Abstract
The number of individuals with autism spectrum disorders (ASD) diagnoses is increasing rapidly, indicating a need for multi-faceted interventions. The addition of a parent training component to cognitive–behavioral therapy (CBT) has been effectively used to treat a variety of psychological disorders in children to support generalization of skills and to reduce the burden of intensive therapy by using parents as co-therapists. We review these treatments as applied to childhood anxiety, oppositional/conduct, and attention-deficit/hyperactivity problems, as well as ASD-specific treatments that combine CBT with a parent component. The Stress and Anger Management Program, a 9-week emotion regulation treatment for school-aged children with high-functioning ASD, is described here as one example of a group CBT intervention that includes parent training.
Similar content being viewed by others
Introduction
Individuals with autism spectrum Disorders (ASD) demonstrate social communication difficulties and perseverative/repetitive interests or behaviors (American Psychiatric Association 2013). Recent estimates from the Centers for Disease Control and Prevention suggest that 1 in every 68 children meets criteria for an ASD (Centers for Disease Control and Prevention 2014). This high prevalence indicates that the need for timely, developmentally appropriate, and practical interventions is more critical now than ever before. Behavioral and cognitive–behavioral treatments have been found to be the most effective interventions for secondary and comorbid conditions in individuals with ASD (Dawson and Burner 2011; Scarpa et al. 2013a). Other co-occurring conditions, such as anxiety, attention difficulties, disruptive behaviors, depression, and general issues with emotion dysregulation, are often seen in children and adolescents with ASD (Levy et al. 2010; Mayes et al. 2011; Tonge et al. 1999; White et al. 2009).
The current review focuses only on children formerly thought of as having high-functioning ASD (HFA), meaning that they do not have intellectual impairment. Despite an average or above average level of cognitive functioning, these children still show difficulties in other areas, such as social communication (Landa 2000; Paul et al. 2009), peer relationships (e.g., Frankel and Myatt 2003; Frankel et al. 2010; Laugeson et al. 2012), some academic skills (Minshew et al. 1994; Estes et al. 2011), activities of daily living (Klin et al. 2007; Kanne et al. 2011), and social skills that may impact later school-to-work transitions (Higgins et al. 2008; Hurlbutt and Chalmers 2004). These children also show more emotional difficulties than their peers, continuing into adolescence. For example, researchers found that adolescents with HFA had more negative thoughts, behavioral problems, and life interference as compared with typically developing (TD) peers and peers with anxiety disorders, and the ASD participants had as much anxiety as their peers with anxiety disorders (Farrugia and Hudson 2006). Therefore, the addition of cognitive techniques to the traditional behavioral strategies used to treat symptoms of ASD is necessary, appropriate, and novel. Though others exist, we discuss the Stress and Anger Management Program (STAMP; Scarpa et al. 2013b) herein as one program example of cognitive–behavioral therapy (CBT) with a parent training (PT) component.
Over the last several decades, inclusion of parents has been noted as an integral part of behavioral treatment for children with ASD (Frankel and Myatt 2003; Lovaas 1987; Research Units on Pediatric Psychopharmacology (RUPP) Autism Network 2007), but less work has been done to include parents as facilitators of change in cognitive behavioral interventions. Evidence-based CBT is considered to be the gold standard for treatment of a variety of psychological disorders and is most successful for children when it has been modified to be developmentally appropriate (Kendall and Chodhury 2003; Weisz and Kazdin 2010). Within CBT, behavioral strategies seek to modify self-destructive actions, and cognitive techniques target how an individual thinks about a situation or processes information. In combination, CBT allows clinicians to change antecedent conditions and/or pair motivating reinforcers to help encourage positive behavior and promote new skills, while also focusing on changing maladaptive cognitions or thought processes. Additionally, when used to treat anxiety, CBT often systematically exposes the child to the feared stimulus in order to confront and overcome the fear.
Emerging evidence suggests that, when modified to a child’s developmental level, CBT can be an appropriate and effective intervention for a variety of psychopathologies (Weisz and Kazdin 2010; Sofronoff et al. 2005; Scarpa and Lorenzi 2013; Kendall et al. 2008). When modifying CBT for children, it is often recommended to introduce parents as a valuable piece of the therapeutic process. We propose that this is equally, if not more, true for children with ASD, for whom initiative for change and awareness of difficulties may be intrinsically low, and generalizability of skills to settings outside the clinic can be especially problematic.
Due to the oft-noted importance of parent inclusion in ASD interventions and the need for further refinement of PT, specifically in cognitive–behavioral programs for ASD, we aim to review behavioral and cognitive–behavioral PT interventions for children with and without ASD, noting components that appear to be most helpful. While this is not a comprehensive review, we present an overview of these treatments with the goal of summarizing the most effective content and delivery factors. We will end with a brief description of the development of PT within STAMP, a caregiver-assisted CBT intervention for the treatment of emotion dysregulation in young children with ASD, as a program example that may help guide future work in this area. While there are other successful CBTs for children with ASD that include family involvement (e.g., Reaven and Blakeley-Smith 2013; Sofronoff et al. 2007), STAMP is notable for filling the need for an emotion regulation treatment with PT for children young children (ages 5–7 years) for whom parent involvement is critical.
Importance of PT
Including PT in child-focused treatments is a common modification for a wide range of childhood disorders. However, there is variability with regard to the structure of PT and level and nature of parental involvement. Some of the common diagnostic areas in which parents are often involved in treatment include children with disruptive/oppositional behaviors, tics, attention-deficit/hyperactivity disorder (ADHD), anxiety disorders, eating disorders, and ASD (which will be discussed in a later section). Despite the variability associated with PT components of treatment, many programs have asserted the importance of this modification.
Parent management training (PMT) and behavioral parent training (BPT) are two commonly used terms that both generally refer to instructing parents to modify their child’s behavior in the home. For the purposes of this paper, any type of treatment that includes parent instruction will be considered a PT program. Although the child is the target of treatment, many programs that include PT do not directly involve the child in every session. When the child is not present, information and skills that are learned by parents in sessions are then applied in the home.
PT with Oppositional/Conduct Problems
In a meta-analysis of 26 studies that included 36 comparisons between experimental (i.e., BPT) and control (e.g., wait-list control or therapy other than BPT) groups for preschool/elementary school-age children with antisocial behavior (e.g., aggression, tantrums, noncompliance), positive effect sizes (ES) were found for all five outcome variables analyzed: overall child outcome (mean ES = 0.86), parental report of child outcome (mean ES = 0.84), observer report of child outcome (mean ES = 0.85), teacher report of child outcome (mean ES = 0.73), and parental adjustment (mean ES = 0.44) (Serketich and Dumas 1996). Overall, the average child whose parent participated in a BPT program was better adjusted after treatment than the average child whose parent received another treatment or no treatment. This evidence supports the involvement of parents when children are the focus of treatment.
A separate meta-analysis compared the effectiveness of BPT and CBT for youth with antisocial behavior between the ages of 3 and 12 years (McCart et al. 2006). This meta-analysis of 71 published outcome studies considered BPT to be training that instructed parents/caregivers in the use of behavior management concepts (e.g., differential reinforcement) and CBT to be therapy targeting maladaptive social–cognitive processes in youth to address topics such as social skills training, problem solving, or anger management. Results indicated that BPT was more effective for young children (preschool to school-age), while CBT was more effective for older children. This suggests that developmental issues are important to consider when determining the appropriateness of a particular intervention for any given child, with parent involvement potentially more beneficial in early childhood. However, this meta-analysis did not include programs that combined BPT and CBT approaches and cautioned that a number of studies have indicated that broad-based interventions (e.g., involvement of schools, parents, and youth) are more powerful than either BPT or CBT alone (e.g., Henggeler and Borduin 1990; Webster-Stratton and Hammond 1997).
