Abstract
Purpose of review
To evaluate the impact of healthy dietary patterns compared to the Western diet on periodontal indices in adults, used in the prevention and treatment of periodontal diseases.
Recent findings
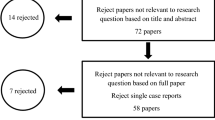
Four RCTs and seven case–control studies were included on a critical appraisal of the evidence using GRADE, based on random effects meta-analysis by methodological subgroups for periodontal indices, and a narrative synthesis. There is a clinically significant reduction on bleeding on probing, Gingival Index and periodontal inflamed surface area, Calculus and Debris Index and incidence of tooth loss on healthy dietary patterns group, with a very low to moderate certainty of the evidence. Methodological complementation between included studies allows to consider “real-world data” that RCTs ignore, which have a significant effect on this association. Although biological plausibility is reported, more studies are required to clarify these results.
Summary
healthy dietary patterns could impact on periodontal health–disease status, reducing the global burden of periodontal diseases by improving the results of the standard care actions, such as toothbrushing, interdental cleaning and periodontal therapy. Further research is required to improve the quality of the evidence.










Similar content being viewed by others
References
Peres MA, Macpherson LMD, Weyant RJ, Daly B, Venturelli R, Mathur MR, et al. Oral diseases: a global public health challenge. Lancet. 2019;394(10194):249–60. https://doi.org/10.1016/s0140-6736(19)31146-8.
Bennett JE, Stevens GA, Mathers CD, Bonita R, Rehm J, Kruk ME, et al. NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet. 2018;392(10152):1072–88. https://doi.org/10.1016/s0140-6736(18)31992-5.
Tonetti MS, Jepsen S, Jin L, Otomo-Corgel J. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: A call for global action. J Clin Periodontol. 2017;44(5):456–62. https://doi.org/10.1111/jcpe.12732.
Martini D, Godos J, Bonaccio M, Vitaglione P, Grosso G. Ultra-Processed Foods and Nutritional Dietary Profile: A Meta-Analysis of Nationally Representative Samples. Nutrients. 2021;13(10):3390. https://doi.org/10.3390/nu13103390.
Christ A, Lauterbach M, Latz E. Western Diet and the Immune System: An Inflammatory Connection. Immunity. 2019;51(5):794–811. https://doi.org/10.1016/j.immuni.2019.09.020.
Al-Zahrani MS, Borawski EA, Bissada NF. Poor Overall Diet Quality as a Possible Contributor to Calculus Formation. Oral Health Prev Dent. 2004;2(4):345–9. https://doi.org/10.3290/j.ohpd.a9761.
Baumgartner S, Imfeld T, Schicht O, Rath C, Persson RE, Persson GR. The impact of the stone age diet on gingival conditions in the absence of oral hygiene. J Periodontol. 2009;80(5):759–68. https://doi.org/10.1902/jop.2009.080376.
Bawadi HA, Khader YS, Haroun TF, Al-Omari M, Tayyem RF. The association between periodontal disease, physical activity and healthy diet among adults in Jordan. J Periodontal Res. 2011;46(1):74–81. https://doi.org/10.1111/j.1600-0765.2010.01314.x.
Jauhiainen LM, Ylostalo PV, Knuuttila M, Mannisto S, Kanerva N, Suominen AL. Poor diet predicts periodontal disease development in 11-year follow-up study. Community Dent Oral Epidemiol. 2020;48(2):143–51. https://doi.org/10.1111/cdoe.12513.
Pulikkotil SJ, Nath S, Ramachandran V. Determinants of periodontitis among a rural Indian population: A case control study. Commun Dent Health. 2020;37(1):26–31. https://doi.org/10.1922/CDH_4632Pulikkotil06.
Salazar CR, Laniado N, Mossavar-Rahmani Y, Borrell LN, Qi Q, Sotres-Alvarez D, et al. Better-quality diet is associated with lower odds of severe periodontitis in US Hispanics/Latinos. J Clin Periodontol. 2018;45(7):780–90. https://doi.org/10.1111/jcpe.12926.
O’Connor JP, Milledge KL, O’Leary F, Cumming R, Eberhard J, Hirani V. Poor dietary intake of nutrients and food groups are associated with increased risk of periodontal disease among community-dwelling older adults: a systematic literature review. Nutr Rev. 2020;78(2):175–88. https://doi.org/10.1093/nutrit/nuz035.
Abdelhamid AS, Brown TJ, Brainard JS, Biswas P, Thorpe GC, Moore HJ, et al. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev 2018;7:CD003177. https://doi.org/10.1002/14651858.CD003177.pub3.
