Abstract
Ingestion of oral dosage forms with food can drastically change drug pharmacokinetic parameters to consumption in fasted state. Accurate prediction of food effect (FE) is an important focus during drug development, as well as a requirement for drug approval by the Food and Drug Administration. FE can significantly restrict the clinical usefulness of drugs and is a principal parameter that must be considered early in drug development. Several approaches are available to predict FE in the human, including cell culture models, a variety of small and large animal models, and, more recently, physiologically based pharmacokinetic computerized models that incorporate biorelevant drug physicochemical properties. Each has its own advantages and disadvantages. While many methods are available to study FE, not all of these methods are applicable, efficient, consistent, financially feasible, or reasonable for every drug or drug formulation. Most importantly, different models may offer different applicability in accurately predicting FE in human species. Drug development is a long and often expensive process. Understanding of and access to an appropriate, reproducible, frugal means of FE assessment is vital in the field of drug development in order to ensure the development of a safe and effective drug. The following review delineates the advantages and disadvantages of a variety of preclinical FE study methods. While no single approach is good enough to give completely reliable predictions, a combination of in vitro, in vivo, and in silico approach may be advantageous to predict FE.
Similar content being viewed by others
References
Mathias N, Xu Y, Vig B, Kestur U, Saari A, Crison J, et al. Food effect in humans: predicting the risk through in vitro dissolution and in vivo pharmacokinetic models. AAPS J. 2015;17(4):988–98.
Koziolek M, Grimm M, Schneider F, Jedamzik P, Sager M, Kühn JP, et al. Navigating the human gastrointestinal tract for oral drug delivery: uncharted waters and new frontiers. Adv Drug Deliv Rev. 2016;101:75–88.
Deng J, Zhu X, Chen Z, Fan CH, Kwan HS, Wong CH, et al. A review of food–drug interactions on oral drug absorption. Drugs. 2017;77(17):1833–55.
Mignot A, Guillaume M, Göhler K, Stahlberg HJ. Oral bioavailability of gatifloxacin in healthy volunteers under fasting and fed conditions. Chemotherapy. 2002;48(3):111–5.
Gammaitoni A, Smith S, Boyd B. The lack of effect of food on the pharmacokinetics of ZX008 (fenfluramine oral solution): results of a single-dose , Two-period Crossover Study. Clin Ther. 2018;40(8):1338–46.
U.S. Department of Health and Human Services Food and Drug Administration. Guidance for Industry - Bioavailability and Bioequivalence. 2014 http://academy.gmp-compliance.org/guidemgr/files/UCM389370.pdf. Accessed November 2019.
Gupta N, Hanley MJ, Venkatakrishnan K, Wang B, Sharma S, Bessudo A, et al. The effect of a high-fat meal on the pharmacokinetics of ixazomib, an oral proteasome inhibitor, in patients with advanced solid tumors or lymphoma. J Clin Pharmacol. 2016;56(10):1288–95.
U.S. Department of Health and Human Services Food and Drug Administration. Ninlaro (ixazomib) [package insert]. 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/208462lbl.pdf. Accessed 07 June 2020.
Mudie DM, Amidon GL, Amidon GE. Physiological parameters for oral delivery and in vitro testing. Mol Pharm. 2010;7(5):1388–405.
Pavurala N, Achenie LEK. A mechanistic approach for modeling oral drug delivery. Comput Chem Eng. 2013;57:196–206.
Farha M, Masson E, Tomkinson H, Mugundu G. Food effect study design with oral drugs: lessons learned from recently approved drugs in oncology. J Clin Pharmacol. 2018;59(4):463–71.
Verwei M, Minekus M, Zeijdner E, Schilderink R, Havenaar R. Evaluation of two dynamic in vitro models simulating fasted and fed state conditions in the upper gastrointestinal tract (TIM-1 and tiny-TIM) for investigating the bioaccessibility of pharmaceutical compounds from oral dosage forms. Int J Pharm. 2016;498(1–2):178–86.
Souliman S, Blanquet S, Beyssac E, Cardot J-M. A level A in vitro/in vivo correlation in fasted and fed states using different methods: applied to solid immediate release oral dosage form. Eur J Pharm Sci. 2006;27(1):72–9.
Raman S, Polli JE. Prediction of positive food effect: bioavailability enhancement of BCS class II drugs. Int J Pharm. 2016;506(1–2):110–5.
