Abstract
Aims
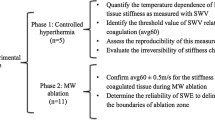
Real-time monitoring of tissue temperature during percutaneous tumor ablation improves treatment efficacy, leading clinicians in adjustment of treatment settings. This study aims at assessing feasibility of ultrasound thermometry during laser ablation of biological tissue using a specific ultrasound imaging techniques based on elastography acoustic radiation force impulse (ARFI).
Methods
ARFI uses high-intensity focused ultrasound pulses to generate ‘radiation force’ in tissue; this provokes tissue displacements trackable using correlation-based ultrasound methods: the sensitivity of shear waves velocity is able to detect temperature changes. Experiments were carried out using a Nd:YAG laser (power: 5 W) in three non-perfused ex vivo pig livers. In each organ, a thermocouple was placed close to the applicator tip (distance range 1.5–2.5 cm) used to record a reference temperature. Positioning of laser applicator and thermocouple was eco-guided. The organ was scanned by an echography system equipped with ARFI; propagation velocity was measured in a region of interest of 1 × 0.5 cm located close to thermocouple, to investigate influence of tissue temperature on shear waves velocity.
Results
Shear wave velocity has a very low sensitivity to temperature up to 55–60 °C, and in all cases, velocity is < 5 m s−1; for temperature > 55–60 °C, velocity shows a steep increment. The system measures a value “over limit”, meaning a velocity > 5 m s−1.
Conclusions
Ultrasound thermometry during laser ablation of biological tissue based on elastography shows an abrupt output change at temperatures > 55–60 °C. This issue can have a relevant clinical impact, considering tumor necrosis when temperature crosses 55 °C to define the boundary of damaged volume.
Graphic abstract






Similar content being viewed by others
Availability of data and materials
Measurements and Biomedical Instrumentation Lab, Università Campus Bio-Medico di Roma; please contact e.schena@unicampus.it or francescogiurazza@hotmail.it
References
Saccomandi P, Schena E, Silvestri S (2013) Techniques for temperature monitoring during laser induced thermotherapy: an overview. Int J Hyperth 29(7):609–619
Schena E, Tosi D, Saccomandi P, Lewis E, Kim T (2016) Fiber optic sensors for temperature monitoring during thermal treatments: an overview. Sensors 16(7):1144
Fani F, Schena E, Saccomandi P, Silvestri S (2008) CT-based thermometry: an overview. Int J Hyperth 30(4):219–227
Rieke V, Butts Pauly K (2008) MR thermometry. J Magn Reson Imaging 27(2):376–390
Azhari H (2012) Feasibility study of ultrasonic computed tomography-guided high-intensity focused ultrasound. Ultrasound Med Biol 38(4):619–625
Parker DL, Smith V, Sheldon P, Crooks LE, Fussell L (1983) Temperature distribution measurements in two-dimensional NMR imaging. Med Phys 10(3):321–325
Weiss N, Sosna J, Goldberg SN, Azhari H (2014) Non-invasive temperature monitoring and hyperthermic injury onset detection using X-ray CT during HIFU thermal treatment in ex vivo fatty tissue. Int J Hyperther 30(2):119–125
Pandeya GD, Klaessens JHGM, Greuter MJW et al (2011) Feasibility of computed tomography based thermometry during interstitial laser heating in bovine liver. Eur Radiol 21(8):1733–1738
Schena E, Saccomandi P, Giurazza F et al (2013) Experimental assessment of CT-based thermometry during laser ablation of porcine pancreas. Phys Med Biol 58(16):5705
Arnal B, Pernot M, Tanter M (2011) Monitoring of thermal therapy based on shear modulus changes: II. Shear wave imaging of thermal lesions. IEEE Trans Ultrason Ferroelectr 8:1603–1611
Sapin-de Brosses E, Gennisson JL, Pernot M, Fink M, Tanter M (2010) Temperature dependence of the shear modulus of soft tissues assessed by ultrasound”. Phys Med Biol 55(6):1701