Scahill et al. (2006) investigated an intervention for 24 children between the ages of 6 and 12 years who had both tics and disruptive behaviors. Participants were randomly assigned to either 10-week PMT combined with treatment as usual (e.g., clinical services including parent education, monitoring of symptoms, medication management, and/or child psychotherapy) or treatment as usual only. Participants that received the combination of PMT and treatment as usual were more likely than those who received only treatment as usual to be rated as “much improved” or “very much improved” by clinicians that were blind to group assignment (64 % of children in combination group, 17 % of children in control group). Additionally, the group that also received PMT evidenced a 51 % decline in parent-reported disruptive/oppositional behavior, while the control group only evidenced a 19 % decline (effect size = 0.96). Thus, the addition of parent management to treatment as usual in this group of children with tics and disruptive behavior disorders led to significant improvements in behavior.
A similar study compared the PMT-Oregon Model (PMTO; Patterson 2005) to regular services (described as being an active and appropriate alternative to PMTO that was offered by therapists in the comparison group; actual services received included family therapy, behavior therapy, cognitive therapy, humanistic-existential therapy, and other/eclectic therapy) in a total sample of 112 children between the ages of 4 and 12 years with conduct problems (Ogden and Hagen 2008). The purpose of PMTO is to use ecological and transactional principles to break patterns of interaction between children and parents that escalate disruptive behavior, and for parents to learn more effective discipline and problem solving. Results indicated that children of parents that received PMTO demonstrated better teacher-reported social competence and fewer parent-reported externalizing symptoms than those children who received regular services. Additionally, parents who received PMTO were found to use better disciplinary skills post-treatment than those whose children had received regular services. These results support using parents as the agent to improve outcomes for their children with conduct problems, with some evidence of generalization from the home to the school. Similar to the study by McCart and colleagues (2006), children in the younger age group (4–7 years) seemed to benefit more from PMTO than did children in the older age group (8–12 years).
Another well-known program designed for parents of children (ages 2–8 years) with noncompliance problems is a curriculum known as Parenting the Strong-Willed Child (PSWC; Long and Forehand 2002). This program trains parents to increase positive attention for good behavior, provide appropriate consequences, provide clear instructions, and other basic concepts related to behavior modification. In an independent evaluation of 71 parents who participated in the PSWC program, results indicated significant improvements in child behavior problems (both frequency and intensity, as reported by parents) and self-reported parenting behavior (Conners et al. 2007). As such, this study also provides evidence for effectively treating children through a parent intervention.
The Incredible Years Program (IYP; Webster-Stratton 2000) has evidenced success in both preventing and treating behavior problems in children ages 2–12 years. In this program, parents learn to teach children important skills through play, reduce critical and violent discipline, improve parental self-control and problem solving, increase social support, and improve involvement in school-related activities. Many randomized controlled trials have demonstrated evidence of improvements in child behavior across various contexts following the implementation of this treatment program (e.g., Webster-Stratton 1990; Miller and Rojas-Flores 1999; Taylor et al. 1998).
Additionally, Foster et al. (2007) used cost-effectiveness acceptability curves to analyze the various components of IYP, finding that the most cost-effective treatment involved a combination of components. For problems at school, the combination of parent and teacher training was found to be the most cost-effective; for problems at home, the combination of child, parent, and teacher training was found to be the most cost-effective. Finally, in one study of the IYP in twenty-five 2- to 5-year-old children with developmental delay, preliminary evidence supported the efficacy of this program in reducing negative child and parent behavior (McIntyre 2008).
PT with ADHD
ADHD is another childhood disorder for which parents are commonly involved in treatment, often in the form of PT. Fabiano et al. (2012)) used a wait-list controlled trial to investigate the efficacy of an 8-week BPT program designed for fathers of children with ADHD. In this study, participants included 55 fathers of children with ADHD between the ages of 6 and 12 years. The intervention consisted of BPT during the first half of each session on topics related to attending to positive behavior, issuing effective commands, problem solving, and using time out, while the second half of each session allowed the fathers to interact with their children and practice the skills they had just learned, while receiving feedback from clinicians. Compared with the wait-list control group, the fathers in the treatment group demonstrated lower rates of negative talk and higher rates of praise during parent–child interactions. Additionally, fathers reported a reduction in the intensity of their child’s problem behaviors. However, maintenance of these gains was somewhat limited at 1-month follow-up. Future research might investigate strategies for maximizing treatment gains over time in PT programs.
BPT in combination with routine clinical care was directly compared with routine clinical care alone in a randomized controlled study of 94 children with ADHD between the ages of 4 and 12 years (van den Hoofdakker et al. 2007). The combination of BPT and routine clinical care was superior to routine clinical care alone in improving both internalizing and behavioral problems. Interestingly, children assigned to the routine care alone condition were prescribed more medication. Thus, BPT over and above routine clinical care resulted in an enhancement of the effectiveness of routine clinical care by improving behavioral and internalizing problems, and potentially by also limiting the need for medication in children with ADHD.
Another study on children with ADHD targeted social competency and friendship quality in this population rather than behavioral problems (Mikami et al. 2010). Mikami and colleagues included 62 parents of children with ADHD (ages 6–10 years) and assigned half to a parental friendship coaching intervention and half to a no-treatment control group. Parents of 62 children without ADHD served as TD comparisons. The parental friendship coaching component (treatment group) used the parent as the agent of change and topics of training included teaching children good play skills, inviting a peer to have a playdate, and meeting new friends. Following treatment, children of parents who received friendship coaching evidenced more positive parent reports of social skills, reductions in parent-reported conflict and disengagement shown on playdates, and improved teacher-reported social acceptance, with continued improvement at 1-month follow up. Additionally, the parental friendship coaching program led to increases in parent facilitation and involvement of the child’s playgroup and reduced parental criticism of the child. This evidence suggests that parent training in parent friendship coaching can have a significant impact on child peer problems.
PT with Anxiety Disorders
Interventions in children with anxiety disorders have shown similar findings to many of those previously mentioned in studies of other childhood disorders. Whereas the prior studies reviewed above utilized primarily behavioral approaches, however, these studies emphasize cognitive–behavioral approaches in the treatment of anxiety and work with both the child and the parent in therapy (either individually or in combination). Barrett et al. (1996), for example, demonstrated that the combination of individual CBT with an added family component was superior to individual CBT alone in young children with anxiety disorders (ages 7–10 years), but not in older children (ages 11–14 years), as measured by the proportion of participants who were diagnosis-free following treatment. This finding also persisted at 12-month follow-up. Another CBT PT group intervention with parents of anxious children, aged 9 years or younger, found that children whose parents participated in the intervention evidenced less anxiety post-treatment than children whose parents were in the control group (Cartwright-Hatton et al. 2010). These gains were also maintained at 12-month follow-up.