Miyake M, Oka Y, Mukai T. Food effect on meal administration time of pharmacokinetic profile of cilostazol, a BCS class II drug. Xenobiotica. 2019;50(2):145–9.
Radwan A, Zaid AN, Jaradat N, Odeh Y. Food effect: the combined effect of media pH and viscosity on the gastrointestinal absorption of ciprofloxacin tablet. Eur J Pharm Sci. 2017;101:100–6.
Buch P, Langguth P, Kataoka M, Yamashita S. IVIVC in oral absorption for fenofibrate immediate release tablets using a dissolution/permeation system. J Pharm Sci. 2009;98(6):2001–9.
Abuhelwa AY, Foster DJR, Mudge S, Hayes D, Upton RN. Population pharmacokinetic modeling of itraconazole and hydroxyitraconazole for oral SUBA-itraconazole and Sporanox capsule formulations in healthy subjects in fed and fasted states. Antimicrob Agents Chemother. 2015;59(9):5681–96.
Heinen CA, Reuss S, Amidon GL, Langguth P. Ion pairing with bile salts modulates intestinal permeability and contributes to food-drug interaction of BCS class III compound trospium chloride. Mol Pharm. 2013;10(11):3989–96.
Sutton SC, Nause R, Gandelman R. The impact of gastric pH, volume, and emptying on the food effect of ziprasidone oral absorption. AAPS J. 2017;19(4):1084–90.
Andreas CJ, Pepin X, Makopoulos C, et al. Mechanistic investigation of the negative food effect of modified release zolpidem. Eur J Pharm Sci. 2017;102:284–98.
Shono Y, Jantratid E, Janssen N, Kesisoglou F, Mao Y, Vertzoni M, et al. Prediction of food effects on the absorption of celecoxib based on biorelevant dissolution testing coupled with physiologically based pharmacokinetic modeling. Eur J Pharm Biopharm. 2009;73(1):107–14.
Won CS, Oberlies NH, Paine MF. Mechanisms underlying food-drug interactions: inhibition of intestinal metabolism and transport. Pharmacol Ther. 2012;136(2):186–21.
Koziolek M, Kostewicz E, Vertzoni M. Physiological considerations and in vitro strategies for evaluating the influence of food on drug release from extended-release formulations. AAPS PharmSciTech. 2018;19(7):2885–97.
Batchelor H. Influence of food on paediatric gastrointestinal drug absorption following oral administration: a review. Children. 2015;2(2):244–71.
Dressman JB, Berardi RR, Dermentzoglou LC, Russell TL, Schmaltz SP, Barnett JL, et al. Upper grastrointestinal (GI) pH in young, healthy men and women. Pharm Res. 1990;7(7):756–61.
Abuhelwa AY, Williams DB, Upton RN, Foster DRR. Food, gastrointestinal pH, and models of oral drug absorption. Eur J Pharm Biopharm. 2017;112:234–48.
Holmstock N, De Bruyn T, Bevernage J, et al. Exploring food effects on indinavir absorption with human intestinal fluids in the mouse intestine. Eur J Pharm Sci. 2013;49(1):27–32.
Rubbens J, Brouwers J, Tack J, Augustijins P. Gastrointestinal dissolution, supersaturation and precipitation of the weak base indinavir in healthy volunteers. Eur J Pharm Biopharm. 2016;109:122–9.
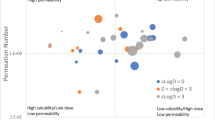
Benet LZ. The role of BCS (Biopharmaceutics Classification System) and BDDCS (Biopharmaceutics Drug Disposition Classification System) in drug development. J Pharm Sci. 2013;102(1):34–42.
Benet LZ. The use of BDDCS in drug development : the observations, the predictions, understanding the scientific basis and the extensions. 2016. http://www.scdmdg.org/slides/2016-04-19-SCDMDG-BDDCS.pdf. Accessed January 2019.
Amidon GL, Lennernäs H, Shah VP, Crison JR. A theoretic basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm Res. 1995;12(3):413–20.
Camilleri M. Integrated upper gastrointestinal response to food intake. Gastroenterology. 2006;131(2):640–58.
Marathe PH, Wen Y, Norton J, Greene DS, Barbhaiya RH, Wilding IR. Effect of altered gastric emptying and gastrointestinal motility on metformin absorption. Br J Clin Pharmacol. 2000;50(4):325–32.
