Abstract
Purpose of review
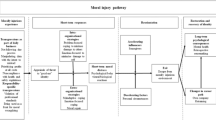
High-risk occupation workers (HROWs) are often exposed to potentially morally injurious events (PMIEs) which can contribute to moral distress (MD) or moral injury (MI). Moral resilience (MR) has been proposed as a protective or moderating factor to protect HROWs from harm caused by PMIE exposures. The current review was designed to (1) update the definition of MR to a broader context of HROWs, (2) identify components of MR for HROWs, and (3) determine demographic variables that may impact MR development.
Recent findings
The existing research on MR primarily focuses on healthcare workers; research on other high-risk occupations is sparse.
Summary
An updated definition of MR was constructed and proposed for HROWs. A review of the existing literature identified six themes related to MR in HROWs (i.e., self-care, self-regulation, moral compass, moral courage, communication, and social support at work), alongside three key demographic variables (i.e., experience, religion/spirituality, gender/sex). Further research is needed on the strategies used by demographically diverse HROWs to develop MR and protect from or moderate PMIEs, MD, and MI.


Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Litz BT, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, et al. Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695–706. https://doi.org/10.1016/j.cpr.2009.07.003.
Rodrigues S, Mercier J-M, McCall A, Nannarone M, Sedge P, Wilson J, et al. Against everything that got you into the job: experiences of potentially morally injurious events among Canadian public safety personnel. Eur J Psychotraumatol. 2023;14(1):2205332. https://doi.org/10.1080/20008066.2023.2205332.
Shay J, Jurist EL. Moral injury. Psychoanal Psychol. 2014;31(2):182–91. https://doi.org/10.1037/a0036090.
Smith-MacDonald L, Lentz L, Malloy D, Brémault-Phillips S, Carleton RN. Meat in a seat: a grounded theory study exploring moral injury in Canadian public safety communicators, firefighters, and paramedics. Int J Environ Res Public Health. 2021;18(22):12145. https://doi.org/10.3390/ijerph182212145.
McCarthy J, Gastmans C. Moral distress: a review of the argument-based nursing ethics literature. Nurs Ethics. 2015;22(1):131–52. https://doi.org/10.1177/0969733014557139.
Riedel P-L, Kreh A, Kulcar V, Lieber A, Juen B. A scoping review of moral stressors, moral distress and moral injury in healthcare workers during COVID-19. Int J Environ Res Public Health. 2022;19(3):1666. https://doi.org/10.3390/ijerph19031666.
Fourie C. Moral distress and moral conflict in clinical ethics. Bioeth. 2015;29(2):91–7. https://doi.org/10.1111/bioe.12064.
Hines SE, Chin KH, Glick DR, Wickwire EM. Trends in moral injury, distress, and resilience factors among healthcare workers at the beginning of the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(2):488. https://doi.org/10.3390/ijerph18020488.
Corley MC, Elswick RK, Gorman M, Clor T. Development and evaluation of a moral distress scale. J Adv Nurs. 2001;33(2):250–6. https://doi.org/10.1111/j.1365-2648.2001.01658.x.
Barr P. Moral distress and considering leaving in NICU nurses: direct effects and indirect effects mediated by burnout and the hospital ethical climate. Neonatology. 2021;117(5):646–9. https://doi.org/10.1159/000509311.
Dzeng E, Curtis JR. Understanding ethical climate, moral distress, and burnout: a novel tool and a conceptual framework. BMJ Qual Saf. 2018;27(10):766–70. https://doi.org/10.1136/bmjqs-2018-007905.
Lake ET, Narva AM, Holland S, Smith JG, Cramer E, Rosenbaum KEF, et al. Hospital nurses’ moral distress and mental health during COVID-19. J Adv Nurs. 2022;78(3):799–809. https://doi.org/10.1111/jan.15013.
Oh Y, Gastmans C, Peter E. Moral distress experienced by nurses: a quantitative literature review. Nurs Ethics. 2015;22(1):15–31. https://doi.org/10.1177/0969733013502803.