As demonstrated above, a wide variety of studies on an extensive range of childhood disorders have evidenced results supporting PT in many forms. Impacts range from reduced symptomology or improved quality of peer relationships for the child to improved adjustment in the parent. Several studies also demonstrated the superiority of the combination of PT with routine treatment in comparison to routine treatment alone, particularly in young children. Thus, there is substantial evidence in support of the value of behavioral and cognitive–behavioral PT programs for childhood disorders including ADHD, anxiety disorders, and disruptive/oppositional behaviors.
PT with ASD
PT treatments clearly have demonstrated value for children who suffer from various disorders of childhood; their counterparts in the field of ASD interventions have developed more recently, within the past 5–10 years. In the past, autism was theorized to be caused by parental psychopathology, especially emotionally detached “refrigerator mothers” (Bettelheim 1967). In contrast, contemporary science recognizes the structural and functional neural differences in children with and without ASD (see Buxbaum and Hof 2013). Today, parents are embraced and considered to be a valuable part of the therapy session. Parents are an important, readily accessible resource and can be co-therapists in the home. For multiple reasons, including the need to start treatment early and intensively to maximize benefits, it has become cost-effective to use parents as a way to practice new skills, generalize skills between the therapeutic setting and the home, and maintain gains.
It has become increasingly apparent that intensive behavioral treatment of 20 to 40 h per week leads to the most positive gains in children with ASD (Smith 2010). However, this represents a significant financial and time investment for families. While private insurance companies may cover some portions of these expenses, rarely are families reimbursed for all treatment expenses (Anan et al. 2008). Families without private insurance often struggle to acquire any type of therapy for their child, much less 20–40 h per week.
As a result, using parents as co-therapists has become a valuable way to increase the intensity of therapy and often supplements clinician-provided therapies. In this way, the many social and communication skills that young children with ASD struggle to learn are taught and practiced across multiple settings, including the naturalized home environment. Additionally, once trained, parents are often able to teach other family members or caretakers to work with the child, creating further opportunities for learning and a wider network of co-therapists (Koegel and Koegel 2006; Koegel et al. 2010). Group therapy formats with PT components have also been used as a cost-effective and efficacious way of educating parents (Brookman-Frazee et al. 2009). Groups allow professionals to provide therapy for more families at one time, increasing their availability and thereby serving the community more effectively.
Many children with ASD do not receive a diagnosis until they are toddlers or preschool age. At this point, prior to school enrollment, the child is less likely to be involved in specialized services such as outside therapy or HeadStart. Therefore, the parent is the “first line of defense” and can begin to work towards treatment gains starting from the initial diagnosis. It has been found that treatments are more powerful when they begin early, as soon as possible after diagnosis (Smith 2010). Before formal or structured programs of treatment can be arranged, the parent is the child’s window to the world, and many parents use informal techniques to teach their child with ASD about the social world around them. Additionally, while teachers change yearly and therapists have a high turnover rate, the parent is likely to be the most consistent figure throughout the child’s development (McConachie and Diggle 2007; Koegel et al. 2010). Parents are more likely to have insight into their child’s needs and motivations, further underscoring the importance of utilizing parents as a resource in the therapeutic environment.
Targets of programs designed for children/adolescents with ASD that incorporate PT include social skills (Beaumont and Sofronoff 2008), anxiety (Reaven et al. 2012; Sofronoff et al. 2005; Storch et al. 2013; Wood et al. 2009), anger (Sofronoff et al. 2007), and both anxiety and social skills (White et al. 2010). However, CBT programs for children with ASD that include PT are generally lacking in the early childhood (i.e., 5–7-year-old) age range.
Additional Factors Contributing to the Success of PT in Children with ASD
The Positive Influence of PT on Parents
Brookman-Frazee et al. (2009) noted that parents who are intentional and dedicated to treatment, and who consistently attend sessions, are found to elicit more improvements in their children. Parents with clinically significant levels of stress in their life (e.g., marital discord, depression, negative affect, etc.) showed poorer child outcomes as compared with parents without clinically elevated levels of stress (Robbins et al. 1991). Although these types of stress may inhibit the parent’s ability to serve as a co-therapist, these stressors are not typically targets of treatment in PT. Parental stress often accompanies an ASD diagnosis, and decreases in parental stress are viewed as positive secondary outcomes as the child achieves treatment goals (Koegel et al. 1996; Rezendes and Scarpa 2011).
Conversely, when treating disruptive behavior disorders, it is thought that parental psychopathology may exacerbate the child’s externalizing behaviors and that treating the source of the parent’s mental health issues may result in fewer child behavioral difficulties (Brookman-Frazee et al. 2009). In fact, PT in treatment of children with ASD has been to shown to be associated with not only improved child outcomes, but with improvements in parental mental health and adjustment (Tonge et al. 2006), including increased positive affect (Koegel et al. 1996; Schreibman et al. 1991), reduced stress (Moes 1995), reduced symptoms of depression in mothers (Blackledge and Hayes 2006; Bristol et al. 1993), and increased feelings of parent self-efficacy and confidence (Sofronoff and Farbotko 2002; Pillay et al. 2011). As parents of children with ASD are more likely to have parenting stress than the parents of TD children (Sanders and Morgan 1997; Dabrowska and Pisula 2010; Estes et al. 2013), children with Down syndrome (Sanders and Morgan 1997), or children with developmental delay (Estes et al. 2013), any potential stress relief for parents would be beneficial.
In a meta-analysis of 17 PT programs for developmental disabilities, four of which were autism-specific, Singer et al. (2007) found evidence that PT successfully decreased parental stress, especially depressive symptoms. Parent–child interactions also improved after PT interventions. For example, Koegel et al. (2002) implemented a short-term, intensive PT program for families who were geographically distant from the autism center. After 25 h of training, parents returned home to implement the pivotal response treatment (PRT) skills they had learned. On follow-up (ranging from 3 to 12 months after completion), the authors found that parents had successfully generalized and maintained the PRT skills in the home environment. Participation in the PT program led to improvements in child expressive language, parent affect during parent–child interactions, and parent fidelity in treatment techniques. Laski et al. (1988) found that parents were able to generalize the skills they had learned through ASD-specific PT to TD siblings. These studies suggest that parental factors, such as stress and affect, are important to consider and may improve when PT is included in the treatment of children with ASD.
In treatment of ASD symptoms, the lack of focus on parenting style and techniques directly contrasts with treatment models for other externalizing disorders (Brookman-Frazee et al. 2009), which aim to specifically identify maladaptive patterns of parenting and correct them. Although the PT interventions for both sets of disorders provide direct instruction to build skills in parents, they differ in their rationale for PT. That is, parenting behaviors are viewed as a possible source of child difficulties in the externalizing disorders, whereas parents are viewed as agents of change in ASD. In fact, in models such as PRT ; Koegel et al. 2010), parents are not viewed simply as a possible resource, but rather as eventually becoming the primary clinician. Once parents have been taught the key skills needed to shape the child’s behavior, they are able to put as much work into the process as they choose.
With regard to specific child factors that may be implicated, Puleo and Kendall (2011) investigated the use of CBT to treat children with TD who had been diagnosed with an anxiety disorder. In this study, the authors also measured subclinical symptoms of ASD in child participants through parent report. Puleo and Kendall concluded that TD children with moderate levels of ASD symptomology responded better to family CBT than to individual CBT. As such, parent involvement may serve as a necessary bridge to successful skill acquisition in children with at least moderate levels of parent-reported ASD symptomology. Future empirical research should continue to explore the function of parent involvement and training in child-focused treatment.
