Abstract
Purpose of Review
Attention deficit hyperactivity disorder (ADHD) is one of the most common neurodevelopmental disorders characterized by inattention, impulsivity, diminished executive functions, and hyperactivity. Objective criteria can be used to assess the diagnosis and response of the disease to medications.
Recent Findings
Several biomarkers belonging to electrophysiological, genetic, peripheral, and miRNA-based biomarkers have shown promise in studies to be an objective aid to clinical diagnostic criteria for the diagnosis of ADHD.
Summary
This review article focuses on summarizing the existing evidence for different biomarkers that have been studied in the past for diagnosing ADHD.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Still G. The Goulstonian lectures on some abnormal physical conditions in children. Lecture 1. Lancet. 1902;i 1008–0102:1077–82 1163–1168.
Douglas VI. Stop, look and listen: the problem of sustained attention and impulse control in hyperactive and normal children. Can J Behav Sci. 1972;4:259–82.
Childress AC, Berry SA. Pharmacotherapy of attention-deficit hyperactivity disorder in adolescents. Drugs. 2012;72:309–25. https://doi.org/10.2165/11599580-000000000-00000.
American Psychiatric Association. Attention-deficit and disruptive behavior disorders. In: Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington: American Psychiatric Association; 2013.
Zametkin AJ, Ernst M. Problems in the management of attention-deficit-hyperactivity disorder. N Engl J Med. 1999;340:40–6.
Mirsky AF, Duncan CC. A nosology of disorders of attention. Ann N Y Acad Sci. 2001;931:17–32.
Daley KC. Update on attention-deficit/hyperactivity disorder. Curr Opin Pediatr. 2004;16:217–26.
Biomarkers Definition Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Therapeutics. 2001;69:89–95.
Jeste SS, Nelson CA 3rd. Event related potentials in the understanding of autism spectrum disorders: an analytical review. J Autism Dev Disord. 2009;39:495–510.
Lubar JF. Discourse on the development of EEG diagnostics and biofeedback for attention-deficit/hyperactivity disorders. Biofeedback Self Regul. 1991;16:201–25.
Monastra VJ, Lubar JF, Linden M. The development of a quantitative electroencephalographic scanning process for attention deficit-hyperactivity disorder: reliability and validity studies. Neuropsychology. 2001;15:136–44.
Snyder SM, Hall JR. A meta-analysis of quantitative EEG power associated with attention-deficit hyperactivity disorder. J Clin Neurophysiol. 2006;23:440–55.
Snyder SM, Quintana H, Sexson SB, Knott P, Haque AFM, Reynolds DA. Blinded, multicenter validation of EEG and rating scales in identifying ADHD within a clinical sample. Psychiatry Res. 2008;159:346–58.
Buyck I, Wiersema JR. Resting electroencephalogram in attention deficit hyperactivity disorder: developmental course and diagnostic value. Psychiatry Res. 2014;216:391–7.
Liechti MD, Valko L, Muller UC, et al. Diagnostic value of resting electroencephalogram in attention-deficit/hyperactivity disorder across the lifespan. Brain Topogr. 2013;26:135–51.
Loo SK, Cho A, Hale TS, McGough J, McCracken J, Smalley SL. Characterization of the theta to beta ratio in ADHD: identifying potential sources of heterogeneity. J Atten Disord. 2013;17:384–92.
Nazari MA, Wallois F, Aarabi A, Berquin P. Dynamic changes in quantitative electroencephalogram during continuous performance test in children with attention-deficit/hyperactivity disorder. Int J Psychophysiol. 2011;81:230–6.
Ogrim G, Kropotov J, Hestad K. The quantitative EEG theta/beta ratio in attention deficit/hyperactivity disorder and normal controls: sensitivity, specificity, and behavioral correlates. Psychiatry Res. 2012;198:482–8.
van Dongen-Boomsma M, Lansbergen MM, Bekker EM, Sandra Kooij JJ, van der Molen M, Kenemans JL, et al. Relation between resting EEG to cognitive performance and clinical symptoms in adults with attention-deficit/hyperactivity disorder. Neurosci Lett. 2010;469:102–6.