Schulze MB, Martinez-Gonzalez MA, Fung TT, Lichtenstein AH, Forouhi NG. Food based dietary patterns and chronic disease prevention. BMJ. 2018;361: k2396. https://doi.org/10.1136/bmj.k2396.
Kahleova H, Salas-Salvado J, Rahelic D, Kendall CW, Rembert E, Sievenpiper JL. Dietary Patterns and Cardiometabolic Outcomes in Diabetes: A Summary of Systematic Reviews and Meta-Analyses. Nutrients. 2019;11:9. https://doi.org/10.3390/nu11092209.
Menzel J, Biemann R, Longree A, Isermann B, Mai K, Schulze MB, et al. Associations of a vegan diet with inflammatory biomarkers. Sci Rep. 2020;10(1):1933. https://doi.org/10.1038/s41598-020-58875-x.
Ramezani-Jolfaie N, Mohammadi M, Salehi-Abargouei A. The effect of healthy Nordic diet on cardio-metabolic markers: a systematic review and meta-analysis of randomized controlled clinical trials. Eur J Nutr. 2019;58(6):2159–74. https://doi.org/10.1007/s00394-018-1804-0.
Yokoyama Y, Levin SM, Barnard ND. Association between plant-based diets and plasma lipids: a systematic review and meta-analysis. Nutr Rev. 2017;75(9):683–98. https://doi.org/10.1093/nutrit/nux030.
Schwingshackl L, Chaimani A, Hoffmann G, Schwedhelm C, Boeing H. A network meta-analysis on the comparative efficacy of different dietary approaches on glycaemic control in patients with type 2 diabetes mellitus. Eur J Epidemiol. 2018;33(2):157–70. https://doi.org/10.1007/s10654-017-0352-x.
Lu J-W, Yu L-H, Tu Y-K, Cheng H-Y, Chen L-Y, Loh C-H, et al. Risk of Incident Stroke among Vegetarians Compared to Nonvegetarians: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutrients. 2021;13(9):3019. https://doi.org/10.3390/nu13093019.
Fageeh HN, Fageeh HI, Prabhu A, Bhandi S, Khan S, Patil S. Efficacy of vitamin C supplementation as an adjunct in the non-surgical management of periodontitis: a systematic review. Syst Rev. 2021;10(1):5. https://doi.org/10.1186/s13643-020-01554-9.
Cagetti MG, Wolf TG, Tennert C, Camoni N, Lingstrom P, Campus G. The Role of Vitamins in Oral Health. A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2020;17:3. https://doi.org/10.3390/ijerph17030938.
Jockel-Schneider Y, Gossner SK, Petersen N, Stolzel P, Hagele F, Schweiggert RM, et al. Stimulation of the nitrate-nitrite-NO-metabolism by repeated lettuce juice consumption decreases gingival inflammation in periodontal recall patients: a randomized, double-blinded, placebo-controlled clinical trial. J Clin Periodontol. 2016;43(7):603–8. https://doi.org/10.1111/jcpe.12542.
Castro MML, Duarte NN, Nascimento PC, Magno MB, Fagundes NCF, Flores-Mir C, et al. Antioxidants as Adjuvants in Periodontitis Treatment: A Systematic Review and Meta-Analysis. Oxid Med Cell Longev. 2019;2019:9187978. https://doi.org/10.1155/2019/9187978.
Sparrow T v, Dodington DW, Yumol JL, Fritz PC, Ward WE. Higher intakes of flavonoids are associated with lower salivary IL-1beta and maintenance of periodontal health 3–4 years after scaling and root planing. J Clin Periodontol 2020;47(4):461–9. https://doi.org/10.1111/jcpe.13263.
Bazyar H, Gholinezhad H, Moradi L, Salehi P, Abadi F, Ravanbakhsh M, et al. The effects of melatonin supplementation in adjunct with non-surgical periodontal therapy on periodontal status, serum melatonin and inflammatory markers in type 2 diabetes mellitus patients with chronic periodontitis: a double-blind, placebo-controlled trial. Inflammopharmacology. 2019;27(1):67–76. https://doi.org/10.1007/s10787-018-0539-0.
Kruse AB, Kowalski CD, Leuthold S, Vach K, Ratka-Kruger P, Woelber JP. What is the impact of the adjunctive use of omega-3 fatty acids in the treatment of periodontitis? A systematic review and meta-analysis. Lipids Health Dis. 2020;19(1):100. https://doi.org/10.1186/s12944-020-01267-x.
Gorska-Warsewicz H, Rejman K, Laskowski W, Czeczotko M. Milk and Dairy Products and Their Nutritional Contribution to the Average Polish Diet. Nutrients. 2019;11:8. https://doi.org/10.3390/nu11081771.