Delivery Factors
Specific delivery factors have been implicated in the success of PT in ASD samples, separate from content. Findings regarding the fidelity of parent-implemented treatment are mixed. Some studies urge caution when using PT models, as efficacy can be hindered by the quality of parent-implemented treatment, especially as compared with clinician-implemented models (Bibby et al. 2001; Mudford et al. 2001; Symes et al. 2006). Other studies have conversely found high fidelity in PT models (e.g., Koegel et al. 2002; Koegel et al. 1996; Koegel et al. 1991; Laski et al. 1988).
It is thought that improvements in training, such as intensive, “hands-on” models and significant follow-up, may improve treatment fidelity (Research Units on Pediatric Psychopharmacology (RUPP) Autism Network 2007). Having parents model new skills in vivo during therapy sessions has been shown to have larger treatment effects than interventions that did not emphasize practice during the session, when controlling for content and delivery approach (Kaminski et al. 2008). Kaminski and colleagues, as well as others (Ingersoll and Dvortcsak 2006; Kaiser and Hancock 2003), have suggested that clinician feedback is a crucial piece of in-session practice; feedback that was concise, mostly positive, frequent, and immediate was most successful. The actual practice itself has also been found to be more helpful than merely modeling a skill (Ingersoll and Dvortcsak 2006).
Therapist Factors
Multiple therapist factors may be important when working closely with parents. Although not proven, a number of variables have been suggested for further investigation, including a responsive and cooperative teaching format, firm knowledge of the treatment protocol, ability to provide immediate feedback, personalization of the protocol to each family, acknowledging parent feelings as valid, and listening to parent feedback and concerns (Kaiser and Hancock 2003; Ingersoll and Dvortcsak 2006). When building rapport, it also might be important that the therapist not align him-/herself with one specific parent in the family, at the cost of possibly alienating the other parent (Ingersoll and Dvortcsak 2006).
STAMP as a Program Example
STAMP Overview
STAMP (Scarpa et al. 2013a) is a 9-week group-based CBT program that treats emotional dysregulation in children with HFA. This program serves children between the ages of 5 and 7 years and is a developmental modification of the Exploring Feelings CBT program (Attwood 2004a, b), which targets children with ASD between the ages of 9 and 13 years (Sofronoff et al. 2005, 2007). Self-regulation of emotions is targeted through teaching cognitive, social, physical, and relaxation skills (presented as tools in a metaphorical emotional toolbox) to the children, in combination with affective education. In addition, parents meet simultaneously to become more knowledgeable about the skills that their children are learning and to help promote the generalization of skills in the home.
The overall goal of the PT portion of STAMP is to generalize skills from the child sessions to settings outside of the clinic using instruction, modeling, and home practice. Parents are in an optimal position to scaffold learning because they accompany their child throughout their daily routines at home and other settings where skills may be practiced (e.g., church, grocery store, transporting child between activities, etc.). Generalization is supported by (1) training parents on the skills that are being taught to their children and (2) providing homework assignments that promote the use of skills. The parent therapist reviews and reinforces the coping skills that are taught in STAMP rather than teaching parents to directly change their child’s behavior, as is seen in many other behavioral therapies with parental involvement. Instruction is provided through discussion with the parents and viewing the child session through a television monitor. In this way, the parent is able to directly view child therapists modeling the tools with their child (e.g., teaching the child about relaxation), and the parents have immediate access to the parent therapist to address any questions or concerns.
STAMP is designed to teach emotion-based self-regulatory skills to young children with ASD. That is, the focus is to teach children what they themselves can do to help understand and manage their emotions so that they can problem-solve, reduce distress, avoid punishment or injury, and develop friendships. STAMP does not teach extrinsic factors to regulate emotions (e.g., parental comforting), except insofar as it instructs the children on how to seek those extrinsic factors if needed (e.g., asking for help). As such, parents are viewed as facilitators of change (i.e., coaches) through their help with practice and generalization, but they are not considered the causes of change.
The parent therapist also has the opportunity to elicit more information from the parent in order to individualize skills to the child (e.g., what motivates or calms the child, which skills were most helpful). After receiving training on a full array of emotion regulation strategies, parents are encouraged to practice them with their child and monitor which strategies are particularly effective for their child. Knowledge and practice of all the tools promotes their flexible use, which is needed because their effectiveness may change across time and contexts. Finally, home practice assignments are provided each week, with a large portion of each session devoted to discussing these assignments. Parents are asked to help their child work through the home projects and note any areas of difficulty. By sharing this insight with the group, the therapist is then able to tailor the treatment to the individual child’s needs.
It is also important to note what is not included in the PT portion of STAMP. Although parents are often supportive of one another and provide helpful suggestions, STAMP is not designed to be a support group. Most of the session is spent on learning skills directly related to emotion management and reviewing homework, rather than discussing developmental issues or other child or family difficulties related to ASD. STAMP also does not use ABA as the primary approach, though some behavioral strategies are indeed used and integrated with cognitive strategies. As a CBT, this group focuses instead on affective education and proactive skill-building that can be used to cope with intense negative emotions and prevent the escalation of outbursts, rather than the typical functional analysis of antecedent–behavior–consequences used in ABA. Lastly, parents are clearly told that this program is not intended to cure autism but will provide tools to increase success in understanding and managing feelings.
As such, we present STAMP as an example of an innovative program that uses both cognitive and behavioral elements within a group setting. To our knowledge, STAMP was the first program to use a CBT approach to treat emotional dysregulation symptoms in young children with ASD. STAMP aims to fill this need for young children with ASD who struggle to control their anger and anxiety and may serve as a model for the development of similar CBT programs that wish to include a PT component. Current and future projects are examining the “active ingredients” of STAMP, especially the PT focus, as we seek to apply STAMP principles to other settings (e.g., schools) and populations (e.g., nonverbal children, young adults).
The Development of STAMP
STAMP is based on the Exploring Feelings program (Attwood 2004a, b), and was developmentally adapted for 5–7-year-old children with HFA by including shorter sessions, longer program duration, inclusion of parents, and games/activities designed for young children. In addition, the CBT approach was adapted for verbally limited children to include pictures and visual supports such that every verbal concept in the intervention is accompanied by a visual aid. Proof-of-concept for STAMP’s effectiveness was performed in two steps. The first step included development of an initial working manual through therapy with a group of four children. At this time, the main goal was to modify the Exploring Feelings program with consideration to the cognitive level and preferred activities of early school-aged children.
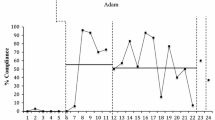
In the second step, the manual was used in a between-groups efficacy study, which included 11 children with ASD (two girls, nine boys) randomly assigned to treatment (n = 5) or to a wait-list (n = 6) condition (Scarpa and Reyes 2011). Outcome measures were taken pre- and immediately post-intervention for both conditions, and then again for the wait-list group after receiving treatment. Measures included parent observations of frequency (i.e., episodes per hour) and duration (in minutes) of behavioral outbursts, parent-reported emotional lability and regulation on the Emotion Regulation Checklist (Shields and Cicchetti 1997, 1998), and child generation of coping strategies in response to vignettes made for this research study. Finally, parents were asked to rate their level of confidence in themselves to manage their child’s emotions and their confidence in their child to manage his/her own emotions, and to rate their satisfaction with the program. Overall results supported benefits of STAMP. Compared with the wait-list group, children in STAMP exhibited a trend towards shorter outbursts (ES = 0.45 and 0.46, respectively) and significantly increased knowledge of appropriate coping strategies after treatment (ES = 0.65). Parents also reported improved confidence in themselves and their child to manage anger and anxiety relative to the control group (ES = 0.63 to 0.89). When comparing the whole sample from pre- to post-treatment in a within subjects analysis, both groups also demonstrated significantly less negative affect, paired t(10) = 2.03, p < .10, and a trend towards better emotion regulation, paired t(10) = 1.45, p < .05, after treatment.
