Abstract
Purpose of review
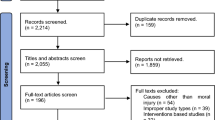
The goals of this report were to (a) review the empirical evidence of interventions for moral injury syndrome (MIS) symptoms, (b) quantitatively synthesize these effects through a preliminary meta-analysis, and (c) provide treatment and research recommendations for MIS based on our qualitative and quantitative review.
Recent findings
Participants in MIS treatment improved on targeted MIS symptoms and general mental health, with scores decreasing across measured adverse mental health outcomes compared to control conditions. Increased scores on positive outcomes such as self-forgiveness were also reported. Meta-analysis revealed significant omnibus effects across mental health symptoms (g = − 0.60), positive outcomes (g = − 0.51), and hallmark MIS symptom (g = − 0.51) domains. There were robust mixed treatment effects for PTSD (g = − 0.61) and depression (g = − 0.47) specific outcomes. While control samples also improved on PTSD (g = − 0.37) and hallmark MIS symptoms (g = − 0.34) across within-group models, stronger within-group treatment effects for these domains/subdomains (g = − 0.71 and − 0.63, respectively) indicate that EBTs for MIS are more useful for targeting these symptoms than traditional trauma treatments or waitlist conditions.
Summary
Empirically supported treatments for MIS symptoms are effective in reducing negative impact of MIS to mental health. As EBTs for MIS treat PTSD to a comparable degree as conventional trauma treatments, and are superior in attenuating MIS symptoms, we recommend expanding access to MIS treatments.




Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
Jinkerson JD. Defining and assessing moral injury: a syndrome perspective. Traumatology. 2016;22(2):122–30. https://doi.org/10.1037/trm0000069.
Litz BT, Stein N, Delaney E, et al. Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clin Psychol Rev. 2009;29(8):695–706. https://doi.org/10.1016/j.cpr.2009.07.003.
Mantri S, Lawson JM, Wang Z, Koenig HG. Prevalence and predictors of moral injury symptoms in health care professionals. J Nerv Ment Dis. 2021;209(3):174–80. https://doi.org/10.1097/NMD.0000000000001277.
• Maguen S, Griffin BJ, Vogt D, et al. Moral injury and peri- and post-military suicide attempts among post-9/11 veterans. Psychol Med. 2023;53(7):3200–3209. https://doi.org/10.1017/S0033291721005274.
Gibbons SW, Shafer M, Hickling EJ, Ramsey G. How do deployed health care providers experience moral injury? Narrat Inq Bioeth. 2013;3(3):247–59. https://doi.org/10.1353/nib.2013.0055.
Nieuwsma JA, O’Brien EC, Xu H, et al. Patterns of potential moral injury in post-9/11 combat veterans and COVID-19 healthcare workers. J Gen Intern Med. 2022;37(8):2033–40. https://doi.org/10.1007/s11606-022-07487-4.
Bryan CJ, Bryan AO, Roberge E, Leifker FR, Rozek DC. Moral injury, posttraumatic stress disorder, and suicidal behavior among national guard personnel. Psychol Trauma. 2018;10(1):36–45. https://doi.org/10.1037/tra0000290.
Norman SB, Capone C, Panza KE, et al. A clinical trial comparing trauma-informed guilt reduction therapy (TrIGR), a brief intervention for trauma-related guilt, to supportive care therapy. Depress Anxiety. 2022;39(4):262–73. https://doi.org/10.1002/da.23244.
• Weber MC, Smith AJ, Jones RT, et al. Moral injury and psychosocial functioning in health care workers during the COVID-19 pandemic. Psychol Serv. 2023;20(1):19–29. https://doi.org/10.1037/ser0000718. Recent study on impact of moral injury on healthcare workers.
• Nichter B, Norman SB, Maguen S, Pietrzak RH. Moral injury and suicidal behavior among US combat veterans: results from the 2019–2020 National Health and Resilience in Veterans Study. Depress Anxiety. 2021;38(6):606–14. https://doi.org/10.1002/da.23145. Recent study on the impact of moral injury on suicide risk.
