Abstract
Purpose
Accurate early diagnosis of appendicitis can decrease its complications and minimize the mortality, morbidity and costs. This prospective study evaluates the accuracy of bedside emergency physician performed ultrasound study diagnosis in acute appendicitis.
Methods
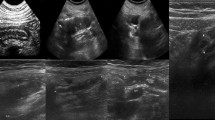
Patients who were suspicious to have appendicitis based on their clinical findings were included and underwent emergency physician performed ultrasound study. Then they were followed up until the recognition of final diagnosis based on pathology report or identification of an alternative diagnosis. Ultrasound studies were done by post-graduate year three emergency medicine residents or emergency medicine attending physicians who were attended in a 4 h didactic and practical course and with 7.5 MHz linear probe both in longitudinal and axial axes.
Results
Ninety-seven patients were included and analyzed. 27 (27.8 %) of patients had appendicitis according to the results of emergency physicians performed ultrasound studies. 19 (70.37 %) of them had appendicitis according to their pathologic reports too. Forty-three (44.3 %) of patients had appendicitis according to pathology reports. Only 19 (44.18 %) of them were diagnosed by emergency physicians. Emergency physician performed ultrasound study had a sensitivity of 44.18 %, specificity of 85.18 %, positive predictive value of 70.37 %, negative predictive value of 65.71 % and overall accuracy of 67.01 % in diagnosing appendicitis in patients clinically suspicious to have acute appendicitis.
Conclusion
Emergency physician performed bedside ultrasound has an acceptable overall accuracy but its sensitivity is low thus it can help emergency physicians to diagnose the acute appendicitis when used in conjunction with other clinical and para-clinical evaluations but not per se.
Riassunto
Scopo
Un’accurata diagnosi precoce di appendicite può diminuirne le complicanze e ridurre al minimo mortalità, morbilità e costi. Questo studio prospettico valuta l’accuratezza della diagnosi ecografica, eseguita in emergenza da un medico, nello studio di appendicite acuta.
Metodi
Sono stati inclusi I pazienti con sospetto clinico di appendicite e sottoposti ad ecografia d’emergenza eseguita da un medico. I pazienti sono stati poi seguiti fino alla diagnosi definitiva, basata su reperti di anatomia patologia o su una diagnosi alternativa. Le ecografie sono state eseguite da residents di medicina con 3 anni post-laurea o da medici di medicina d’urgenza che avevano partecipato ad un corso didattico e pratico di 4 ore, con sonda lineare da 7.5 MHz sia con scansioni longitudinali che assiali.
Risultati
Sono stati inclusi ed esaminati novantasette pazienti. 27 (27,8 %) secondo i risultati delle ecografie effettuate dai medici di emergenza avevano un’appendicite. 19 (70.37 %) di loro avevano un’appendicite anche secondo i risultati dell’anatomia patologica. 43 (44,3 %) pazienti avevano un’appendicite, secondo i risultati dell’anatomia patologica. Solo in 19 (44.18 %) di loro era stata diagnosticata dai medici di emergenza. Lo studio ecografico aveva sensibilità del 44.18 %, specificità del 85.18 %, valore predittivo positivo del 70.37 %, valore predittivo negativo del 65,71 % e accuratezza complessiva del 67.01 % nella diagnosi di appendicite in pazienti clinicamente sospetti per appendicite acuta.
Conclusione
L’ecografia eseguita da un medico di emergenza ha un’accuratezza complessiva accettabile, ma la sua sensibilità è bassa, quindi può aiutare i medici a diagnosticare in emergenza l’appendicite acuta se usata in combinazione con altre valutazioni cliniche e para-cliniche, ma non se esclusiva ed isolata.