DeMayo F, Molinsky R, Tahir MJ, Roy S, Genkinger JM, Papapanou PN, et al. Diet quality and periodontal disease: Results from the oral infections, glucose intolerance and insulin resistance study (ORIGINS). J Clin Periodontol. 2021;48(5):638–47. https://doi.org/10.1111/jcpe.13450.
Skoczek-Rubinska A, Bajerska J, Menclewicz K. Effects of fruit and vegetables intake in periodontal diseases: A systematic review. Dent Med Probl. 2018;55(4):431–9. https://doi.org/10.17219/dmp/99072.
Corbella S, Calciolari E, Alberti A, Donos N, Francetti L. Systematic review and meta-analysis on the adjunctive use of host immune modulators in non-surgical periodontal treatment in healthy and systemically compromised patients. Sci Rep. 2021;11(1):12125. https://doi.org/10.1038/s41598-021-91506-7.
Xu X, Shi Z, Liu G, Chang D, Inglis SC, Hall JJ, et al. The Joint Effects of Diet and Dietary Supplements in Relation to Obesity and Cardiovascular Disease over a 10-Year Follow-Up: A Longitudinal Study of 69,990 Participants in Australia. Nutrients. 2021;13(3):944. https://doi.org/10.3390/nu13030944.
Ramseier CA, Woelber JP, Kitzmann J, Detzen L, Carra MC, Bouchard P. Impact of risk factor control interventions for smoking cessation and promotion of healthy lifestyles in patients with periodontitis: A systematic review. J Clin Periodontol. 2020;47(Suppl 22):90–106. https://doi.org/10.1111/jcpe.13240.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71. https://doi.org/10.1136/bmj.n71.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358: j4008. https://doi.org/10.1136/bmj.j4008.
Loe H, Silness J. Periodontal Disease in Pregnancy. I. Prevalence and Severity. Acta Odontol Scand. 1963;21:533–51. https://doi.org/10.3109/00016356309011240.
Leira Y, Martin-Lancharro P, Blanco J. Periodontal inflamed surface area and periodontal case definition classification. Acta Odontol Scand. 2018;76(3):195–8. https://doi.org/10.1080/00016357.2017.1401659.
Silness J, Loe H. Periodontal Disease in Pregnancy. Ii. Correlation between Oral Hygiene and Periodontal Condtion. Acta Odontol Scand. 1964;22:121–35. https://doi.org/10.3109/00016356408993968.
Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975;25(4):229–35.
Schwingshackl L, Hoffmann G. Diet quality as assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension score, and health outcomes: a systematic review and meta-analysis of cohort studies. J Acad Nutr Diet. 2015;115(5):780-800.e5. https://doi.org/10.1016/j.jand.2014.12.009.
Higgins JP, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343: d5928. https://doi.org/10.1136/bmj.d5928.
Alshabanat A, Zafari Z, Albanyan O, Dairi M, FitzGerald JM. Asthma and COPD Overlap Syndrome (ACOS): A Systematic Review and Meta Analysis. PLoS ONE. 2015;10(9): e0136065. https://doi.org/10.1371/journal.pone.0136065.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6. https://doi.org/10.1136/bmj.39489.470347.AD.
Caton JG, Armitage G, Berglundh T, Chapple ILC, Jepsen S, Kornman KS, et al. A new classification scheme for periodontal and peri-implant diseases and conditions - Introduction and key changes from the 1999 classification. J Clin Periodontol. 2018;45(Suppl 20):S1-8. https://doi.org/10.1111/jcpe.12935.
Bartha V, Exner L, Schweikert D, Peter Woelber J, Vach K, Meyer AL, et al. Effect of the Mediterranean diet on gingivitis: A randomized controlled trial. J Clin Periodontol. https://doi.org/10.1111/jcpe.13576
Woelber JP, Bremer K, Vach K, Konig D, Hellwig E, Ratka-Kruger P, et al. An oral health optimized diet can reduce gingival and periodontal inflammation in humans - a randomized controlled pilot study. BMC Oral Health. 2016;17(1):28. https://doi.org/10.1186/s12903-016-0257-1.
Woelber JP, Gartner M, Breuninger L, Anderson A, Konig D, Hellwig E, et al. The influence of an anti-inflammatory diet on gingivitis. A randomized controlled trial. J Clin Periodontol 2019;46(4):481–90. https://doi.org/10.1111/jcpe.13094.