Ledergerber B, Bettex JD, Joos B, Flepp M, Lüthy R. Effect of standard breakfast on drug absorption and multiple-dose pharmacokinetics of ciprofloxacin. Antimicrob Agents Chemother. 1985;27(3):350–2.
Galanello R, Piga A, Cappellini M, et al. Effect of food, type of food, and time of food intake on deferasirox bioavailability: recommendations for an optimal deferasirox administration regimen. J Clin Pharmacol. 2008;48(4):428–35.
U.S. Department of Health and Human Services Food and Drug Administration. Guidance for industry, bioequivalence studies with pharmacokinetic endpoints for drugs submitted under an ANDA. 2013. http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/uc, 2013. Accessed February 2019.
Tran JQ, Hartung JP, Tompkins CA, Frohna PA. Effects of high- and low-fat meals on the pharmacokinetics of ozanimod, a novel sphingosine-1-phosphate receptor modulator. Clin Pharmacol Drug Dev. 2018;7(6):634–40.
Nichols AI, Richards LS, Behrle J, et al. Effect of food on the pharmacokinetics of desvenlafaxine in healthy subjects. J Bioequiv Availab. 2012;4(2):24–9.
Löbenberg R, Krämer J, Shah VP, Amidon GL, Dressman JB. Dissolution testing as a prognostic tool for oral drug absorption: dissolution behavior of glibenclamide. Pharm Res. 2000;17(4):439–44.
Grimm M, Koziolek M, Kühn J-P, Weitschies W. Interindividual and intraindividual variability of fasted state gastric fluid volume and gastric emptying of water. Eur J Pharm Biopharm. 2018;127:309–17.
Bushra R, Aslam N, Khan AY. Food-drug interactions. Oman Med J. 2011;26(2):77–83.
Hwan Cho J, Mann Ko C. Food and drug interactions. J Lifestyle Med. 2017;7(1):1–9.
Sugano K, Kataoka M, da Costa MC, Yamashita S. Prediction of food effect by bile micelles on oral drug absorption considering free fraction in intestinal fluid. Eur J Pharm Sci. 2010;40(2):118–24.
Kaur N, Narang A, Bansal AK. Use of biorelevant dissolution and PBPK modeling to predict oral drug absorption. Eur J Pharm Biopharm. 2018;129:222–46.
Culen M, Rezacova A, Jampilek J, Dohnal J. Designing a dynamic dissolution method: a review of instrumental options and corresponding physiology of stomach and small intestine. J Pharm Sci. 2013;102(9):2995–3017.
Sievens-Figueroa L, Pandya N, Bhakay A, Keyvan G, Michniak-Kohn B, Bilgili E, et al. Using USP I and USP IV for discriminating dissolution rates of nano- and microparticle-loaded pharmaceutical strip-films. AAPS PharmSciTech. 2012;13(4):1473–82.
Berben P, Ashworth L, Beato S, Bevernage J, Bruel JL, Butler J, et al. Biorelevant dissolution testing of a weak base: interlaboratory reproducibility and investigation of parameters controlling in vitro precipitation. Eur J Pharm Biopharm. 2019;140:141–8.
Baxevanis F, Kuiper J, Fotaki N. Fed-state gastric media and drug analysis techniques: current status and points to consider. Eur J Pharm Biopharm. 2016;107:234–48.
United States Department of Health and Human Services Food and Drug Administration. Dissolution testing and acceptance criteria for immediate-release solid oral dosage form drug products containing high solubility drug substances guidance for industry. 2018. https://www.fda.gov/media/92988/download. Accessed February 2019.
Grady H, Elder D, Webster GK, Mao Y, Lin Y, Flanagan T, et al. Industry’s view on using quality control, biorelevant, and clinically relevant dissolution tests for pharmaceutical development, registration, and commercialization. J Pharm Sci. 2018;107(1):34–41.
Juenemann D, Jantratid E, Wagner C, Reppas C, Vertzoni M, Dressman JB. Biorelevant in vitro dissolution testing of products containing micronized or nanosized fenofibrate with a view to predicting plasma profiles. Eur J Pharm Biopharm. 2011;77(2):257–64.
Fuchs A, Leigh M, Kloefer B, Dressman JB. Advances in the design of fasted state simulating intestinal fluids: FaSSIF-V3. Eur J Pharm Biopharm. 2015;94:229–40.
Klein S. The use of biorelevant dissolution media to forecast the in vivo performance of a drug. AAPS J. 2010;12(3):397–406.