American Psychological Association. High risk jobs and high risk populations. American Psychological Association; 2011. https://www.apa.org/wsh/past/2011/high-risk-jobs. Accessed 15 May 2023
Brassington K, Lomas T. Can resilience training improve well-being for people in high-risk occupations? A systematic review through a multidimensional lens. J Posit Psychol. 2021;16(5):573–92. https://doi.org/10.1080/17439760.2020.1752783.
Britt TW, Jennings KS, Cheung JH, Pury CLS, Zinzow HM, Raymond MA, et al. Determinants of mental health treatment seeking among soldiers who recognize their problem: implications for high-risk occupations. Work Stress. 2016;30(4):318–36. https://doi.org/10.1080/02678373.2016.1246490.
Lentz L, Smith-MacDonald L, Malloy D, Carleton RN, Brémault-Phillips S. Compromised conscience: a scoping review of moral injury among firefighters, paramedics, and police officers. Front Psychol. 2021;12:639781. https://doi.org/10.3389/fpsyg.2021.639781.
Maftei A, Holman A-C. The prevalence of exposure to potentially morally injurious events among physicians during the COVID-19 pandemic. Eur J Psychotraumatol. 2021;12(1):1898791. https://doi.org/10.1080/20008198.2021.1898791.
Hansen KT, Nelson CG, Kirkwood K. Prevalence of potentially morally injurious events in operationally deployed Canadian Armed Forces Members. J Trauma Stress. 2021;34(4):764–72. https://doi.org/10.1002/jts.22710.
Rodrigues S, Mercier J-M, Nannarone M, McCall A, Farrell S, Sedge P, et al. Experiences of moral injury in Canadian public safety personnel. Ottawa: Atlas Institute for Veterans and Families; 2022.
Soffer-Elnekave R, Haight W, Nashandi NJC, Cho M, Suleiman J, Park S. Re-orienting narratives of moral injury towards positive development: the experiences of emerging adults with child welfare histories. Child Youth Serv Rev. 2023:149. https://doi.org/10.1016/j.childyouth.2023.106922.
Young PD, Rushton CH. A concept analysis of moral resilience. Nurs Outlook. 2017;65(5):579–87. https://doi.org/10.1016/j.outlook.2017.03.009.
Labrague LJ. Psychological resilience, coping behaviours and social support among health care workers during the COVID-19 pandemic: a systematic review of quantitative studies. J Nurs Manag. 2021;29(7):1893–905. https://doi.org/10.1111/jonm.13336.
Nishimi K, Choi KW, Cerutti J, Powers A, Bradley B, Dunn EC. Measures of adult psychological resilience following early-life adversity: how congruent are different measures? Psychol Med. 2021;51(15):2637–46. https://doi.org/10.1017/S0033291720001191.
Sala Defilippis TML, Curtis K, Gallagher A. Moral resilience through harmonised connectedness in intensive care nursing: a grounded theory study. Intensive Crit Care Nurs. 2020;57:102785. https://doi.org/10.1016/j.iccn.2019.102785.
Rushton CH. Moral resilience: a capacity for navigating moral distress in critical care. AACN Adv Crit Care. 2016;27(1):111–9. https://doi.org/10.4037/aacnacc2016275.
Kreh A, Brancaleoni R, Magalini SC, Chieffo DPR, Flad B, Ellebrecht N, et al. Ethical and psychosocial considerations for hospital personnel in the Covid-19 crisis: moral injury and resilience. PloS One. 2021;16(4):e0249609. https://doi.org/10.1371/journal.pone.0249609.
Wang Z, Koenig HG, Tong Y, Wen J, Sui M, Liu H, et al. Moral injury in Chinese health professionals during the COVID-19 pandemic. Psychol Trauma: Theory Res Pract Policy. 2022;14(2):250–7. https://doi.org/10.1037/tra0001026.