Similar content being viewed by others
References
Becker T, Kharbanda A, Bachur R (2007) Atypical clinical features of pediatric appendicitis. Acad Emerg Med 14(2):124–129
Kaiser S, Jorulf H, Söderman E, Frenckner B (2004) Impact of radiologic imaging on the surgical decision-making process in suspected appendicitis in children. Acad Radiol 11(9):971–979
Applegate KE, Sivit CJ, Salvator AE et al (2001) Effect of cross-sectional imaging on negative appendectomy and perforation rates in children. Radiology 220(1):103–107
Seetahal SA, Bolorunduro OB, Sookdeo TC, Oyetunji TA, Greene WR, Frederick W et al (2011) Negative appendectomy: a 10-year review of a nationally representative sample. Am J Surg 201(4):433–437
Doria AS, Moineddin R, Kellenberger CJ, Epelman M, Beyene J, Schuh S et al (2006) US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology 241(1):83–94
van Randen A, Bipat S, Zwinderman AH, Ubbink DT, Stoker J, Boermeester MA (2008) Acute appendicitis: meta-analysis of diagnostic performance of CT and graded compression US related to prevalence of disease. Radiology 249(1):97–106
Terasawa T, Blackmore CC, Bent S, Kohlwes RJ (2004) Systematic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med 141(7):537–546
Pinto F, Pinto A, Russo A, Coppolino F, Bracale R, Fonio P et al (2013) Accuracy of ultrasonography in the diagnosis of acute appendicitis in adult patients: review of the literature. Crit Ultrasound J 5(1):S2
Chen SC, Wang HP, Hsu HY, Huang PM, Lin FY (2000) Accuracy of ED sonography in the diagnosis of acute appendicitis. Am J Emerg Med 18(4):449–452
Mardan MA, Mufti TS, Khattak IU, Chilkunda N, Alshayeb AA, Mohammad AM et al (2007) Role of ultrasound in acute appendicitis. J Ayub Med Coll Abbottabad 19(3):72–79
Incesu L, Coskun A, Selcuk MB, Akan H, Sozubir S, Bernay F (1997) Acute appendicitis: MR imaging and sonographic correlation. Am J Roentgenol 168:669–674
Flum DR, Koepsell T (2002) The clinical and economic correlates of misdiagnosed appendicitis: nationwide analysis. Arch Surg 137:799–804
Nasiri S, Mohebbi F, Sodagari N, Hedayat A (2012) Diagnostic values of ultrasound and the Modified Alvarado Scoring System in acute appendicitis. Int J Emerg Med 5(1):26
Ramachandran P, Sivit CJ, Newman KD, Schwartz MZ (1996) Ultrasonography as an adjunct in the diagnosis of acute appendicitis: a 4-year experience. J Pediatr Surg 31(1):164–167
Brodzisz A, Wieczorek P, Dybiec E, Pietka M, Osemlak J (2003) High frequency ultrasound diagnostics of right lower quadrant abdominal pain in children. Ann Univ Mariae Curie Sklodowska Med 58(1):437–443
Rosendahl K, Aukland SM, Fosse K (2004) Imaging strategies in children with suspected appendicitis. Eur Radiol 14(4):138–145
Hernandez JA, Swischuk LE, Angel CA, Chung D, Chandler R, Lee S (2005) Imaging of acute appendicitis: US as the primary imaging modality. Pediatr Radiol 35(4):392–395
Fox JC, Solley M, Anderson CL, Zlidenny A, Lahham S, Maasumi K (2008) Prospective evaluation of emergency physician performed bedside ultrasound to detect acute appendicitis. Eur J Emerg Med 15(2):80–85
Bramante R, Radomski M, Nelson M, Raio C (2013) Transvaginal imaging of the right adnexa demonstrating a non-compressing, enlarged appendix with an appendicolith (hyperechoic with posterior shadow). West J Emerg Med 14(5):415–418
Lee JH (2003) Sonography of acute appendicitis. Semin Ultrasound CT MR 24(2):83–90
Ang A, Chong NK, Daneman A (2001) Pediatric appendicitis in “real-time”: the value of sonography in diagnosis and treatment. Pediatr Emerg Care 17(5):334–340
Lee JH, Jeong YK, Hwang JC et al (2002) Graded compression sonography with adjuvant use of a posterior manual compression technique in the sonographic diagnosis of acute appendicitis. Am J Roentgenol 178(4):863–868
Conflict of interest
The authors (Seyyed Abbas Hasani, Marzieh Fathi, Mohammad Amin Zare, Marzieh Daadpey, Nader Hojati Firoozabadi, Daniyal Lotfi) have no conflict of interest.
Human and animal studies
The study was conducted in accordance with all institutional and national guidelines for the care and use of laboratory animals.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). All patients provided written informed consent to enrolment in the study and to the inclusion in this article of information that could potentially lead to their identification.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fathi, M., Hasani, S.A., Zare, M.A. et al. Diagnostic accuracy of emergency physician performed graded compression ultrasound study in acute appendicitis: a prospective study. J Ultrasound 18, 57–62 (2015). https://doi.org/10.1007/s40477-014-0130-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-014-0130-5