In a consumer satisfaction survey, all parents reported being satisfied to very satisfied with the STAMP program. Qualitative feedback from parents after the program’s completion described previous attempts at emotion labeling but referred to STAMP as the “missing piece” that instructed the parent in how to help her child reduce his level of anger or anxiety. Parents reported enjoying learning the “tools” and benefiting from the discussion in the PT portion of treatment. Parents were also appreciative of the setup that allowed them to concurrently observe the child session from the PT/observation room. Parent feedback has been incorporated into the iterative development of STAMP over time and has improved the program’s design and outcome.
After collecting data from participants in the feasibility study and small RCT described above, the protocol was modified based on parent and therapist input. For example, the story and video used at the end of the 9-week program were lengthened. The story and video are created with the children as characters who are displaying or practicing the various STAMP tools and then distributed to each child to aid in maintenance of skills after treatment has ended. Therapists also suggested ways to enhance the teaching of cognitive tools through card games, because perspective-taking and reappraisal skills are particularly difficult for children with ASD. Finally, parents and therapists suggested the addition of more role-plays in order to practice the skills in session. These suggestions have improved the program and were incorporated in the manual as it was being developed and refined; the manual was published in 2013 (Scarpa et al. 2013b).
Lessons Learned
Some specific lessons have been learned by including parents in STAMP. First, the philosophical stance behind parent inclusion and the goals of STAMP was clarified. We believe that children with ASD can be directly taught cognitive–behavioral strategies of emotion regulation through affective education, skill-building, and cognitive restructuring, so they can learn to self-soothe in emotional situations. By the same token, it is inherently challenging for children with ASD to generalize skills to outside the setting in which those skills are taught. As such, we firmly believe that parents are critical facilitators of generalization by promoting and reinforcing practice of the child’s self-regulatory skills in the home and other settings.
Second, STAMP uses a CBT framework. Therefore, parents with extensive involvement in ABA treatments had to be reminded that STAMP does not use the principles of traditional ABA (e.g., errorless learning, physical prompting, functional behavior analysis). Whereas a traditional ABA approach might focus on understanding the antecedents and consequences that initiate and maintain the child’s behavior, STAMP uses strategies to teach children how to manage the emotion that may underlie the behavior. For example, if a child typically tantrums when taking a test at school, ABA may focus on differential reinforcement that ignores tantrums while reinforcing test-taking. STAMP, on the other hand, would focus on teaching the child to recognize signs of anxiety that may underlie the behavior and utilize tools to manage the anxiety. We found it important to discuss these differences in approach and to emphasize proactive prevention and skill-building in STAMP rather than a focus on changing consequences after the behavior.
Third, it was clear that home assignments needed to be individualized throughout treatment in order to fit the preferences and learning styles of different children. For example, for one child who loved numbers, we used number labels in as many homework assignments as possible. For another child that had a special interest in road signs, the parent found miniature road signs from a train set to use during especially stressful activities. One child seemed to comprehend material better from experiential learning than from pictures, and his parents began to use charades games to teach him about emotions. We found that such individualization was best done through discussion of the home practice assignments and asking all parents to provide suggestions on how to personalize activities to be more appropriate for each child.
Lastly, although not a focus of the PT component in STAMP, different parenting characteristics had to be addressed in the PT groups. Some parents, for example, had low confidence in their child’s abilities and needed to be challenged to try some new strategies. Others had high expectations and viewed their child’s behavior as failure despite small steps being made toward improvement; these parents benefited from reminders to look at the full process of change. In some cases, parents inadvertently reinforced anxiety or aggression in their child by succumbing to persistent child requests/demands, and these parents were encouraged instead to remind their child to use the STAMP tools to help their child cope in those situations. In sum, the parents with whom we have had the privilege to work have taught us invaluable lessons about the goals and philosophy of STAMP as well as its effective implementation or delivery.
Conclusions
STAMP shows a number of differences when compared with pre-existing treatments with a PT component, highlighting its unique contribution to the field. A pivotal difference is the use of both cognitive and behavioral strategies throughout the course of treatment, while other treatments are predominantly behaviorally based. In STAMP, parents are viewed as co-facilitators and stakeholders in the treatment, rather than individuals who need to be corrected in their parenting techniques. As discussed in depth above, treating parents as co-therapists allows them to take an active role in treatment and helps generalize and maintain skills from therapy sessions to the home. While the STAMP parent group is not a support group, it does employ a welcoming and non-critical atmosphere, in order to encourage open discussion and troubleshooting between parents. This is a departure from other interventions, whose specific aims are to “fix” a parent’s ways of teaching his or her child.
Additionally, STAMP incorporates work directly with the child, while many behavior therapy models often work only through parent components. We believe that the use of both parent and child groups is one of the key ingredients that makes STAMP valuable, but additional trials with larger sample sizes and more diverse participants are required to explore this idea further. Moreover, it is possible that STAMP can be used in other settings (e.g., schools), where parents are not available. In these cases, caregiver-based assistance by other school personnel may take on more importance. The utility of the parent component across ages, diagnoses, functional severity, and developmental stages also remains to be seen, as does the utility of an expanded range of measures that might reduce reliance on parent report. Home practice assignments are another important aspect of STAMP, as they create opportunities for parents and children to review and practice skills that were learned in session. This review aids in making the skills concrete and applicable to the child’s life.
Greater focus on the use of PT in CBT will result in improvements in the way we are able to address oppositional, emotional, and behavioral difficulties in young children with ASD. It is our hope through this review of PT in general and discussion of STAMP in particular to show the merit of combining CBT strategies with a PT component and thus to foster continued development of similar combined programs for young children with ASD.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author
Anan, R. M., Warner, L. J., McGillivary, J. E., Chong, I. M., & Hines, S. J. (2008). Group intensive family training (GIFT) for preschoolers with autism Spectrum disorders. Behavioral Interventions, 23(3), 165–180. doi:10.1002/bin.262.
Attwood, T. (2004a). Exploring Feelings: Cognitive Behaviour Therapy to Manage Anger. Arlington: Future Horizons, Inc.
Attwood, T. (2004b). Exploring Feelings: Cognitive Behaviour Therapy to Manage Anxiety. Arlington: Future Horizons, Inc.
Barrett, P. M., Dadds, M. R., & Rapee, R. M. (1996). Family treatment of childhood anxiety: a controlled trial. Journal of Consulting and Clinical Psychology, 64, 333–334. doi:10.1037/0022-006X.64.2.333.
Beaumont, R., & Sofronoff, K. (2008). A multi-component social skills intervention for children with Asperger syndrome: the Junior Detective Training Program. Journal of Child Psychology and Psychiatry, 49(7), 743–753. doi:10.1111/j.1469-7610.2008.01920.x.
Bettelheim, B. (1967). The empty fortress: infantile autism and the birth of the self. New York: Free Press.
Bibby, P., Eikeseth, S., Martin, N. T., Mudford, O. C., & Reeves, D. (2001). Progress and outcomes for children with autism receiving parent-managed intensive interventions. Research in Developmental Disabilities, 22(6), 425–447. doi:10.1016/S0891-4222(01)00082-8.