• Rushton CH, Thomas TA, Antonsdottir IM, Nelson KE, Boyce D, Vioral A, et al. Moral injury and moral resilience in health care workers during the COVID-19 pandemic. J Palliat Med. 2022;25(5):712–9. https://doi.org/10.1089/jpm.2021.0076. This paper looked at MI and MR during the COVID-19 pandemic but only among nursing professionals and the current study reviewed MR components pre and post COVID-19 pandemic
Spilg EG, Rushton CH, Phillips JL, Kendzerska T, Saad M, Gifford W, et al. The new frontline: exploring the links between moral distress, moral resilience and mental health in healthcare workers during the COVID-19 pandemic. BMC Psychiatry. 2022;22(1):19. https://doi.org/10.1186/s12888-021-03637-w.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. https://doi.org/10.1080/1364557032000119616.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. https://doi.org/10.7326/M18-0850.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74. https://doi.org/10.2307/2529310.
Brewer K, Ziegler H, Kurdian S, Nguyen J. Relationships of individual and workplace characteristics with nurses’ moral resilience. Nurs Ethics. 2023:9697330231161692–2. https://doi.org/10.1177/09697330231161692.
• Faraco MM, Gelbcke FL, Brehmer LC, Ramos FR, Schneider DG, Silveira LR. Moral distress and moral resilience of nurse managers. Nurs Ethics. 2022;29(5):1253–65. https://doi.org/10.1177/09697330221085770. This article was where the idea of individual and team-based components of MR was developed which is built on in the current scoping review.
Helmers A, Palmer KD, Greenberg RA. Moral distress: developing strategies from experience. Nurs Ethics. 2020;27(4):1147–56. https://doi.org/10.1177/0969733020906593.
Holtz HK, Weissinger GM, Swavely D, Lynn L, Yoder A, Cotton B, et al. The long tail of COVID-19: implications for the future of emergency nursing. J Emerg Nurs. 2023;49(2):198–209. https://doi.org/10.1016/j.jen.2022.10.006.
Monteverde S. Caring for tomorrow’s workforce: moral resilience and healthcare ethics education. Nurs Ethics. 2016;23(1):104–16. https://doi.org/10.1177/0969733014557140.
Varasteh S, Esmaeili M, Navid Hamidi M, Ebadi A. Explaining the concept of moral resilience among intensive care unit nurses. Nurs Ethics. 2023:9697330221140481. https://doi.org/10.1177/09697330221140481.
•• Holtz H, Heinze K, Rushton C. Interprofessionals’ definitions of moral resilience. J Clin Nurs. 2018;27(3-4):e488–94. https://doi.org/10.1111/jocn.13989. This article discusses common themes within moral resilience including buoyancy, personal, and relational integrity, which were built into the major themes within the current scoping review.
Richard AA, Shea K. Delineation of self-care and associated concepts. J Nurs Scholarsh. 2011;43(3):255–64. https://doi.org/10.1111/j.1547-5069.2011.01404.x.
Dos Santos MR, da Silva LTP, de Araújo MM, Ferro TA, Silva IN, Szylit R. Ethical and moral conflicts in the nursing care of pediatric patients with cancer and their families. Cancer Nurs. 2022;46(4):314–20. https://doi.org/10.1097/NCC.0000000000001113.
Baker-Townsend J, Cummings C. Incorporating moral resilience into an undergraduate nursing program. Arch Psychiatr Nurs. 2020;34(5):391–3. https://doi.org/10.1016/j.apnu.2020.06.001.
•• Jacobs G. God hey, now i’ve been through something.: moral resilience of coordinators in voluntary palliative terminal care. J Hosp Palliat Nurs. 2022;24(4):E144–50. https://doi.org/10.1097/NJH.0000000000000868. This article discussed strategies used to manage PMIEs, MD, and MI included within multiple sub-themes in the current scoping review including seeking dialogue, looking for alternative solutions to workplace challenges, seeking support, emotion regulation, and cognitive reconstruction.
