Abstract
Purpose
Few studies have assessed the relationship between meal skipping with subjective health complaints in children and adolescents. The aim of our study was to determine the association between meal skipping and subjective health complaints in this population.
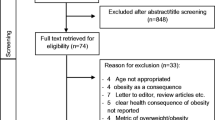
Methods
A total of 14,400 students aged 7–18 years were selected using multistage stratified cluster sampling method from 30 provinces of Iran. Data were collected as a part of the fifth national school-based surveillance program (CASPIAN-V) in Iran. Information about students’ lifestyle, health behaviours, health status and health complaints were gathered through a validated questionnaire.
Results
The mean (standard deviation) age of participants was 12.3 (3.2) years old. Breakfast skipping was associated with increased odds of stomachache (OR 1.77, 95% CI 1.56, 2.00), backache (OR 1.68, 95% CI 1.46, 1.92), difficulty in getting to sleep (OR 1.66, 95% CI 1.48, 1.86), feeling nervous (OR 1.59, 95% CI 1.43, 1.76) and irritability (OR 1.29, 95% CI 1.02, 1.25). There were 27, 63, 58 and 107% increase in odds of headache, stomachache, backache and difficulty in getting to sleep by lunch skipping, respectively. While dinner skipping was related to 39, 59 and 52% increase in odds of headache, feeling low and difficulty in getting to sleep, respectively, it was associated with decreased odds of stomachache (OR 0.33, 95% CI 0.25, 0.44).
Conclusions
Our study suggests that meal skipping is associated with some somatic and psychological health complaints among children; therefore, regular meal consumption, at least three times a day, is highly recommended in this population.
Level of evidence
V, cross-sectional descriptive study.
Similar content being viewed by others
References
Roberts C, Freeman J, Samdal O et al (2009) The Health Behaviour in School-aged Children (HBSC) study: methodological developments and current tensions. Int J Public Health 54(Suppl 2):140–150. https://doi.org/10.1007/s00038-009-5405-9
Bullinger M (2002) Assessing health related quality of life in medicine. An overview over concepts, methods and applications in international research. Restor Neurol Neurosci 20:93–101. https://content.iospress.com/articles/restorative-neurology-and-neuroscience/rnn00198. Accessed Dec 2017
Eriksen HR, Ihlebaek C (2002) Subjective health complaints. Scand J Psychol 43(2):101–103. https://doi.org/10.1111/1467-9450.00274
Taillefer MC, Dupuis G, Roberge MA et al (2003) Health-related quality of life models: systemic review of the literature. Sol Indic Res 64:293–323. https://doi.org/10.1023/A:1024740307643
Gobina I, Valmaa R, Tynjala J et al (2011) The medicine use and corresponding subjective health complaints among adolescents, a cross-national survey. Pharmacoepidemiol Drug Saf 20(4):424–431. https://doi.org/10.1002/pds.2102
Ravens-Sieberer U, Torsheim T, Hetland J et al (2009) Subjective health, symptom load and quality of life of children and adolescents in Europe. Int J Public Health 54:151–159. https://doi.org/10.1007/s00038-009-5406-8
Roelen CA, Koopmans PC, Groothoff JW (2010) Subjective health complaints in relation to sickness absence. Work 37(1):15–21. https://doi.org/10.3233/WOR-2010-1052
Pendergast FJ, Livingstone KM, Worsley A et al (2016) Correlates of meal skipping in young adults: a systematic review. Int J Behav Nut Phys Act 13:125. https://doi.org/10.1186/s12966-016-0451-1
Ghafari M, Doosti-Irani A, Amiri M et al (2017) Prevalence of the skipping breakfast among the Iranian students: a review article. Iran J Public Health 46(7):882–929. http://ijph.tums.ac.ir/index.php/ijph/article/view/10385/5789. Accessed Nov 2017
Kelishadi R, Mozafarian N, Qorbani M et al (2017) Is snack consumption associated with meal skipping in children and adolescents? The CASPIAN IV study. Eat Weight Disord 22(2):321–328. https://doi.org/10.1007/s40519-017-0370-4
Zilberter T, Zilberter EY (2014) Breakfast: to skip or not to skip. Front Public Health 2:59. https://doi.org/10.3389/fpubh.2014.00059
Chen J, Cheng J, Liu Y et al (2014) Association between breakfast eating habits and health-promoting lifestyle, suboptimal health status in Southern China: a population based, cross sectional study. J Transl Med 12:348. https://doi.org/10.1186/s12967-014-0348-1
Moschiano F, Messina P, D’Amico D et al (2012) Headache, eating and sleeping behaviors and lifestyle factors in preadolescents and adolescents: preliminary results from an Italian population study. Neurol Sci 33:87–90. https://doi.org/10.1007/s10072-012-1048-3
Motlagh ME, Ziaodini H, Qorbani M et al (2017) Methodology and early findings of the fifth survey of childhood and adolescence surveillance and prevention of adult noncommunicable disease: the CASPIANV study. Int J Prev Med 8:4. https://doi.org/10.4103/2008-7802.198915. eCollection 2017
Global School-based Student Health Survey (GSHS) (2012) World Health Organization. http://www.who.int/chp/gshs/en/. Accessed Jan 2018
Kelishadi R, Majdzadeh R, Motlagh ME,et al (2012) Development and evaluation of a questionnaire for assessment of determinants of weight disorders among children and adolescents: the CASPIAN IV study. Int J Prev Med 3:699–705. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3482997/
World Health Organization (2008) Training course on child growth assessment. WHO, Geneva. http://www.who.int/childgrowth/training/module_c_interpreting_indicators.pdf. Accessed Jan 2018