Blackledge, J. T., & Hayes, S. C. (2006). Using acceptance and commitment training in the support of parents of children diagnosed with autism. Child & Family Behavior Therapy, 28(1), 1–18.
Bristol, M. M., Gallagher, J. J., & Holt, K. D. (1993). Maternal depressive symptoms in autism: response to psychoeducational intervention. Rehabilitation Psychology, 38(1), 3–10.
Brookman-Frazee, L., Vismara, L., Drahota, A., Stahmer, A., & Openden, D. (2009). Parent training interventions for children with Autism Spectrum disorders. In J. L. Matson (Ed.), Applied Behavior Analysis for Children with Autism Spectrum Disorders (pp. 237–257). New York, NY: Springer. doi:10.1007/978-1-4419-0088-3_14.
Buxbaum, J. D., & Hof, P. R. (Eds.). (2013). The neuroscience of autism spectrum disorders. Waltham: Academic.
Cartwright-Hatton, S., McNally, D., Field, A. P., Rust, S., Laskey, B., Dixon, C., & Woodham, A. (2010). A new parenting-based group intervention for young anxious children: results of a randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 50(3), 242–251. doi:10.1016/j.jaac.2010.12.015.
Centers for Disease Control and Prevention. (2014). Prevalence of autism Spectrum Disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2010. Morbidity and Mortality Weekly Report: Surveillance Summaries, 63(2), 1–22.
Conners, N. A., Edwards, M. C., & Grant, A. S. (2007). An evaluation of a parenting class curriculum for parents of young children: parenting the strong-willed child. Journal of Child and Family Studies, 16(3), 321–330. doi:10.1007/s10826-006-9088-z.
Dabrowska, A., & Pisula, E. (2010). Parenting stress and coping styles in mothers and fathers of pre-school children with autism and Down syndrome. Journal of Intellectual Disability Research, 54(3), 266–280. doi:10.1111/j.1365-2788.2010.01258.x.
Dawson, G., & Burner, K. (2011). Behavioral interventions in children and adolescents with autism spectrum disorder: a review of recent findings. Current Opinions in Pediatrics, 23, 616–620. doi:10.1097/MOP.0b013e32834cf082.
Estes, A., Rivera, V., Bryan, M., Cali, P., & Dawson, G. (2011). Discrepancies between academic achievement and intellectual ability in higher-functioning school-aged children with autism spectrum disorder. Journal of Autism and Developmental Disorders, 41(8), 1044–1052. doi:10.1007/s10803-010-1127-3.
Estes, A., Olson, E., Sullivan, K., Greenson, J., Winter, J., Dawson, G., & Munson, J. (2013). Parenting-related stress and psychological distress in mothers of toddlers with autism spectrum disorders. Brain & Development, 35(2), 133–138. doi:10.1016/j.braindev.2012.10.004.
Fabiano, G. A., Pelham, W. E., Cunningham, C. E., Yu, J., Gangloff, B., Buck, M., & Gera, S. (2012). A waitlist-controlled trial of behavioral parent training for fathers of children with ADHD. Journal of Clinical Child and Adolescent Psychology, 41(3), 337–345.
Farrugia, S., & Hudson, J. (2006). Anxiety in adolescents with Asperger syndrome: negative thoughts, behavioral problems, and life interference. Focus on Autism & Other Developmental Disabilities, 21(1), 25–35. doi:10.1177/10883576060210010401.
Foster, E. M., Olchowski, A. E., & Webster-Stratton, C. H. (2007). Is stacking intervention components cost-effective? An analysis of the Incredible Years Program. Journal of the American Academy of Child and Adolescent Psychiatry, 46(11), 1414–1424. doi:10.1097/chi.0b013e3181514c8a.
Frankel, F., & Myatt, R. (2003). Children’s friendship training. New York, NY: Brunner- Routledge.
Frankel, F., Myatt, R., Sugar, C., Whitham, C., Gorospe, C. M., & Laugeson, E. (2010). A randomized controlled study of parent-assisted Children’s Friendship Training with children having autism spectrum Disorders. Journal of Autism and Developmental Disorders, 40(7), 827–842. doi:10.1007/s10803-009-0932-z.
Henggeler, S. W., & Borduin, C. M. (1990). Family therapy and beyond: a multisystemic approach to treating the behavior problems of children and adolescents. Pacific Grove, CA: Brooks/Cole Publishing Company.
Higgins, K. K., Koch, L. C., Boughfman, E. M., & Vierstra, C. (2008). School-to-work transition and Asperger syndrome. Work: A Journal of Prevention, Assessment, & Rehabilitation, 31(3), 291–298.
Hurlbutt, K., & Chalmers, L. (2004). Employment and adults with Asperger syndrome. Focus on Autism & Other Developmental Disabilities, 19(4), 215–222. doi:10.1177/10883576040190040301.
Ingersoll, B., & Dvortcsak, A. (2006). Including parent training in the early childhood special education curriculum for children with autism Spectrum Disorders. Journal of Positive Behavior Interventions, 8(2), 79–87. doi:10.1177/10983007060080020601.
Kaiser, A. P., & Hancock, T. B. (2003). Teaching parents new skills to support their young children’s development. Infants and Young Children, 16(1), 9–21.
Kaminski, J. W., Valle, L. A., Filene, J. H., & Boyle, C. L. (2008). A meta-analytic review of components associated with parent training program effectiveness. Journal of Abnormal Child Psychology, 36(4), 567–589. doi:10.1007/s10802-007-9201-9.
Kanne, S. M., Gerber, A. J., Quirmbach, L. M., Sparrow, S. S., Cicchetti, D. V., & Saulnier, C. A. (2011). The role of adaptive behavior in autism spectrum disorders: implications for functional outcome. Journal of Autism & Developmental Disorders, 41(8), 1007–1018. doi:10.1007/s10803-010-1126-4.
Kendall, P. C., & Chodhury, M. S. (2003). Children and adolescents in cognitive-behavioral therapy: some past efforts and current advances, and the challenges in our future. Cognitive Therapy and Research, 27(1), 89–104. doi:10.1023/A:1022542814822.
Kendall, P. C., Hudson, J. L., Gosch, E., Flannery-Schroeder, E., & Suveg, C. (2008). Cognitive–behavioral therapy for anxiety disordered youth: a randomized clinical trial evaluating child and family modalities. Journal of Consulting and Clinical Psychology, 76(2), 282–297. doi:10.1037/0022-006X.76.2.282.
Klin, A., Saulnier, C. A., Sparrow, S. S., Cicchetti, D. V., Volkmar, F. R., & Lord, C. (2007). Social and communication abilities and disabilities in higher functioning individuals with autism Spectrum disorders: the Vineland and the ADOS. Journal of Autism and Developmental Disorders, 37(4), 748–759. doi:10.1007/s10803-006-0229-4.
Koegel, R. L., Bimbela, A., & Schreibman, L. (1996). Collateral effects of parent training on family interactions. Journal of Autism and Developmental Disorders, 26(3), 347–359.
Koegel, R. L., & Koegel, L. K. (2006). Pivotal response treatments for autism. Baltimore, MD: Paul H. Brookes.
Koegel, R. L., Koegel, L. K., & Schreibman, L. (1991). Assessing and training parents in teaching pivotal behaviors. In R. J. Prinz (Ed.), Advances in behavioral assessment of children and families (pp. 65–82). Greenwich, CT: JAI Press.