• Jansen T-L, Hem MH, Danbolt LJ, Hanssen I. Coping with moral distress on acute psychiatric wards: a qualitative study. Nurs Ethics. 2022;29(1):171–80. https://doi.org/10.1177/09697330211010246. This article was important as major themes were included as sub-themes in the current scoping review including mentally sorting ethical dilemmas, bringing ethical dilemmas to leadership, and the idea of peer support.
Berdida DJE, Grande RAN. Moral distress, moral resilience, moral courage, and moral injury among nurses in the Philippines during the COVID-19 pandemic: a mediation analysis. J Relig Health. 2023; https://doi.org/10.1007/s10943-023-01873-w.
Morley G, Copley DJ, Field R, Zelinsky M, Albert NM. RESPONDER: a qualitative study of ethical issues faced by critical care nurses during the COVID-19 pandemic. J Nurs Manag. 2022;30(7):2403–15. https://doi.org/10.1111/jonm.13792.
Stevenson RM. Brief mindfulness training for Canadian public safety personnel well-being. J Community Saf Well Being. 2022;7(3):88–92. https://doi.org/10.35502/jcswb.263.
Jamieson N, Usher K, Maple M, Ratnarajah D. Invisible wounds and suicide: moral injury and veteran mental health. Int J Ment Health Nurs. 2020;29(2):105–9. https://doi.org/10.1111/inm.12704.
Lachman VD. Moral resilience: managing and preventing moral distress and moral residue. Medsurg Nurs. 2016;25(2):121–4.
Gibson E, Duke G, Alfred D. Exploring the relationships among moral distress, moral courage, and moral resilience in undergraduate nursing students. J Nurs Educ. 2020;59(7):392–5. https://doi.org/10.3928/01484834-20200617-07.
• Rushton CH, Nelson KE, Antonsdottir IM, Hanson GC, Boyce D. Perceived organizational effectiveness, moral injury, and moral resilience among nurses during the COVID-19 pandemic: secondary analysis. Nurs Manag. 2022;53(7):12–22. https://doi.org/10.1097/01.NUMA.0000834524.01865.cc. This paper examined MI and MR during the COVID-19 pandemic but only among nursing professionals and the current study reviewed MR components pre and post COVID-19 pandemic. This paper fostered the idea that examining MR before, during, and after the COVID-19 pandemic is important.
Graeme BG, Dimbleby R. Between ourselves: an introduction to interpersonal communication. London: Hodder Education; 2006.
Sippel LM, Pietrzak RH, Charney DS, Mayes LC, Southwick SM. How does social support enhance resilience in the trauma-exposed individual? Ecol Soc. 2015;20(4):10. https://doi.org/10.5751/ES-07832-200410.
Doğru Ç. Meta-analysis of antecedents and consequences of empowering employees as a contemporary management approach. In: Handbook of Research on Contemporary Approaches in Management and Organizational Strategy. Hershey: IGI Global; 2018. p. 1–17.
Edmondson AC, Lei Z. Psychological safety: the history, renaissance, and future of an interpersonal construct. Annu Rev Organ Psychol Organ Behav. 2014;1(1):23–43. https://doi.org/10.1146/annurev-orgpsych-031413-091305.
Antonsdottir I, Rushton CH, Nelson KE, Heinze KE, Swoboda SM, Hanson GC. Burnout and moral resilience in interdisciplinary healthcare professionals. J Clin Nurs. 2022;31(1-2):196–208. https://doi.org/10.1111/jocn.15896.
Arries-Kleyenstüber EJ. Moral resilience in nursing education: exploring undergraduate nursing students’ perceptions of resilience in relation to ethical ideology. SAGE Open Nurs. 2021;7:23779608211017798. https://doi.org/10.1177/23779608211017798.
Kovanci MS, Atli ÖA. Examining the effect of moral resilience on moral distress. Nurs Ethics. 2023:9697330231177420. https://doi.org/10.1177/09697330231177420.