Keemink J, Bergström CAS. Caco-2 cell conditions enabling studies of drug absorption from digestible lipid-based formulations. Pharm Res. 2018;35(4):74.
Sambuy Y, De Angelis I, Ranaldi G, et al. The Caco-2 cell line as a model of the intestinal barrier: influence of cell and culture-related factors on Caco-2 cell functional characteristics. Cell Biol Toxicol. 2005;21(1):1–26.
Scheers NM, Almgren AB, Sandberg AS. Proposing a Caco-2/HepG2 cell model for in vitro iron absorption studies. J Nutr Biochem. 2014;25(7):710–5.
Hens B, Brouwers J, Anneveld B, et al. Gastrointestinal transfer: in vivo evaluation and implementation in in vitro and in silico predictive tools. Eur J Pharm Sci. 2014;15(63):233–42.
Ingels F, Deferme S, Destexhe E, Oth M, van den Mooter G, Augustijns P. Simulated intestinal fluid as transport medium in the Caco-2 cell culture model. Int J Pharm. 2002;232(1–2):183–92.
Wuyts B, Riethorst D, Brouwers J, Tack J, Annaert P, Augustijns P. Evaluation of fasted and fed state simulated and human intestinal fluids as solvent system in the Ussing chambers model to explore food effects on intestinal permeability. Int J Pharm. 2015;478(2):736–44.
Lee C-M, Luner PE, Locke K, Briggs K. Application of an artificial stomach-duodenum reduced gastric pH dog model for formulation principle assessment and mechanistic performance understanding. J Pharm Sci. 2017;106(8):1987–97.
Carino ST, Sperry DC, Hawley M. Relative bioavailability of three different solid forms of PNU-141659 as determined with the artificial stomach-duodenum model. J Pharm Sci. 2010;99(9):3923–30.
Honigford CR, Aburub A, Fadda HM. A simulated stomach duodenum model predicting the effect of fluid volume and prandial gastric flow patterns on nifedipine pharmacokinetics from cosolvent-based capsules. J Pharm Sci. 2019;108(1):288–94.
McConnell EL, Basit AW, Murdan S. Measurements of rat and mouse gastrointestinal pH, fluid and lymphoid tissue, and implications for in-vivo experiments. J Pharm Pharmacol. 2008;60(1):63–70.
De Leo L, Di Toro N, Decorti G, et al. Fasting increases tobramycin oral absorption in mice. Antimicrob Agents Chemother. 2010;54(4):1644–6.
Musther H, Olivares-Morales A, Hatley OJD, Liu B, Hodjegan AR. Animal versus human oral drug bioavailability: do they correlate. Eur J Pharm Sci. 2014;54(4):280–91.
Fujii F, Kanamaru T, Kikuchi H, Yamashita S, Sakuma S. Enteric-coated tablets improve oral bioavailability of DX-9065, a novel anticoagulant. Eur J Pharm Sci. 2011;42(4):392–9.
Chen EP, Mahar Doan KM, Portelli S, Coatney R, Vaden V, Shi W. Gastric pH and gastric residence time in fasted and fed conscious cynomolgus monkeys using the bravo pH system. Pharm Res. 2008;25(1):123–4.
Mahar KM, Portelli S, Coatney R, Chen EP. Gastric pH and gastric residence time in fasted and fed conscious beagle dogs using the Bravo pH system. J Pharm Sci. 2012;101(7):2439–48.
Parrott N, Lukacova V, Fraczkiewicz G, Bolger MB. Predicting pharmacokinetics of drugs using physiologically based modeling—application to food effects. AAPS J. 2009;11(1):45–53.
Zane P, Guo Z, MacGerorge D, Vicat P, Ollier C. Use of the pentagastrin dog model to explore the food effects on formulations in early drug development. Eur J Pharm Sci. 2014;16(57):207–13.
Lentz KA, Quitko M, Morgan DG, Grace JE Jr, Gleason C, Marathe PH. Development and validation of a preclinical food effect model. J Pharm Sci. 2007;96(2):459–72.
Cvijic S, Ibric S, Parojcic J, Djuris J. An in vitro - in silico approach for the formulation and characterization of ranitidine gastroretentive delivery systems. J Drug Deliv Sci Technol. 2017;45:1–10.
Conner TM, Nikolian VC, Georgoff PE, Pai MP, Alam HB, Sun D, et al. Physiologically based pharmacokinetic modeling of disposition and drug-drug interactions for valproic acid and divalproex. Eur J Pharm Sci. 2018;111:465–181.