Koegel, R. L., Koegel, L. K., Vernon, T. W., & Brookman-Frazee, L. I. (2010). Empirically supported pivotal response treatment for children with autism spectrum disorders. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed.). New York: Guilford.
Koegel, R. L., Symon, J. B., & Koegel, L. K. (2002). Parent education for families of children with autism living in geographically distant areas. Journal of Positive Behavior Interventions, 4(2), 88–103. doi:10.1177/109830070200400204.
Landa, R. (2000). Social language use in Asperger syndrome and high-functioning autism. In A. J. M. Klin, F. R. Volkmar, & S. S. Sparrow (Eds.), Asperger Syndrome (pp. 125–156). New York, NY: Guilford Press.
Laugeson, E. A., Frankel, F., Gantman, A., Dillon, A. R., & Mogil, C. (2012). Evidence-based social skills training for adolescents with autism spectrum disorders: the UCLA PEERS program. Journal of Autism and Developmental Disorders, 42, 1025–1036. doi:10.1007/s10803-011-1339-1.
Laski, K. E., Charlop, M. H., & Schreibman, L. (1988). Training parents to use the Natural Language Paradigm to increase their autistic children’s speech. Journal of Applied Behavior Analysis, 21(4), 391–400. doi:10.1901/jaba. 1988.21-391.
Levy, S. E., Giarelli, E., Lee, L.-C., Schieve, L. A., Kirby, R. S., Cunniff, C., Nicholas, J., Reaven, J., & Rice, C. E. (2010). Autism spectrum disorder and co-occurring developmental, psychiatric, and medical conditions among children in multiple populations of the United States. Journal of Developmental & Behavioral Pediatrics, 31(4), 267–275. doi:10.1097/DBP.0b013e3181d5d03b.
Long, N., & Forehand, R. (2002). Parenting the strong-willed child: leader’s guide for the six week parenting class, Version 2.0. Unpublished manual.
Lovaas, O. I. (1987). Behavioral treatment and normal educational and intellectual functioning in young autistic children. Journal of Consulting and Clinical Psychology, 55(1), 3–9.
Mayes, S. D., Calhoun, S. L., Murray, M. J., & Zahid, J. (2011). Variables associated with anxiety and depression in children with autism. Journal of Developmental and Physical Disabilities, 23(4), 325–337. doi:10.1007/s10882-011-9231-7.
McCart, M. R., Priester, P. E., Davies, W. H., & Azen, R. (2006). Differential effectiveness of behavioral parent-training and cognitive–behavioral therapy for antisocial youth: a meta-analysis. Journal of Abnormal Child Psychology, 34(4), 527–543. doi:10.1007/s10802-006-9031-1.
McConachie, H., & Diggle, T. (2007). Parent implemented early intervention for young children with autism spectrum disorder: a systematic review. Journal of Evaluation in Clinical Practice, 13(1), 120–129. doi:10.1111/j.1365-2753.2006.00674.x.
McIntyre, L. L. (2008). Adapting Webster-Stratton’s Incredible Years parent training for children with developmental delay: findings from a treatment group only study. Journal of Intellectual Disability Research, 52(12), 1176–1192. doi:10.1111/j.1365-2788.2008.01108.x.
Mikami, A. Y., Lerner, M. D., Griggs, M. S., McGrath, A., & Calhoun, C. D. (2010). Parental influence on children with attention-deficit/hyperactivity disorder: II. Results of a pilot intervention training parents as friendship coaches for children. Journal of Abnormal Child Psychology, 38(6), 737–749. doi:10.1007/s10802-010-9403-4.
Miller, L. S., & Rojas-Flores, L. (1999). Preventing conduct problems in urban, Latino preschoolers through parent training: a pilot study. New York, NY: New York University Child Study Center.
Minshew, N. J., Goldstein, G., Taylor, H. G., & Siegel, D. J. (1994). Academic achievement in high functioning autistic individuals. Journal of Clinical and Experimental Neuropsychology, 16(2), 261–270. doi:10.1080/01688639408402637.
Moes, D. (1995). Parent education and parenting stress. In R. L. Koegel & L. K. Koegel (Eds.), Teaching Children with Autism: Strategies for Initiating Positive Interactions and Improving Learning Opportunities (pp. 79–93). Baltimore, MD: Paul H. Brookes.
Mudford, O. C., Martin, N. T., Eikeseth, S., & Bibby, P. (2001). Parent-managed behavioral treatment for preschool children with autism: some characteristics of UK programs. Research in Developmental Disabilities, 22(3), 173–182. doi:10.1016/S0891-4222(01)00066-X.
Ogden, T., & Hagen, K. A. (2008). Treatment effectiveness of parent management training in Norway: a randomized controlled trial of children with conduct problems. Journal of Consulting and Clinical Psychology, 76(4), 607–621. doi:10.1037/0022-006X.76.4.607.
Patterson, G. R. (2005). The next generation of PMTO models. Behavior Therapist, 28(2), 27–33.
Paul, R., Orlovski, S. M., Marcinko, H. C., & Volkmar, F. (2009). Conversational behaviors in youth with high-functioning ASD and Asperger syndrome. Journal of Autism and Developmental Disorders, 39(1), 115–125. doi:10.1007/s10803-008-0607-1.
Pillay, M., Alderson-Day, B., Wright, B., Williams, C., & Urwin, B. (2011). Autism Spectrum Conditions-Enhancing Nurture and Development (ASCEND): an evaluation of intervention support groups for parents. Clinical Child Psychology and Psychiatry, 16(1), 5–20. doi:10.1177/1359104509340945.
Puleo, C. M., & Kendall, P. C. (2011). Anxiety disorders in typically developing youth: autism spectrum symptoms as a predictor of cognitive–behavioral treatment. Journal of Autism and Developmental Disorders, 41(3), 275–286. doi:10.1007/s10803-010-1047-2.
Reaven, J., Blakeley-Smith, A., Leuthe, E., Moody, E., & Hepburn, S. (2012). Facing your fears in adolescence: cognitive–behavioral therapy for high-functioning autism spectrum disorders and anxiety. Autism Research and Treatment, 1–13. doi:10.1155/2012/423905.
Reaven, J., & Blakeley-Smith, A. (2013). Parental involvement in treating anxiety in youth with high-functioning ASD. In A. Scarpa, S. W. White, & T. Attwood (Eds.), CBT for children and adolescents with high-functioning autism Spectrum disorders (pp. 3–26). New York: Guilford.
Research Units on Pediatric Psychopharmacology (RUPP) Autism Network. (2007). Parent training for children with pervasive developmental disorders: a multi-site feasibility trial. Behavior Interventions, 22(3), 179–199. doi:10.1002/bin.
Rezendes, D. L., & Scarpa, A. (2011). Associations between parental anxiety/depression and child behavior problems related to autism spectrum disorders: the roles of parenting stress and parenting self-efficacy. Autism Research and Treatment, 1–10. doi:10.1155/2011/395190.
Robbins, F. R., Dunlap, G., & Plienis, A. J. (1991). Family characteristics, family training, and the progress of young children with autism. Journal of Early Intervention, 15(2), 173–184. doi:10.1177/105381519101500206.