Hossain F, Clatty A. Self-care strategies in response to nurses’ moral injury during COVID-19 pandemic. Nurs Ethics. 2021;28(1):23–32. https://doi.org/10.1177/0969733020961825.
Gross J. The extended process model of emotion regulation: elaborations, applications, and future directions. Psychol Inq. 2015;26(1):130–7. https://doi.org/10.1080/1047840X.2015.989751.
Tang E, Jones C, Smith-MacDonald L, Brown MRG, Vermetten EHGJM, Brémault-Phillips S. Decreased emotional dysregulation following multi-modal motion-assisted memory desensitization and reconsolidation therapy (3MDR): identifying possible driving factors in remediation of treatment-resistant PTSD. Int J Environ Res Public Health. 2021;18(22):12243. https://doi.org/10.3390/ijerph182212243.
Barratt C. Developing resilience: the role of nurses, healthcare teams and organizations. Nurs Stand. 2018;33(7):43–9. https://doi.org/10.7748/ns.2018.e11231.
Walser RD, Wharton E. Acceptance and commitment therapy: using mindfulness and values in the treatment of moral injury. In: Currier JM, Drescher KD, Nieuwsma J, editors. Addressing moral injury in clinical practice. Washington: American Psychological Association; 2021. p. 163–81. https://doi.org/10.1037/0000204-010.
Hamrick HC, Kelley ML, Bravo AJ. Morally injurious events, moral injury, and suicidality among recent-era veterans: the moderating effects of rumination and mindfulness. Mil Behav Health. 2020;8(1):109–20. https://doi.org/10.1080/21635781.2019.1669509.
Roth SL, Andrews K, Protopopescu A, Lloyd C, O'Connor C, Losier BJ, et al. Development and preliminary evaluation of the moral injury assessment for public safety personnel. Traumatology. 2023;29(2):301–8. https://doi.org/10.1037/trm0000367.
Pajakoski E, Rannikko S, Leino-Kilpi H, Numminen O. Moral courage in nursing– an integrative literature review. Nurs Health Sci. 2021;23:570–85. https://doi.org/10.1111/nhs.12805.
Lützén K, Ewalds-Kvist B. Moral distress and its interconnection with moral sensitivity and moral resilience: viewed from the philosophy of Viktor E. Frankl. J Bioeth Inq. 2013;10(3):317–24. https://doi.org/10.1007/s11673-013-9469-0.
Alderson-Day B, Fernyhough C. Inner speech: development, cognitive functions, phenomenology, and neurobiology. Psychol Bull. 2015;141:931–65. https://doi.org/10.1037/bul0000021.
Masten AS. Global perspectives on resilience in children and youth. Child Dev. 2014;85(1):6–20. https://doi.org/10.1111/cdev.12205.
Pauly B, Varcoe C, Storch J, Newton L. Registered nurses’ perceptions of moral distress and ethical climate. Nurs Ethics. 2009;16(5):561–73. https://doi.org/10.1177/0969733009106649.
Webb EL, Ireland JL, Lewis M, Morris D. Potential sources of moral injury for healthcare workers in forensic and psychiatric settings: a systematic review and meta-ethnography. Trauma Violence Abuse. 2023; https://doi.org/10.1177/15248380231167390.
Donovan N. Peer support facilitates post-traumatic growth in first responders: a literature review. Trauma. 2022;24(4):277–85. https://doi.org/10.1177/14604086221079441.
Luo D, Song Y, Cai X, Li R, Bai Y, Chen B, et al. Nurse managers’ burnout and organizational support: the serial mediating role of leadership and resilience. J Nurs Manag. 2022;30(8):4251–61. https://doi.org/10.1111/jonm.13852.
Schein EH. Organizational culture and leadership. 1st ed. Hoboken: Jossey-Bass Publishers; 1985.
Shay J. Achilles in Vietnam: combat trauma and the undoing of character. New York City: Simon and Schuster; 1994.