Zhang T. Physiologically based pharmacokinetic modeling of disposition and drug-drug interactions for atorvastatin and its metabolites. Eur J Pharm Sci. 2015;77:216–29.
Grimstein M, Yan Y, Zhang X, et al. Physiologically based pharmacokinetic modeling in regulatory science : an update from the U. S. Food and Drug Administration’s Office of Clinical Pharmacology. J Pharm Sci. 2019;108(1):21–5.
Tistaert C, Heimbach T, Xia B, Parrott N, Samant TS, Kesisoglou F. Food effect projections via physiologically based pharmacokinetic modeling: predictive case studies. J Pharm Sci. 2019;108(1):592–602.
Willmann S, Thelen K, Becker C, Dressman JB, Lippert J. Mechanism-based prediction of particle size-dependent dissolution and absorption: cilostazol pharmacokinetics in dogs. Eur J Pharm Biopharm. 2010;76(1):83–94.
Riedmaier AE, Lindley DJ, Hall JA, et al. Mechanistic physiologically based pharmacokinetic modeling of the dissolution and food effect of a Biopharmaceutics Classification System IV compound—the venetoclax story. J Pharm Sci. 2018;107(1):495–502.
Yu LX, Amidon GL. A compartmental absorption and transit model for estimating oral drug absorption. Int J Pharm. 1999;186(2):119–25.
Jones HM, Parrott N, Ohlenbusch G, Lavé T. Predicting pharmacokinetic food effects using biorelevant solubility media and physiologically based modelling. Clin Pharmacokinet. 2006;45(12):1213–26.
Zhang H, Xia B, Sheng J, Heimbach T, Lin TH, He H, et al. Application of physiologically based absorption modeling to formulation development of a low solubility, low permeability weak base: mechanistic investigation of food effect. AAPS PharmSciTech. 2014;15(2):400–6.
Gao Z-W, Zhu Y-t, Yu M-m, et al. Preclinical pharmacokinetics of TPN729MA, a novel PDE5 inhibitor, and prediction of its human pharmacokinetics using a PBPK model. Acta Pharmacol Sin. 2015;36(12):1528–36.
Li X, Shi L, Tang X, Wang Q, Zhou L, Song W, et al. Mechanistic prediction of food effects for Compound A tablet using PBPK model. Saudi J Biol Sci. 2017;24(3):603–9.
Rebeka J, Jernegja O, Igor L, et al. PBPK absorption modeling of food effect and bioequivalence in fed state for two formulations with crystalline and amorphous forms of BCS 2 class drug in generic drug development. AAPS PharmSciTech. 2019;20(2):1–10.
Willmann S, Thelen K, Lippert J. Integration of dissolution into physiologically-based pharmacokinetic models III: PK-Sim. J Pharm Pharmcol. 2012;64(7):997–1007.
Eissing T, Kuepfer L, Becker C, et al. A computational systems biology software platform for multiscale modeling and simulation: integrating whole-body physiology, disease biology, and molecular reaction networks. Front Physiol. 2011;2(4):1–10.
Li M, Zhao P, Pan Y, Wagner C. Predictive performance of physiologically based pharmacokinetic models for the effect of food on oral drug absorption: current status. CPT Pharmacometrics Syst Pharmacol. 2018;7(2):82–9.
Dressman JB, Amidon GL, Reppas C, Shah VP. Dissolution testing as a prognostic tool for oral drug absorption: immediate release dosage forms. Pharm Res. 1998;15(1):11–22.
Pandey P, Hamey R, Bindra DS, Huang Z, Mathias N, Eley T, et al. From bench to humans: formulation development of a poorly water soluble drug to mitigate food effect. AAPS PharmSciTech. 2014;15(2):407–16.
Kim TH, Bulitta JB, Kim D-H, Shin S, Soo SB. Novel extended in vitro-in vivo correlation model for the development of extended-release formulations for baclofen: from formulation composition to in vivo pharmacokinetics. Int J Pharm. 2019;556:276–86.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Code Availability
n/a
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Food Factors: Molecular targets, mechanisms, pharmacology and in vivo efficacy
Rights and permissions
About this article
Cite this article
Zhang, T., Wells, E. A Review of Current Methods for Food Effect Prediction During Drug Development. Curr Pharmacol Rep 6, 267–279 (2020). https://doi.org/10.1007/s40495-020-00230-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40495-020-00230-9