Williams LM, Hermens DF, Thein T, Clark CR, Cooper NJ, Clarke SD, et al. Using brain-based cognitive measures to support clinical decisions in ADHD. Pediatr Neurol. 2010;42:118–26.
Arns M, Conners CK, Kraemer HC. A decade of EEG theta/beta ratio research in ADHD: a meta-analysis. J Atten Disord. 2013;17:374–83.
Banaschewski T, Brandeis D, Heinrich H, Albrecht B, Brunner E, Rothenberger A. Association of ADHD and conduct disorder–brain electrical evidence for the existence of a distinct subtype. J Child Psychol Psychiatry Allied Discip. 2003;44(3):356–76.
Banaschewski T, Brandeis D, Heinrich H, Albrecht B, Brunner E, Rothenberger A. Questioning inhibitory control as the specific deficit of ADHD—evidence from brain electrical activity. J Neural Transm. 2004;111(7):841–64. https://doi.org/10.1007/s00702-003-0040-8.
Valko L, Doehnert M, Muller UC, Schneider G, Albrecht B, Drechsler R, et al. Differences in neurophysiological markers of inhibitory and temporal processing deficits in children and adults with ADHD. J Psychophysiol. 2009;23(4):235–46. https://doi.org/10.1027/0269-8803.23.4.235.
van Leeuwen TH, Steinhausen HC, Overtoom CC, Pascual-Marqui RD, van’t Klooster B, Rothenberger A, et al. The continuous performance test revisited with neuroelectric mapping: impaired orienting in children with attention deficits. Behav Brain Res. 1998;94(1):97–110.
Fallgatter AJ, Ehlis AC, Rosler M, Strik WK, Blocher D, Herrmann MJ. Diminished prefrontal brain function in adults with psychopathology in childhood related to attention deficit hyperactivity disorder. Psychiatry Res. 2005;138(2):157–69. https://doi.org/10.1016/j.pscychresns.2004.12.002.
Mueller A, Candrian G, Grane VA, Kropotov JD, Ponomarev VA, Baschera GM. Discriminating between ADHD adults and controls using independent ERP components and a support vector machine: a validation study. Nonlinear Biomed Phys. 2011;5:5. https://doi.org/10.1186/1753-4631-5-5.
Liechti MD, Maurizio S, Heinrich H, Jäncke L, Meier L, Steinhausen HC, et al. First clinical trial of tomographic neurofeedback in attention-deficit/hyperactivity disorder: evaluation of voluntary cortical control. Clin Neurophysiol. 2012;123(10):1989–2005. https://doi.org/10.1016/j.clinph.2012.03.016.
Thapar A, Cooper M, Eyre O, Langley K. What have we learnt about the causes of ADHD? J Child Psychol Psychiatry. 2013;54:3–16. https://doi.org/10.1111/j.1469-7610.2012.02611.x.
Hawi Z, Cummins TD, Tong J, Johnson B, Lau R, Samarrai W, et al. The molecular genetic architecture of attention deficit hyperactivity disorder. Mol Psychiatry. 2015;20:289–97. https://doi.org/10.1038/mp.2014.183.
Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136:215–33. https://doi.org/10.1016/j.cell.2009.01.002.
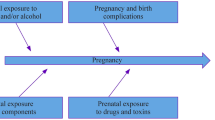
Mill J, Petronis A. Pre- and peri-natal environmental risks for attention-deficit hyperactivity disorder (ADHD): the potential role of epigenetic processes in mediating susceptibility. J Child Psychol Psychiatry. 2008;49:1020–30. https://doi.org/10.1111/j.1469-7610.2008.01909.x.
Schuch V, Utsumi DA, Costa TV, Kulikowski LD, Muszkat M. Attention deficit hyperactivity disorder in the light of the epigenetic paradigm. Front Psychiatry. 2015;6:126. https://doi.org/10.3389/fpsyt.2015.00126.
Kosik KS. The neuronal microRNA system. Nat Rev Neurosci. 2006;7:911–20. https://doi.org/10.1038/nrn2037.