Gayton SD, Lovell GP. Resilience in ambulance service paramedics and its relationships with well-being and general health. Traumatology. 2012;18(1):58–64. https://doi.org/10.1177/1534765610396727.
Mantri S, Song YK, Lawson JM, Berger EJ, Koenig HG. Moral injury and burnout in health care professionals during the COVID-19 pandemic. J Nerv Ment Dis. 2021;209(10):720–6. https://doi.org/10.1097/NMD.0000000000001367.
Brémault-Phillips S, Pike A, Scarcella F, Cherwick T. Spirituality and moral injury among military personnel: a mini-review. Front Psychiatry. 2019;10:276. https://doi.org/10.3389/fpsyt.2019.00276.
Ortiz L, Villereal S, Engel M. Culture and spirituality: a review of literature. Soc Thought. 2000;19(4):21–36. https://doi.org/10.1080/15426432.2000.9960272.
Baumsteiger R, Chenneville T, McGuire JF. The roles of religiosity and spirituality in moral reasoning. Ethics Behav. 2013;23(4):266–77. https://doi.org/10.1080/10508422.2013.782814.
Usset TJ, Gray E, Griffin BJ, Currier JM, Kopacz MS, Wilhelm JH, et al. Psychospiritual developmental risk factors for moral injury. Religions. 2020;11(10):484. https://doi.org/10.3390/rel11100484.
Harris JI, Park CL, Currier JM, Usset TJ, Voecks CD. Moral injury and psycho-spiritual development: considering the developmental context. Spiritual Clin Pract. 2015;2(4):256–66. https://doi.org/10.1037/scp0000045.
Shapiro JR, Klein SL, Morgan R. Stop controlling for sex and gender in global health research. BMJ Glob Health. 2021;6(4):e005714. https://doi.org/10.1136/bmjgh-2021-005714.
Heidari S, Babor TF, de Castro P, Tort S, Curno M. Sex and gender equity in research: rationale for the SAGER guidelines and recommended use. Res Integr Peer Rev. 2016;1(1):1–9. https://doi.org/10.1186/S41073-016-0007-6.
Funding
This work was supported by the Supporting Psychological Health in First Responders Grant from the Government of Alberta (grant number: 21SPHIFR30-2).
Author information
Authors and Affiliations
Contributions
The authors Temitope Osifeso, Sierra J. Crocker, Liana Lentz, David Malloy, R. Nicholas Carleton, Suzette Brémault-Phillips, and Lorraine Smith-MacDonald contributed to the study creation and design. The literature search, exclusion criteria, search strategy and study selection, were conducted by Temitope Osifeso, Sierra J. Crocker, and Liana Lentz. Data extraction and synthesis were conducted by Temitope Osifeso and Sierra J. Crocker. Conceptualization of the framework was done by Temitope Osifeso. The first and main draft of the manuscript was written by Temitope Osifeso and Sierra J. Crocker, and all authors provided feedback on the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Temitope Osifeso declares that she has no conflict of interest. Sierra J. Crocker declares that she has no conflict of interest. Liana Lentz declares that she has no conflict of interest. Lorraine Smith-MacDonald declares that she has no conflict of interest. Merna Seliman declares that she has no conflict of interest. Gojjam Limenih declares that she has no conflict of interest. Renée S. MacPhee declares that she has no conflict of interest. Gregory S. Anderson declares that he has no conflict of interest. Suzette Brémault-Phillips declares that she has no conflict of interest. David Malloy declares that he has no conflict of interest. R. Nicholas Carleton declares that he has no conflict of interest.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sierra J. Crocker is a co-first author.
Supplementary information
ESM 1
(DOCX 13 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Osifeso, T., Crocker, S.J., Lentz, L. et al. A Scoping Review of the Components of Moral Resilience: Its Role in Addressing Moral Injury or Moral Distress for High-Risk Occupation Workers. Curr Treat Options Psych 10, 463–491 (2023). https://doi.org/10.1007/s40501-023-00310-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40501-023-00310-9