Rajaram SS, Nisha S, Ali NM, Shashikumar P, Karmakar S, Pandey V. Influence of a Low-Carbohydrate and Rich in Omega-3 Fatty Acids, Ascorbic Acid, Antioxidants, and Fiber Diet on Clinical Outcomes in Patients with Chronic Gingivitis: A Randomized Controlled Trial. J Int Soc Prev Community Dent. 2021;11(1):58–67. https://doi.org/10.4103/jispcd.JISPCD_365_20.
Atarbashi-Moghadam F, Moallemi-Pour S, Atarbashi-Moghadam S, Sijanivandi S, Baghban AA. Effects of raw vegan diet on periodontal and dental parameters. Tzu Chi Med J. 2020;32(4):357–61. https://doi.org/10.4103/tcmj.tcmj_161_19.
Laffranchi L, Zotti F, Bonetti D, Dalessandi D, Fontana P. Oral implications of the vegan diet: observational study. Minerva Stomatol 2010;59:11.12:583–91.
Linkosalo E, Markkanen H, Syrjanen S. Effects of a lacto-ovo-vegetarian diet on the free amino acid composition of wax-stimulated whole human saliva. J Nutr. 1985;115(5):588–92. https://doi.org/10.1093/jn/115.5.588.
Linkosalo E, Ohtonen S, Markkanen H, Karinpaa A, Kumpusalo E. Caries, periodontal status and some salivary factors in lactovegetarians. Scand J Dent Res. 1985;93(4):304–8. https://doi.org/10.1111/j.1600-0722.1985.tb01973.x.
Zotti F, Laffranchi L, Fontana P, Dalessandi D, Bonetti D. Effetti della fluoroterapia sulle alterazioni orali determinate dalla dieta vegana. Minerva Stomatol. 2014;63(5):179–88.
Staufenbiel I, Weinspach K, Forster G, Geurtsen W, Gunay H. Periodontal conditions in vegetarians: a clinical study. Eur J Clin Nutr. 2013;67(8):836–40. https://doi.org/10.1038/ejcn.2013.101.
Abbass MMS, Rady D, Radwan IA, el Moshy S, AbuBakr N, Ramadan M, et al. The occurrence of periodontal diseases and its correlation with different risk factors among a convenient sample of adult Egyptian population: a cross-sectional study. F1000Res 2019;8:1740. https://doi.org/10.12688/f1000research.20310.2.
Alhassani AA, Hu FB, Li Y, Rosner BA, Willett WC, Joshipura KJ. The associations between major dietary patterns and risk of periodontitis. J Clin Periodontol. 2021;48(1):2–13. https://doi.org/10.1111/jcpe.13380.
Alhassani AA, Hu FB, Rosner BA, Tabung FK, Willett WC, Joshipura KJ. The relationship between inflammatory dietary pattern and incidence of periodontitis. Br J Nutr. 2021;126(11):1698–708. https://doi.org/10.1017/S0007114520005231.
Alsyefi AA, Alasqah M. Dietary habits and periodontal health in Saudi Arabia: A qualitative study. Eur J Mol Clin Med. 2021;8(1):1258–70.
Altun E, Walther C, Borof K, Petersen E, Lieske B, Kasapoudis D, et al. Association between Dietary Pattern and Periodontitis-A Cross-Sectional Study. Nutrients. 2021;13:11. https://doi.org/10.3390/nu13114167.
Al-Zahrani MS, Borawski EA, Bissada NF. Periodontitis and three health-enhancing behaviors: maintaining normal weight, engaging in recommended level of exercise, and consuming a high-quality diet. J Periodontol. 2005;76(8):1362–6. https://doi.org/10.1902/jop.2005.76.8.1362.
Caine RL. Correlation of periodontal disease, dental caries, oral hygiene, dietary patterns, and academic majors among college students. Q Natl Dent Assoc. 1976;35(1):20–6.
Chalikias MS, Kyriakopoulos GL. Individualized daily values affecting the dentist condition of Greek students. J Food Agric Environ. 2011;9(1):159–65.
Costa PD, Canaan JCR, Midori Castelo P, Campideli Fonseca D, Marcia Pereira-Dourado S, Mendonca Murata R, et al. Influence of Micronutrient Intake, Sociodemographic, and Behavioral Factors on Periodontal Status of Adults Assisted by a Public Health Care System in Brazil: A Cross-Sectional Multivariate Analysis. Nutrients. 2021;13:3. https://doi.org/10.3390/nu13030973.
Eberhard J, Ruiz K, Tan J, Jayasinghe TN, Khan S, Eroglu E, et al. A randomised clinical trial to investigate the effect of dietary protein sources on periodontal health. J Clin Periodontol. https://doi.org/10.1111/jcpe.13587.