Ames D, Erickson Z, Youssef NA, et al. Moral injury, religiosity, and suicide risk in US veterans and active-duty military with PTSD symptoms. Mil Med. 2018;184(3–4):e271–8. https://doi.org/10.1093/milmed/usy148.
Currier JM, Holland JM, Drescher KD. Spirituality factors in the prediction of outcomes of PTSD treatment for U.S. military veterans. J Trauma Stress. 2015;28(1):57–64.
Glynn SM. Family-centered care to promote successful community reintegration after war: it takes a nation. Clin Child Fam Psychol Rev. 2013;16(4):410–4. https://doi.org/10.1007/s10567-013-0153-z.
Harris JI, Erbes CR, Winskowski AM, Engdahl BE, Nguyen XV. Social support as a mediator in the relationship between religious comforts and strains and trauma symptoms. Psycholog Relig Spiritual. 2014;6(3):223. https://doi.org/10.1037/a0036421.
Nillni YI, Shayani DR, Finley E, Copeland LA, Perkins DF, Vogt DS. The impact of posttraumatic stress disorder and moral injury on women veterans’ perinatal outcomes following separation from military service. J Trauma Stress. 2020;33(3):248–56. https://doi.org/10.1002/jts.22509.
Harris JI, Meis L, Cheng ZH, Voecks C, Usset T, Sherman M. Spiritual distress and dyadic adjustment in veterans and partners managing PTSD. Spiritual Clin Pract. 2017;4(4):229–37. https://doi.org/10.1037/scp0000143.
Sherman MD, Usset T, Voecks C, Harris JI. Roles of religion and spirituality among veterans who manage PTSD and their partners. Psycholog Relig Spiritual. 2018;10(4):368–74. https://doi.org/10.1037/rel0000159.
Hendrickson RC, Slevin RA, Hoerster KD, Chang BP, Sano E, McCall CA, Monty GR, Thomas RG, Raskind MA. The impact of the COVID-19 pandemic on mental health, occupational functioning, and professional retention among health care workers and first responders. J Gen Intern Med. 2022;37(2):397–408. https://doi.org/10.1007/s11606-021-07252-z.
Raines AM, Currier J, McManus ES, Walton JL, Uddo M, Franklin CL. Spiritual struggles and suicide in veterans seeking PTSD treatment. Psychol Trauma. 2017;9(6):746–9. https://doi.org/10.1037/tra0000239.
Jones KA, Freijah I, Carey L, Carleton RN, Devenish-Meares P, Dell L, Rodrigues S, Madden K, Johnson L, Hosseiny F, Phelps AJ. Moral injury, chaplaincy and mental health provider approaches to treatment: a scoping review. J Relig Health. 2022;61:1051–94. https://doi.org/10.1007/s10943-022-01534-4.
Kondrath SR. Moral injury and spiritual distress: clinical applications in interdisciplinary, spiritually integrated interventions. Curr Treat Options Psych. 2022;9:126–39. https://doi.org/10.1007/s40501-022-00263-5.
National Institutes of Health. Study quality assessment tools. National Heart, Lung, and Blood Institute. 2021. Accessed August 15, 2021. Retrieved from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive meta-analysis version 4. 2022. Biostat, Englewood, NJ.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. introduction to meta-analysis. John Wiley & Sons. 2009. https://doi.org/10.1002/9780470743386.
Field AP, Gillett R. How to do a meta-analysis. Br J Math Stat Psychol. 2010;63(3):665–94. https://doi.org/10.1348/000711010X502733.
Hunter JE, Schmidt FL. Methods of meta-analysis: correcting error and bias in research findings. 3rd ed. London: Sage; 2015. https://doi.org/10.4135/9781483398105.
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I 2 Index? Psychol Methods. 2006;11(2):193–206. https://doi.org/10.1037/1082-989X.11.2.193.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane Handbook for systematic reviews of interventions. (2nd ed). Oxford: Wiley-Blackwell 2019. https://doi.org/10.1002/9781119536604.
Zakzanis KK. Statistics to tell the truth, the whole truth, and nothing but the truth: Formulae, illustrative numerical examples, and heuristic interpretation of effect size analyses for neuropsychological researchers. Arch Clin Neuropsychol. 2001;16(7):653–67. https://doi.org/10.1093/arclin/16.7.653.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New York: Routledge; 1988. https://doi.org/10.4324/9780203771587.