Mariani A, Kwiecinski W, Pernot M, Balvay D, Tanter M, Clement O et al (2014) Real time shear waves elastography monitoring of thermal ablation: in vivo evaluation in pig livers. J Surg Res 188:37–43
Starritt HC, Duck FA, Humphrey VF (1991) Forces acting in the direction of propagation in pulsed ultrasound fields. Phys Med Biol 36(11):1465
Callé S, Remenieras JP, Bou Matar O, Hachemi ME, Patat R (2005) Temporal analysis of tissue displacement induced by a transient ultrasound radiation force. J Acoust Soc Am 118(5):2829–2840
Schena E, Saccomandi P, Giurazza F, et al. (2013) Monitoring of temperature increase and tissue vaporization during laser interstitial thermotherapy of ex vivo swine liver by computed tomography. In: Conference Proceedings of IEEE Engineering in Medicine and Biological Society, pp 378–381
Saccomandi P, Schena E, Caponero MA et al (2012) Theoretical analysis and experimental evaluation of laser-induced interstitial thermotherapy in ex vivo porcine pancreas. IEEE Trans Bio Med Eng 59(10):2958–2964
Joint Committee for Guides in Metrology, Working Group 1 (JCGM/WG1) (2008) Evaluation of measurement data — Guide to the expression of uncertainty in measurement. www.bipm.org
Ahmed M, Brace CL, Lee FT Jr, Goldberg SN (2011) Principles of and advances in percutaneous ablation. Radiology 258(2):351–369
Livraghi T, Solbiati L, Meloni MF, Gazelle GS, Halpern EF, Goldberg SN (2003) Treatment of focal liver tumors with percutaneous radiofrequency ablation: complications encountered in a multicenter study. Radiology 226(2):441–451
Gervais DA, McGovern FJ, Arellano RS, McDougal WS, Mueller PR (2003) Renal cell carcinoma: clinical experience and technical success with radio-frequency ablation of 42 tumors. Radiology 226(2):417–424
Di Matteo FM, Picconi F, Martino M et al (2014) Endoscopic ultrasound-guided Nd:YAG laser ablation of recurrent pancreatic neuroendocrine tumor: a promising revolution? Endoscopy 46(S01):E380–E381
Frich L (2006) Non-invasive thermometry for monitoring hepatic radiofrequency ablation. Minim Invasiv Ther Allied Technol 15(1):18–25
Paulides MM, Stauffer PR, Neufeld E et al (2013) Simulation techniques in hyperthermia treatment planning. Int J Hyperther 29(4):346–357
Wu T, Felmlee JP, Greenleaf JF, Riederer SJ, Ehman RL (2001) Assessment of thermal tissue ablation with MR elastography. Magn Reson Med 45:80–87
Felicani C, De Molo C, Stefanescu H et al (2018) Point quantification elastography in the evaluation of liver elasticity in healthy volunteers: a reliability study based on operator expertise. J Ultrasound 21(2):89–98
Mulazzani L, Salvatore V, Ravaioli F et al (2017) Point shear wave ultrasound elastography with Esaote compared to real-time 2D shear wave elastography with supersonic imagine for the quantification of liver stiffness. J Ultrasound 20(3):213–225
Righi S, Fiorini E, De Molo C et al (2012) ARFI elastography in patients with chronic autoimmune liver diseases: a preliminary study. J Ultrasound 15(4):226–231
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in studies involving animals were in accordance with the ethical standards of the institution or practice at which the studies were conducted.
Informed consent
For this type of study informed consent is not required. For this type of study consent for publication is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Giurazza, F., Massaroni, C., Silvestri, S. et al. Preliminary analysis of ultrasound elastography imaging-based thermometry on non-perfused ex vivo swine liver. J Ultrasound 23, 69–75 (2020). https://doi.org/10.1007/s40477-019-00407-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-019-00407-z