Grobler SR, Blignaut JB. The effect of a high consumption of apples or grapes on dental caries and periodontal disease in humans. Clin Prev Dent. 1989;11(1):8–12.
Holmes CB, Collier D. Periodontal disease, dental caries, oral hygiene and diet in adventist and other teenagers. J Periodontol. 1966;37(2):100–7. https://doi.org/10.1902/jop.1966.37.2.100.
Hosoda A, Komagamine Y, Kanazawa M, Hama Y, Kojo A, Minakuchi S. The Association between Dietary Habits and Periodontal Disease in Young Adult Women. J Nutr Sci Vitaminol (Tokyo). 2021;67(1):48–56. https://doi.org/10.3177/jnsv.67.48.
Hung HC, Colditz G, Joshipura KJ. The association between tooth loss and the self-reported intake of selected CVD-related nutrients and foods among US women. Community Dent Oral Epidemiol. 2005;33(3):167–73. https://doi.org/10.1111/j.1600-0528.2005.00200.x.
Iwasaki M, Ennibi OK, Bouziane A, Erraji S, Lakhdar L, Rhissassi M, et al. Association between periodontitis and the Mediterranean diet in young Moroccan individuals. J Periodontal Res. 2021;56(2):408–14. https://doi.org/10.1111/jre.12833.
Jaghasi I, Hatahet W, Dashash M. Dietary patterns and oral health in schoolchildren from Damascus, Syrian Arab Republic. East Mediterr Health J. 2012;18(4):358–64. https://doi.org/10.26719/2012.18.4.358.
Jauhiainen L, Suominen AL, Kanerva N, Mannisto S, Knuuttila M, Ylostalo P. Periodontal pocketing and gingival bleeding in relation to Nordic diet - results from a population-based survey. J Clin Periodontol. 2016;43(12):1013–23. https://doi.org/10.1111/jcpe.12631.
Kalyanpur R, Bilagi UR, Shetty PJ. Prosthodontic Need among Adults of Hubli, Karnataka India. J Evol Med Dent Sci. 2019;8(45):3378–81. https://doi.org/10.14260/jemds/2019/733.
Karjalainen S, Sewon L, Soderling E, Lapinleimu H, Seppanen R, Simell O. Oral health of 3-year-old children and their parents after 29 months of child-focused antiatherosclerotic dietary intervention in a prospective randomized trial. Caries Res. 1997;31(3):180–5. https://doi.org/10.1159/000262395.
Kaye EK, Heaton B, Sohn W, Rich SE, Spiro A 3rd, Garcia RI. The Dietary Approaches to Stop Hypertension Diet and New and Recurrent Root Caries Events in Men. J Am Geriatr Soc. 2015;63(9):1812–9. https://doi.org/10.1111/jgs.13614.
Khocht A, Orlich M, Paster B, Bellinger D, Lenoir L, Irani C, et al. Cross-sectional comparisons of subgingival microbiome and gingival fluid inflammatory cytokines in periodontally healthy vegetarians versus non-vegetarians. J Periodontal Res. 2021;56(6):1079–90. https://doi.org/10.1111/jre.12922.
Kondo K, Ishikado A, Morino K, Nishio Y, Ugi S, Kajiwara S, et al. A high-fiber, low-fat diet improves periodontal disease markers in high-risk subjects: a pilot study. Nutr Res. 2014;34(6):491–8. https://doi.org/10.1016/j.nutres.2014.06.001.
Kono GN, Hendiani I, Komara I. Dietary habit of chronic periodontitis patients based on Balanced Nutrition Guidelines from the Ministry of Health of the Republic of Indonesia. Padjajaran J Dent. 2021;33:1. https://doi.org/10.24198/pjd.vol33no1.15404.
Kotsakis GA, Chrepa V, Shivappa N, Wirth M, Hebert J, Koyanagi A, et al. Diet-borne systemic inflammation is associated with prevalent tooth loss. Clin Nutr. 2018;37(4):1306–12. https://doi.org/10.1016/j.clnu.2017.06.001.
Kumar HA, Shetty NJ. Correlation between type of diet and periodontal parameters. Indian J Public Health Res Dev. 2018;9:12. https://doi.org/10.5958/0976-5506.2018.01832.6.
Kwok T, Yu CN, Hui HW, Kwan M, Chan V. Association between functional dental state and dietary intake of Chinese vegetarian old age home residents. Gerodontology. 2004;21(3):161–6. https://doi.org/10.1111/j.1741-2358.2004.00030.x.
Li A, Chen Y, Schuller AA, van der Sluis LWM, Tjakkes GE. Dietary inflammatory potential is associated with poor periodontal health: A population-based study. J Clin Periodontol. 2021;48(7):907–18. https://doi.org/10.1111/jcpe.13472.