Salmon J, Campbell KJ, Crawford DA (2006) Television viewing habits associated with obesity risk factors: a survey of Melbourne school children. Med J Aust 184:64–67. https://www.mja.com.au/journal/2006/184/2/television-viewing-habits-associated-obesity-risk-factors-survey-melbourne. Accessed Nov 2017
Djalalinia SH, Qorbani M, Rezaei N, Sheidaei A, Mahdavi-Gorabi A, Kasaeian A (2017) Joint association of screen time and physical activity anthropometric measures in Iranian children and adolescents: the weight disorders survey of the CASPIAN-IV study. J Pediatr Endocrinol Metab 30(7):731–738. https://doi.org/10.1515/jpem-2016-0486
Adeniyi AF, Okafor NC, Adeniyi CY (2011) Depression and physical activity in a sample of Nigerian adolescents: levels, relationships and predictors. Child Adolesc Psychiatry Ment Health 5:16. https://doi.org/10.1186/1753-2000-5-16
Kowalski KC, Crocker PR, Donen RM (2004) The physical activity questionnaire for older children (PAQ-C) and adolescents (PAQ-A) manual. College of Kinesiology, University of Saskatchewan 87, Canada. https://www.prismsports.org/UserFiles/file/PAQ_manual_ScoringandPDF.pdf. Accessed Mar 2018
Kelishadi R, Motlagh ME, Roomizadeh P et al (2013) First report on path analysis for cardiometabolic components in a nationally representative sample of pediatric population in the Middle East and North Africa (MENA): the CASPIAN III study. Ann Nutr Metab 62(3):257–265. https://doi.org/10.1159/000346489
Haugland S, Wold B, Stevenson J et al (2001) Subjective health complaints in adolescence: a cross national comparison of prevalence and dimensionality. Eur J Public Health 11(1):4–10. https://doi.org/10.1177/140349480203000309
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B 57:289–300. https://doi.org/10.2307/2346101
Kafeshani O, Sarrafzadegan N, Nouri F, Mohammadifard N (2015) Major dietary patterns in Iranian adolescents: Isfahan healthy heart program, Iran. ARYA Atheroscler 11(Suppl 1):61–68. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4530660/. Accessed Dec 2017
Leech RM, Worsley A, Timperio A et al (2015) Understanding meal patterns: definitions, methodology and impact on nutrient intake and diet quality. Nutr Res Rev 28:1–21. https://doi.org/10.1017/S0954422414000262
Shenkin A (2006) Micronutrients in health and disease. Postgrad Med J 82:559–567. https://doi.org/10.1136/pgmj.2006.047670
Chen X, Sekine M, Hamanishi S et al (2005) Lifestyles and health related quality of life in Japanese school children: a cross-sectional study. Prev Med 40(6):668–678. https://doi.org/10.1016/j.ypmed.2004.09.034
Farhang MA, Dehgan P, Jahangiry L (2018) Mental health problems in relation to eating behavior patterns, nutrient intakes and health related quality of life among Iranian female adolescents. PLoS One 13(4):e0195669. https://doi.org/10.1371/journal.pone.0195669
Huang CJ, Hu HT, Fan YC et al (2010) Association of breakfast skipping with obesity and health-related quality of life: evidence from a national survey in Taiwan. Int J Obes 34(4):720–725. https://doi.org/10.1038/ijo.2009.285
Yi Y-H, Kim Y-J, Lee S-Y, Lee J-G, Jeong D-W, Cho Y-H et al (2015) The correlation of meal frequency and nutrition with mental health status in women aged 20–39 years: the 5th Korea National Health and Nutrition Examination Survey, 2010–2012. Korean J Obes 24(2):101 107. https://doi.org/10.7570/kjo.2015.24.2.101
Seremet N, Karaagaoglu N, Kaner G, Tel K (2015) Gastroesophageal reflux symptoms and nutritional preferences. Ethno Med 9(3):305–318. https://doi.org/10.1080/09735070.2015.11905448
Casucci G, Terlizzi R, Cevoil S (2014) Headache in school age. Neurol Sci 35:31–35. https://doi.org/10.1007/s10072-014-1738-0
Torelli P, Evangelista A, Bini A et al (2009) Fasting headache: a review of the literature and new hypotheses. J Headache Pain 49(5):744–752. https://doi.org/10.1111/j.1526-4610.2009.01390.x
Lim SL, Canavarro C, Zaw MH et al (2012) Irregular meal timing is associated with helicobacter pylori infection and gastritis. ISRN Nutr 2013, https://doi.org/10.5402/2013/714970(eCollection 2013)
Fujiwara Y, Machida A, Watanabe Y et al (2005) Association between dinner-to-bed time and gastro-esophageal reflux disease. Am J Gastroenterol 100:2633–2636. https://doi.org/10.1111/j.1572-0241.2005.00354.x
Acknowledgements
This nationwide survey was performed in Iran with cooperation of Ministry of Education and Training, the Ministry of Health and Medical Education, the Child Health Promotion Research Center, the Isfahan University of Medical Sciences and the Endocrinology and Metabolism Research Center of Tehran University.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
Study protocols were approved by the Ethics committee of Isfahan University of Medical Sciences, Project number: 194049.
Informed consent
After complete explanation of the study objectives and protocols, written and verbal informed consent was obtained from the parents and students, respectively.
Rights and permissions
About this article
Cite this article
Azemati, B., Heshmat, R., Qorbani, M. et al. Association of meal skipping with subjective health complaints in children and adolescents: the CASPIAN-V study. Eat Weight Disord 25, 241–246 (2020). https://doi.org/10.1007/s40519-018-0559-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40519-018-0559-1