Miller BH, Wahlestedt C. MicroRNA dysregulation in psychiatric disease. Brain Res. 2010;1338:89–99. https://doi.org/10.1016/j.brainres.2010.03.035.
Geaghan M, Cairns MJ. MicroRNA and posttranscriptional dysregulation in psychiatry. Biol Psychiatry. 2015;78:231–9. https://doi.org/10.1016/j.biopsych.2014.12.009.
Issler O, Chen A. Determining the role of microRNAs in psychiatric disorders. Nat Rev Neurosci. 2015;16:201–12. https://doi.org/10.1038/nrn3879.
• Wu L, Zhao Q, Zhu X, Peng M, Jia C, Wu W, et al. A novel function of microRNA let-7d in regulation of galectin-3 expression in attention deficit hyperactivity disorder rat brain. Brain Pathol. 2010;20:1042–54. https://doi.org/10.1111/j.1750-3639.2010.00410.xThis study reported that Rno-let-7d was increased in animal models of ADHD also regulated galectin-3.
Hong Q, Yang L, Zhang M, Pan XQ, Guo M, Fei L, et al. Increased locomotor activity and non-selective attention and impaired learning ability in SD rats after lentiviral vector-mediated RNA interference of Homer 1a in the brain. Int J Med Sci. 2013;10:90–102. https://doi.org/10.7150/ijms.4892.
Yang L, Hong Q, Zhang M, Liu X, Pan XQ, Guo M, et al. The role of Homer 1a in increasing locomotor activity and non-selective attention, and impairing learning and memory abilities. Brain Res. 2013;1515:39–47. https://doi.org/10.1016/j.brainres.2013.03.030.
Pietrzykowski AZ, Spijker S. Impulsivity and comorbid traits: a multi-step approach for finding putative responsible microRNAs in the amygdala. Front Neurosci. 2014;8:389. https://doi.org/10.3389/fnins.2014.00389.
Wu LH, Cheng W, Yu M, He BM, Sun H, Chen Q, et al. Nr3C1-Bhlhb2 axis dysregulation is involved in the development of attention deficit hyperactivity. Mol Neurobiol. 2017;54:1196–212. https://doi.org/10.1007/s12035-015-9679-z.
Kandemir H, Erdal ME, Selek S, Ay ÖI, Karababa IF, Kandemir SB, et al. Evaluation of several micro RNA (miRNA) levels in children and adolescents with attention deficit hyperactivity disorder. Neurosci Lett. 2014;580:158–62. https://doi.org/10.1016/j.neulet.2014.07.060.
Wu LH, Peng M, Yu M, Zhao QL, Li C, Jin YT, et al. Circulating microRNA let-7d in attention-deficit/hyperactivity disorder. NeuroMolecular Med. 2015;17:137–46. https://doi.org/10.1007/s12017-015-8345-y.
Wu L, Zhao Q, Zhu X, Peng M, Jia C, Wu W, et al. A novel function of microRNA let-7d in regulation of galectin-3 expression in attention deficit hyperactivity disorder rat brain. Brain Pathol. 2010;20(6):1042–54.
•• Wang L-J, Li S-C, Lee M-J, Chou M-C, Chou W-J, Lee S-Y, et al. Blood-bourne microRNA biomarker evaluation in attention-deficit/hyperactivity disorder of Han Chinese individuals: an exploratory study. Front Psychiatry. 2018;9:227. https://doi.org/10.3389/fpsyt.2018.00227This study identified 13 miRNAs as potential ADHD biomarkers that would aid in the diagnosis of ADHD.
Cortese S. The neurobiology and genetics of attention-deficit/ hyperactivity disorder (ADHD): what every clinician should know. Eur J Paediatr Neurol. 2012;16(5):422–33.
Friedel S, Saar K, Sauer S, Dempfle A, Walitza S, Renner T, et al. Association and linkage of allelic variants of the dopamine transporter gene in ADHD. Mol Psychiatry. 2007;12(10):923–33.