Sanders, J. L., & Morgan, S. B. (1997). Family stress and adjustment as perceived by parents of children with autism or Down syndrome: implications for intervention. Child & Family Behavior Therapy, 19(4), 15–32. doi:10.1300/J019v19n04_02.
Scahill, L., Sukhodolsky, D. G., Bearss, K., Findley, D., Hamrin, V., Carroll, D. H., & Rains, A. L. (2006). Randomized trial of parent management training in children with tic disorders and disruptive behavior. Journal of Child Neurology, 21(8), 650–656. doi:10.1177/08830738060210080201.
Scarpa, A., & Lorenzi, J. (2013). Cognitive–behavioral therapy with children and adolescents: history and principles. In A. Scarpa, S. W. White, & T. Attwood (Eds.), CBT for children and adolescents with high-functioning autism spectrum disorders (pp. 3–26). New York, NY: Guilford.
Scarpa, A., & Reyes, N. (2011). Improving emotion regulation with CBT in young children with high functioning Autism Spectrum disorders: a pilot study. Behavioural and Cognitive Psychotherapy, 39, 495–500. doi:10.1017/S1352465811000063.
Scarpa, A., Wells, A. O., & Attwood, T. (2013a). Exploring feelings for young children with high-functioning autism or Asperger’s disorder: the STAMP treatment manual. London, UK: Jessica Kingsley Publishers.
Scarpa, A., White, S. W., & Attwood, T. (Eds.). (2013b). CBT Interventions for Children and Adolescents with High-Functioning Autism Spectrum Disorders. New York, NY: Guilford.
Schreibman, L., Kaneko, W. M., & Koegel, R. L. (1991). Positive affect of parents of autistic children: a comparison across two teaching techniques. Behavior Therapy, 22(4), 479–490. doi:10.1016/S0005-7894(05)80340-5.
Serketich, W. J., & Dumas, J. E. (1996). The effectiveness of behavioral parent training to modify antisocial behavior in children: a meta-analysis. Behavior Therapy, 27(2), 171–186. doi:10.1016/S0005-7894(96)80013-X.
Shields, A., & Cicchetti, D. (1997). Emotion regulation among school age children: the development and validation of a new criterion Q-sort scale. Developmental Psychology, 33, 906–916.
Shields, A., & Cicchetti, D. (1998). Reactive aggression among maltreated children: the contributions of attention and emotion dysregulation. Journal of Clinical Child Psychology, 27, 381–395.
Singer, G. H. S., Ethridge, B. L., & Aldana, S. I. (2007). Primary and secondary effects of parenting and stress management interventions for parents of children with developmental disabilities: a meta-analysis. Mental Retardation and Developmental Disabilities Research Reviews, 13(4), 357–369. doi:10.1002/mrdd.20175.
Smith, T. (2010). Early and intensive behavioral intervention in autism. In J. R. Weisz & A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (2nd ed.). New York: Guilford.
Sofronoff, K., Attwood, T., & Hinton, S. (2005). A randomised control trial of CBT intervention for anxiety in children with Asperger syndrome. Journal of Child Psychology and Psychiatry, 46(11), 1152–1160. doi:10.1111/j.1469-7610.2005.00411.x.
Sofronoff, K., Attwood, T., Hinton, S., & Levin, I. (2007). A randomized controlled trial of cognitive behavioural intervention for anger management in children diagnosed with Asperger syndrome. Journal of Autism and Developmental Disorders, 37(7), 1203–1214. doi:10.1007/s10803-006-0262-3.
Sofronoff, K., & Farbotko, M. (2002). The effectiveness of parent management training to increase self-efficacy in parents of children with Asperger syndrome. Autism, 6(3), 271–286. doi:10.1177/1362361302006003005.
Storch, E. A., Arnold, E. B., Lewin, A. B., Nadeau, J. M., & Jones, A. M. (2013). The effect of cognitive-behavioral therapy versus treatment as usual for anxiety in children with autism spectrum disorders: a randomized, controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 52(2), 132. doi:10.1016/j.jaac.2012.11.007.
Symes, M. D., Remington, B., Brown, T., & Hastings, R. P. (2006). Early intensive behavioral intervention for children with autism. Research in Developmental Disabilities, 27(1), 30–42. doi:10.1016/j.ridd.2004.07.007.
Taylor, T. K., Schmidt, F., Pepler, D., & Hodgins, H. (1998). A comparison of electric treatment with Webster-Stratton’s Parents and Children Series in a children’s mental health center. Behavior Therapy, 29(2), 221–240. doi:10.1016/S0005-7894(98)80004-X.
Tonge, B. J., Brereton, A. V., Gray, K. M., & Einfeld, S. L. (1999). Behavioral and emotional disturbance in high-functioning autism and Asperger syndrome. Autism, 3(2), 117–130.
Tonge, B., Brereton, A., Kiomall, M., Mackinnon, A., King, N., & Rinehart, N. (2006). Effects on parent mental health of an education and skills training program for parents of young children with autism: a randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry, 45, 561–569. doi:10.1097/01.chi.0000205701.48324.26.
van den Hoofdakker, B. J., van der Veen-Mulders, L., Sytema, S., Emmelkamp, P. M. G., Minderaa, R. B., & Nauta, M. H. (2007). Effectiveness of behavioral parent training for children with ADHD in routine clinical practice: a randomized controlled study. Journal of the American Academy of Child and Adolescent Psychiatry, 46(10), 1263–1271. doi:10.1097/chi.0b013e3181354bc2.
Webster-Stratton, C. (1990). Long-term follow-up of families with young conduct problem children: from pre-school to grade school. Journal of Clinical Child Psychology, 19(2), 144–149.
Webster-Stratton, C. (2000). The Incredible Years Training Series (Juvenile Justice Bulletin). Washington, DC: U.S. Department of Justice, Office of Juvenile Justice and Delinquency Prevention.
Webster-Stratton, C., & Hammond, M. (1997). Treating children with early-onset conduct problems: a comparison of child and parent training interventions. Journal of Consulting and Clinical Psychology, 65(1), 93–109. doi:10.1037/0022-006X.65.1.93.
Weisz, J. R., & Kazdin, A. E. (Eds.). (2010). Evidence-based psychotherapies for children and adolescents (2nd ed.). New York: Guilford.
White, S. W., Albano, A. M., Johnson, C. R., Kasari, C., Ollendick, T., Klin, A., & Scahill, L. (2010). Development of a cognitive–behavioral intervention program to treat anxiety and social deficits in teens with high-functioning autism.
White, S. W., Oswald, D., Ollendick, T., & Scahill, L. (2009). Anxiety in children and adolescents with autism spectrum disorders. Clinical Psychology Review, 29(3), 216–229. doi:10.1016/j.cpr.2009.01.003.
Wood, J. J., Drahota, A., Sze, K., Har, K., Chiu, A., & Langer, D. A. (2009). Cognitive behavioral therapy for anxiety in children with autism spectrum disorders: a randomized, controlled trial. Journal of Child Psychology and Psychiatry, 50(3), 224–234. doi:10.1111/j.1469-7610.2008.01948.x.
Conflict of Interest
Dr. Scarpa receives royalties from the publication of the STAMP manual.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hassenfeldt, T.A., Lorenzi, J. & Scarpa, A. A Review of Parent Training in Child Interventions: Applications to Cognitive–Behavioral Therapy for Children with High-Functioning Autism. Rev J Autism Dev Disord 2, 79–90 (2015). https://doi.org/10.1007/s40489-014-0038-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40489-014-0038-1