Linkosalo E, Halonen P, Markkanen H. Factors related to dental health and some salivary factors in Finnish Seventh-Day Adventists. Proc Finn Dent Soc. 1988;84(5–6):279–89.
Machado V, Botelho J, Viana J, Pereira P, Lopes LB, Proenca L, et al. Association between Dietary Inflammatory Index and Periodontitis: A Cross-Sectional and Mediation Analysis. Nutrients. 2021;13:4. https://doi.org/10.3390/nu13041194.
Mazur M, Bietolini S, Bellardini D, Lussi A, Corridore D, Maruotti A, et al. Oral health in a cohort of individuals on a plant-based diet: a pilot study. Clin Ter. 2020;171(2):e142–8. https://doi.org/10.7417/CT.2020.2204.
Nielsen SJ, Trak-Fellermeier MA, Joshipura K, Dye BA. Dietary Fiber Intake Is Inversely Associated with Periodontal Disease among US Adults. J Nutr. 2016;146(12):2530–6. https://doi.org/10.3945/jn.116.237065.
Rahmatulla M, Guile EE. Relationship between dental caries and vegetarian and non-vegetarian diets. Community Dent Oral Epidemiol. 1990;18(5):277–8. https://doi.org/10.1111/j.1600-0528.1990.tb00077.x.
Reyes-Izquierdo A, Flores Gonzales LA, Caballero-Garcia CS, Leon-Rios XA. Association between diet of the vegan population and self-perception of periodontal state in Metropolitan Lima. Nutr Hosp. https://doi.org/10.20960/nh.03757
Richardson RL, Jones M. A bacteriologic census of human saliva. J Dent Res. 1958;37(4):697–709. https://doi.org/10.1177/00220345580370041701.
Sedgley CM, Chu CS, Lo ECM, Samaranayake LP. The oral prevalence of aerobic and facultatively anaerobic gram-negative rods and yeasts in semi-recluse human vegetarians. Arch Oral Biol. 1996;41(3):307–9. https://doi.org/10.1016/0003-9969(95)00125-5.
Sherfudhin H, Abdullah A, Shaik H, Johansson A. Some aspects of dental health in young adult Indian vegetarians. A pilot study. Acta Odontol Scand. 1996;54(1):44–8. https://doi.org/10.3109/00016359609003508.
Stein C, Cunha-Cruz J, Hugo FN. Is dietary pattern a mediator of the relationship between socioeconomic status and dental caries? Clin Oral Investig. 2021;25(9):5441–7. https://doi.org/10.1007/s00784-021-03852-5.
Tennert C, Reinmuth AC, Bremer K, Al-Ahmad A, Karygianni L, Hellwig E, et al. An oral health optimized diet reduces the load of potential cariogenic and periodontal bacterial species in the supragingival oral plaque: A randomized controlled pilot study. Microbiologyopen. 2020;9(8): e1056. https://doi.org/10.1002/mbo3.1056.
Vaananen MK, Markkanen HA, Tuovinen VJ, Kullaa AM, Karinpaa AM, Luoma H, et al. Dental caries and mutans streptococci in relation to plasma ascorbic acid. Scand J Dent Res. 1994;102(2):103–8. https://doi.org/10.1111/j.1600-0722.1994.tb01163.x.
Woelber JP, Tennert C, Ernst SF, Vach K, Ratka-Kruger P, Bertz H, et al. Effects of a Non-Energy-Restricted Ketogenic Diet on Clinical Oral Parameters. An Exploratory Pilot Trial. Nutrients. 2021;13:12. https://doi.org/10.3390/nu13124229.
Wright DM, McKenna G, Nugent A, Winning L, Linden GJ, Woodside JV. Association between diet and periodontitis: a cross-sectional study of 10,000 NHANES participants. Am J Clin Nutr 2020;112(6):1485–91. https://doi.org/10.1093/ajcn/nqaa266.
Yoshihara A, Watanabe R, Hanada N, Miyazaki H. A longitudinal study of the relationship between diet intake and dental caries and periodontal disease in elderly Japanese subjects. Gerodontology. 2009;26(2):130–6. https://doi.org/10.1111/j.1741-2358.2008.00244.x.
Chapple ILC, Mealey BL, Van Dyke TE, Bartold PM, Dommisch H, Eickholz P, et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Clin Periodontol. 2018;45:S68-77. https://doi.org/10.1111/jcpe.12940.