Gizer IR, Ficks C, Waldman ID. Candidate gene studies of ADHD: a meta-analytic review. Hum Genet. 2009;126(1):51–90.
Franke B, Faraone SV, Asherson P, Buitelaar J, Bau CHD, Ramos-Quiroga JA, et al. The genetics of attention deficit/hyperactivity disorder in adults, a review. Mol Psychiatry. 2012;17(10):960–87.
Kebir O, Joober R. Neuropsychological endophenotypes in attention-deficit/hyperactivity disorder: a review of genetic association studies. Eur Arch Psychiatry Clin Neurosci. 2011;261(8):583–94.
Barnes JJM, Dean AJ, Nandam LS, O’Connell RG, Bellgrove MA. The molecular genetics of executive function: role of monoamine system genes. Biol Psychiatry. 2011;69(12):E127–43.
McGough JJ. Attention deficit hyperactivity disorder pharmacogenetics: the dopamine transporter and D4 receptor. Pharmacogenomics. 2012;13(4):365–8.
Bruxel EM, Akutagava-Martins GC, Salatino-Oliveira A, Contini V, Kieling C, Hutz MH, et al. ADHD pharmacogenetics across the life cycle: new findings and perspectives. Am J Med Genet B Neuropsychiatr Genet. 2014;165:263–82.
Kambeitz J, Romanos M, Ettinger U. Meta-analysis of the association between dopamine transporter genotype and response to methylphenidate treatment in ADHD. Pharm J. 2014;14(1):77–84.
Konrad K, Dempfle A, Friedel S, Heiser P, Holtkamp K, Walitza S, et al. Familiality and molecular genetics of attention networks in ADHD. Am J Med Genet B Neuropsychiatr Genet. 2010;153B(1):148–58.
Shang CY, Gau SSF. Association between the DAT1 gene and spatial working memory in attention deficit hyperactivity disorder. Int J Neuropsychopharmacol. 2014;17(1):9–21.
Noaín D, Avale ME, Wedemeyer C, Calvo D, Peper M, Rubinstein M. Identification of brain neurons expressing the dopamine D4 receptor gene using BAC transgenic mice. Eur J Neurosci. 2006;24(9):2429–38.
Taurines R, Grunblatt E, Schecklmann M, Schwenck C, Albantakis L, Reefschlager L, et al. Altered mRNA expression of monoaminergic candidate genes in the blood of children with attention deficit hyperactivity disorder and autism spectrum disorder. World J Biol Psychiatry. 2011;12:104–8.
Wu J, Xiao HF, Sun HJ, Zou L, Zhu LQ. Role of dopamine receptors in ADHD: a systematic meta-analysis. Mol Neurobiol. 2012;45(3):605–20.
Kebir O, Joober R. Neuropsychological endophenotypes in attention-deficit/hyperactivity disorder: a review of genetic association studies. Eur Arch Psychiatry Clin Neurosci. 2011;261(8):583–94.
Barnes JJM, Dean AJ, Nandam LS, O’Connell RG, Bellgrove MA. The molecular genetics of executive function: role of monoamine system genes. Biol Psychiatry. 2011;69(12):E127–43.
Usiello A, Baik JH, Rouge-Pont F, Picetti R, Dierich A, LeMeur M, et al. Distinct functions of the two isoforms of dopamine D2 receptors. Nature. 2000;408(6809):199–203.
Lasky-Su J, Neale BM, Franke B, Anney RJL, Zhou KX, Maller JB, et al. Genome-wide association scan of quantitative traits for attention deficit hyperactivity disorder identifies novel associations and confirms candidate gene associations. Am J Med Genet B. 2008;147B(8):1345–54.
Winsberg BG, Comings DE. Association of the dopamine transporter gene (DAT1) with poor methylphenidate response. J Am Acad Child Adolesc Psychiatry. 1999;38(12):1474–7.
Beischlag TV, Marchese A, Meador-Woodruff JH, Damask SP, O’Dowd BF, Tyndale RF, et al. The human dopamine D5 receptor gene: cloning and characterization of the 5′-flanking and promoter region. Biochemistry. 1995;34(17):5960–70.
