-6
Kim HJ, Madan A, Fenton-Lee D (2014) Does patient compliance with follow-up influence weight loss after gastric bypass surgery? A systematic review and meta-analysis. Obes Surg 24:647–651. https://doi.org/10.1007/s11695-014-1178-1
Burgmer R, Grigutsch K, Zipfel S, Wolf AM, de Zwaan M, Husemann B et al (2005) The influence of eating behavior and eating pathology on weight loss after gastric restriction operations. Obes Surg 15:684–691. https://doi.org/10.1381/0960892053923798
Lager CJ, Esfandiari NH, Subauste AR, Kraftson AT, Brown MB, Cassidy RB et al (2017) Roux-En-Y gastric bypass vs. sleeve gastrectomy balancing the risks of surgery with the benefits of weight loss. Obes Surg 27:154–161. https://doi.org/10.1007/s11695-016-2265-2
Yang P, Chen B, Xiang S, Lin XF, Luo F, Li W (2019) Long-term outcomes of laparoscopic sleeve gastrectomy versus Roux-en-Y gastric bypass for morbid obesity: results from a meta-analysis of randomized controlled trials. Surg Obes Relat Dis 15:546–555. https://doi.org/10.1016/j.soard.2019.02.001
Kaiser KA, Franks SF, Smith AB (2011) Positive relationship between support group attendance and one-year postoperative weight loss in gastric banding patients. Surg Obes Relat Dis 7:89–93. https://doi.org/10.1016/j.soard.2010.07.013
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
This is retrospective clinical studies. All procedures performed were in accordance with the ethical standards of University of Genova, Ospedale Policlinico San Martino, Genova Italy, and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
All patients signed the informed consent for the operation and for the anonymous data processing.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gradaschi, R., Molinari, V., Sukkar, S.G. et al. Disordered eating and weight loss after bariatric surgery. Eat Weight Disord 25, 1191–1196 (2020). https://doi.org/10.1007/s40519-019-00749-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-019-00749-x