Ito H, Numabe Y, Hashimoto S, Sekino S, Murakashi E, Ishiguro H, et al. Correlation Between Gingival Crevicular Fluid Hemoglobin Content and Periodontal Clinical Parameters. J Periodontol. 2016;87(11):1314–9. https://doi.org/10.1902/jop.2016.160092.
McClanahan SF, Bartizek RD, Biesbrock AR. Identification and consequences of distinct Loe-Silness gingival index examiner styles for the clinical assessment of gingivitis. J Periodontol. 2001;72(3):383–92. https://doi.org/10.1902/jop.2001.72.3.383.
Dodington DW, Fritz PC, Sullivan PJ, Ward WE. Higher Intakes of Fruits and Vegetables, beta-Carotene, Vitamin C, alpha-Tocopherol, EPA, and DHA Are Positively Associated with Periodontal Healing after Nonsurgical Periodontal Therapy in Nonsmokers but Not in Smokers. J Nutr. 2015;145(11):2512–9. https://doi.org/10.3945/jn.115.211524.
Petropoulou M, Efthimiou O, Rucker G, Schwarzer G, Furukawa TA, Pompoli A, et al. A review of methods for addressing components of interventions in meta-analysis. PLoS ONE. 2021;16(2): e0246631. https://doi.org/10.1371/journal.pone.0246631.
Albenberg LG, Wu GD. Diet and the intestinal microbiome: associations, functions, and implications for health and disease. Gastroenterology. 2014;146(6):1564–72. https://doi.org/10.1053/j.gastro.2014.01.058.
Baima G, Ribaldone DG, Muwalla M, Romano F, Citterio F, Armandi A, et al. Can Periodontitis Affect the Health and Disease of the Digestive System? A Comprehensive Review of Epidemiological Evidence and Biological Mechanisms. Curr Oral Health Rep. 2021;8(4):96–106. https://doi.org/10.1007/s40496-021-00302-9.
van Bussel BC, Henry RM, Ferreira I, van Greevenbroek MM, van der Kallen CJ, Twisk JW, et al. A healthy diet is associated with less endothelial dysfunction and less low-grade inflammation over a 7-year period in adults at risk of cardiovascular disease. J Nutr. 2015;145(3):532–40. https://doi.org/10.3945/jn.114.201236.
Ishikado A, Kondo K, Maegawa H, Morino K. Nutrition and Periodontal Health in the Patients with Diabetes Mellitus: a Review from the Viewpoint of Endothelial Function. Curr Oral Health Rep. 2021;8(4):67–74. https://doi.org/10.1007/s40496-021-00297-3.
Magrin GL, Strauss FJ, Benfatti CAM, Maia LC, Gruber R. Effects of Short-Chain Fatty Acids on Human Oral Epithelial Cells and the Potential Impact on Periodontal Disease: A Systematic Review of In Vitro Studies. Int J Mol Sci. 2020;21(14):4895. https://doi.org/10.3390/ijms21144895.
Stanisic D, Jeremic N, Majumder S, Pushpakumar S, George A, Singh M, et al. High Fat Diet Dysbiotic Mechanism of Decreased Gingival Blood Flow. Front Physiol. 2021;12: 625780. https://doi.org/10.3389/fphys.2021.625780.
Hussain T, Tan B, Yin Y, Blachier F, Tossou MC, Rahu N. Oxidative Stress and Inflammation: What Polyphenols Can Do for Us? Oxid Med Cell Longev. 2016;2016:7432797. https://doi.org/10.1155/2016/7432797.
Benatar JR, Stewart RAH. Cardiometabolic risk factors in vegans; A meta-analysis of observational studies. PLoS ONE. 2018;13(12): e0209086. https://doi.org/10.1371/journal.pone.0209086.
Frame LA, Costa E, Jackson SA. Current explorations of nutrition and the gut microbiome: a comprehensive evaluation of the review literature. Nut Rev. 2020;78(10):798–812. https://doi.org/10.1093/nutrit/nuz106.
Losno EA, Sieferle K, Perez-Cueto FJA, Ritz C. Vegan Diet and the Gut Microbiota Composition in Healthy Adults. Nutrients. 2021;13(7):2402. https://doi.org/10.3390/nu13072402.
Gibiino G, de Siena M, Sbrancia M, Binda C, Sambri V, Gasbarrini A, et al. Dietary Habits and Gut Microbiota in Healthy Adults: Focusing on the Right Diet. A Systematic Review. Int J Mol Sci. 2021;22(13):6728. https://doi.org/10.3390/ijms22136728.
Pulido-Moran M, Bullon P, Morillo JM, Battino M, Quiles JL, Ramirez-Tortosa M. The relationship between insulin resistance and periodontitis is not affected by Mediterranean diet in a Spanish population. Arch Oral Biol. 2017;77:62–7. https://doi.org/10.1016/j.archoralbio.2017.01.023.