Manor I, Corbex M, Eisenberg J, Gritsenkso I, Bachner-Melman R, Tyano S, et al. Association of the dopamine D5 receptor with attention deficit hyperactivity disorder (ADHD) and scores on a continuous performance test (TOVA). Am J Med Genet B. 2004;127B(1):73–7.
Froehlich TE, McGough JJ, Stein MA. Progress and promise of attention-deficit hyperactivity disorder pharmacogenetics. CNS Drugs. 2010;24(2):99–117.
Stahl SM. Neurotransmission of cognition, part 3. Mechanism of action of selective NRIs: both dopamine and norepinephrine increase in prefrontal cortex. J Clin Psychiatry. 2003;64(3):230–1.
Lasky-Su J, Neale BM, Franke B, Anney RJL, Zhou KX, Maller JB, et al. Genome-wide association scan of quantitative traits for attention deficit hyperactivity disorder identifies novel associations and confirms candidate gene associations. Am J Med Genet B. 2008;147B(8):1345–54.
Mick E, Neale B, Middleton FA, McGough JJ, Faraone SV. Genome-wide association study of response to methylphenidate in 187 children with attention-deficit/hyperactivity disorder. Am J Med Genet B. 2008;147B(8):1412–8.
Yang L, Qian Q, Liu L, Li H, Faraone SV, Wang Y. Adrenergic neurotransmitter system transporter and receptor genes associated with atomoxetine response in attention-deficit hyperactivity disorder children. J Neural Transm. 2013;120(7):1127–33.
Meng WD, Sun SJ, Yang J, Chu RX, Tu W, Liu Q. Elevated serum brain-derived neurotrophic factor (BDNF) but not BDNF gene Val66Met polymorphism is associated with autism spectrum disorders. Mol Neurobiol. 2016;54:1167–72. https://doi.org/10.1007/s12035-016-9721-9.
de Azevedo CT, Mondin TC, Wiener CD, Marques MB, Fucolo Bde A, Pinheiro RT, et al. Neurotrophic factors, clinical features and gender differences in depression. Neurochem Res. 2014;39:1571–8.
Domingos da Silveira da Luz AC, Pereira Dias G, do Nascimento Bevilaqua MC, Cocks G, Gardino PF, Thuret S, et al. Translational findings on brain-derived neurotrophic factor and anxiety: contributions from basic research to clinical practice. Neuropsychobiology. 2013;68:129–38.
Kotyuk E, Keszler G, Nemeth N, Ronai Z, Sasvari-Szekely M, Szekely A. Glial cell line-derived neurotrophic factor (GDNF) as a novel candidate gene of anxiety. PLoS One. 2013;8:e80613.
Vargas HE, Gama CS, Andreazza AC, Medeiros D, Stertz L, Fries G, et al. Decreased serum neurotrophin 3 in chronically medicated schizophrenic males. Neurosci Lett. 2008;440:197–201.
Walz JC, Andreazza AC, Frey BN, Cacilhas AA, Cereser KM, Cunha AB, et al. Serum neurotrophin-3 is increased duringmanic and depressive episodes in bipolar disorder. Neurosci Lett. 2007;415:87–9.
Wysokinski A. Serum levels of brain-derived neurotrophic factor (BDNF) and neurotrophin-3 (NT-3) in depressed patients with schizophrenia. Nord J Psychiatry. 2016;70:267–71.
Bergman O, Westberg L, Lichtenstein P, Eriksson E, Larsson H. Study on the possible association of brain-derived neurotrophic factor polymorphism with the developmental course of symptoms of attention deficit and hyperactivity. Int J Neuropsychopharmacol. 2011;14:1367–76.
Shim SH, Hwangbo Y, Kwon YJ, Jeong HY, Lee BH, Lee HJ, et al. Increased levels of plasma brain-derived neurotrophic factor (BDNF) in children with attention deficit-hyperactivity disorder (ADHD). Prog Neuro-Psychopharmacol Biol Psychiatry. 2008;32:1824–8.