Ferguson CJ. An effect size primer: a guide for clinicians and researchers. Prof Psychol Res Pract. 2009;40(5):532–8. https://doi.org/10.1037/a0015808.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. 1997;315(7109):629–34. https://doi.org/10.1136/bmj.315.7109.629.
Griffin BJ, Worthington EL, Lavelock CR, et al. Efficacy of a self-forgiveness workbook: a randomized controlled trial with interpersonal offenders. J Couns Psychol. 2015;62(2):124–36. https://doi.org/10.1037/cou0000060.
Litz BT, Rusowicz-Orazem L, Doros G, et al. Adaptive disclosure, a combat-specific PTSD treatment, versus cognitive-processing therapy, in deployed Marines and sailors: a randomized controlled non-inferiority trial. Psychiatry Res. 2021;297:113761. https://doi.org/10.1016/j.psychres.2021.113761.
Maguen S, Burkman K, Madden E, et al. Impact of killing in war: a randomized, controlled pilot trial. J Clin Psychol. 2017;73(9):997–1012. https://doi.org/10.1002/jclp.22471.
Harris JI, Erbes CR, Engdahl BE, et al. The effectiveness of a trauma focused spiritually integrated intervention for veterans exposed to trauma. J Clin Psychol. 2011;67:425–38. https://doi.org/10.1002/jclp.20777.
Harris JI, Usset T, Voecks C, Thuras P, Currier J, Erbes C. Spiritually integrated care for PTSD: a randomized controlled trial of “Building Spiritual Strength.” Psychiatry Res. 2018;267:420–8. https://doi.org/10.1016/j.psychres.2018.06.045.
Van Etten ML, Taylor S. Comparative efficacy of treatments for posttraumatic stress disorder: a meta-analysis. Clin Psychol Psychother. 1998;5:126–44.
Campbell JS, Loeffler GH, Pulos S, Campbell AW. Meta-analysis of average symptom change in inpatient treatment for posttraumatic stress disorder in veteran and active duty US military samples. Psychol Serv. 2016;13(4):389. https://doi.org/10.1037/ser0000104.
Kopacz MS, Connery AL, Bishop TM, Bryan CJ, Drescher KD, Currier JM, Pigeon WR. Moral injury: a new challenge for complementary and alternative medicine. Complement Ther Med. 2016;24:29–33. https://doi.org/10.1016/j.ctim.2015.11.003.
Litz BT, Plouffe RA, Nazarov A, Murphy D, Phelps A, Coady A, Houle SA, Dell L, Frankfurt S, Zerach G, Levi-Belz Y. Moral injury outcome scale consortium. Defining and assessing the syndrome of moral injury: initial findings of the moral injury outcome scale consortium. Front Psychiatry. 2022;13:923928. https://doi.org/10.3389/fpsyt.2022.923928.
Currier JM, Farnsworth JK, Drescher KD, McDermott RC, Sims BM, Albright DL. Development and evaluation of the expressions of moral injury scale-military version. Clin Psychol Psychother. 2018;25(3):474–88. https://doi.org/10.1002/cpp.2170.
Taylor S. Assessment of obsessions and compulsions: reliability, validity, and sensitivity to treatment effects. Clin Psychol Review. 1995;15(4):261–96. https://doi.org/10.1016/0272-7358(95)00015-H.
Lambert MJ, Hatch DR, Kingston MD, Edwards BC. Zung, Beck, and Hamilton Rating Scales as measures of treatment outcome: a meta-analytic comparison. J Consult Clin Psychol. 1986;54(1):54–9. https://doi.org/10.1037/0022-006X.54.1.54.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aita, S.L., Kondrath, S.R., Owen, T. et al. The Status of Evidence-Based Treatments for Moral Injury Syndrome: Review and Meta-analysis of Randomized Controlled Trials. Curr Treat Options Psych 10, 217–233 (2023). https://doi.org/10.1007/s40501-023-00292-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40501-023-00292-8