Shakeel R, Ishaque A, Hassan M, Quereshi S, Din SU, Amin G, et al. Effect of mediterranean diet on periodontal diseases among diabetic patients. Pak J Sci. 2021;73(1):68–71.
Holmer H, Widen C, Wallin Bengtsson V, Coleman M, Wohlfart B, Steen S, et al. Improved General and Oral Health in Diabetic Patients by an Okinawan-Based Nordic Diet: A Pilot Study. Int J Mol Sci. 2018;19:7. https://doi.org/10.3390/ijms19071949.
Martinez-Herrera M, Lopez-Domenech S, Silvestre FJ, Silvestre-Rangil J, Banuls C, Hernandez-Mijares A, et al. Dietary therapy and non-surgical periodontal treatment in obese patients with chronic periodontitis. J Clin Periodontol. 2018;45(12):1448–57. https://doi.org/10.1111/jcpe.13030.
Jauhiainen LM, Suominen AL, Mannisto S, Knuuttila M, Ylostalo PV. Periodontal condition in relation to the adherence to nutrient recommendations in daily smokers. J Clin Periodontol. 2018;45(6):636–49. https://doi.org/10.1111/jcpe.12878.
Feres M, Retamal-Valdes B, Faveri M, Duarte P, Shibli J, Soares GMS, et al. Proposal of a Clinical Endpoint for Periodontal Trials: The Treat-to-Target Approach. J Int Acad Periodontol. 2020;22(2):41–53.
Eke PI, Page RC, Wei L, Thornton-Evans G, Genco RJ. Update of the case definitions for population-based surveillance of periodontitis. J Periodontol. 2012;83(12):1449–54. https://doi.org/10.1902/jop.2012.110664.
Page RC, Eke PI. Case Definitions for Use in Population-Based Surveillance of Periodontitis. J Periodontol. 2007;78(7s):1387–99. https://doi.org/10.1902/jop.2007.060264.
Foster E, Bradley J. Methodological considerations and future insights for 24-hour dietary recall assessment in children. Nutr Res. 2018;51:1–11. https://doi.org/10.1016/j.nutres.2017.11.001.
Katkade VB, Sanders KN, Zou KH. Real world data: an opportunity to supplement existing evidence for the use of long-established medicines in health care decision making. J Multidiscip Healthc. 2018;11:295–304. https://doi.org/10.2147/JMDH.S160029.
Anglemyer A, Horvath HT, Bero L. Healthcare outcomes assessed with observational study designs compared with those assessed in randomized trials. Cochrane Database Syst Rev 2014;4:MR000034. https://doi.org/10.1002/14651858.MR000034.pub2.
Funding
This study was supported by National Commission for Scientific and Technological Research, National Ph.D. Scholarship Program [2018—21180023], Santiago, Chile. The receiver of this funding is the corresponding author Dr. Mauricio Baeza. The funding only covers the human resources used for the development of this research; it does not include funds for the publication of this or any other article, so there is currently no open access policy linked to this grant. Therefore, we compliant with the subscription publication route.
Author information
Authors and Affiliations
Contributions
CRediT: Gustavo Sáenz-Ravello was involved in conceptualization, methodology, formal analysis, writing—original draft, Loreto Matamala helped in methodology, formal analysis, writing—original draft, Nidia Castro dos Santos, Patricia Cisternas, Jorge Gamonal, Natalia Bello, Alejandra Fernandez, Natalia Bello-Escamilla and Marcela Hernandez were involved in writing—review & editing, Mauricio Baeza contributed to conceptualization, methodology, formal analysis, writing—original draft, supervision, funding acquisition.
Corresponding author
Ethics declarations
Conflicts of interests/Competing interests
We have no conflicts of interests to declare.
Human and Animal Rights and Informed Consent
Not applicable. We use secondary data that do not require informed consent to be used, according to the International Ethical Guidelines for Health-related Research Involving Humans prepared by the Council for International Organizations of Medical Sciences (CIOMS) in collaboration with the World Health Organization (WHO) in Geneva, 2016.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
PROSPERO registration code: CRD42020203508
This article is part of the Topical Collection on Oral Disease and Nutrition
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Sáenz-Ravello, G., Matamala, L., dos Santos, N.C. et al. Healthy Dietary Patterns on Clinical Periodontal Parameters: A GRADE Compliant Systematic Review and Meta-analysis. Curr Oral Health Rep 9, 32–55 (2022). https://doi.org/10.1007/s40496-022-00307-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40496-022-00307-y