Li H, Liu L, Tang Y, Ji N, Yang L, Qian Q, et al. Sex-specific association of brain-derived neurotrophic factor (BDNF) Val66Met polymorphism and plasma BDNF with attention-deficit/ hyperactivity disorder in a drug-naive Han Chinese sample. Psychiatry Res. 2014;217:191–7.
Amiri A, Torabi Parizi G, Kousha M, Saadat F, Modabbernia MJ, Najafi K, et al. Changes in plasma brain-derived neurotrophic factor (BDNF) levels induced by methylphenidate in children with attention deficit-hyperactivity disorder (ADHD). Prog Neuro-Psychopharmacol Biol Psychiatry. 2013;47:20–4.
Ramos-Quiroga JA, Corominas-Roso M, Palomar G, Gomez-Barros N, Ribases M, Sanchez-Mora C, et al. Changes in the serum levels of brain-derived neurotrophic factor in adults with attention deficit hyperactivity disorder after treatment with atomoxetine. Psychopharmacology. 2014;231:1389–95.
Rios M, Fan G, Fekete C, Kelly J, Bates B, Kuehn R, et al. Conditional deletion of brain-derived neurotrophic factor in the postnatal brain leads to obesity and hyperactivity. Mol Endocrinol. 2001;15:1748–57.
Chourbaji S, Hellweg R, Brandis D, Zorner B, Zacher C, Lang UE, et al. Mice with reduced brain-derived neurotrophic factor expression show decreased choline acetyltransferase activity, but regular brain monoamine levels and unaltered emotional behavior. Brain Res Mol Brain Res. 2004;121:28–36.
Scassellati C, Zanardini R, Tiberti A, Pezzani M, Valenti V, Effedri P, et al. Serum brain-derived neurotrophic factor (BDNF) levels in attention deficit-hyperactivity disorder(ADHD). Eur Child Adolesc Psychiatry. 2014;23:173–7.
Tzang RF, Hsu CD, Liou YJ, Hong CJ, Tsai SJ. Family based association of the brain-derived neurotrophic factor gene in attention-deficit hyperactivity disorder. Psychiatr Genet. 2013;23(4):177–8.
Naumenko VS, Bazovkina DV, Semenova AA, Tsybko AS, Il’chibaeva TV, Kondaurova EM, et al. Effect of glial cell line-derived neurotrophic factor on behavior and key members of the brain serotonin system in mouse strains genetically predisposed to behavioral disorders. J Neurosci Res. 2013;91:1628–38.
Gerlai R, McNamara A, Choi-Lundberg DL, Armanini M, Ross J, Powell-Braxton L, et al. Impaired water maze learning performance without altered dopaminergic function in mice heterozygous for the GDNF mutation. Eur J Neurosci. 2001;14:1153–63.
•• Shim SH, Hwangbo Y, Yoon HJ, Kwon YJ, Lee HY, Hwang JA, et al. Increased levels of plasma glial-derived neurotrophic factor in children with attention deficit hyperactivity disorder. Nord J Psychiatry. 2015;69:546–51 This study was conducted on 86 drug naïve pediatric patients with ADHD which showed increased levels of plasma GDNF levels. The plasma GDNF levels showed a positive correlation with inattention and hyperactivity-impulsivity.
Aloe L, Rocco ML, Bianchi P, Manni L. Nerve growth factor: from the early discoveries to the potential clinical use. J Transl Med. 2012;10:239.
Sarter M, Gehring WJ, Kozak R. More attention must be paid: the neurobiology of attentional effort. Brain Res Rev. 2006;51:145–60.
Syed Z, Dudbridge F, Kent L. An investigation of the neurotrophic factor genes GDNF, NGF, and NT3 in susceptibility to ADHD. Am J Med Genet B Neuropsychiatr Genet. 2007;144B:375–8.
Maness LM, Kastin AJ, Weber JT, Banks WA, Beckman BS, Zadina JE. The neurotrophins and their receptors: structure, function, and neuropathology. Neurosci Biobehav Rev. 1994;18:143–59.
• Park S, Kim BN, Kim JW, Shin MS, Cho SC, Kim JH, et al. Neurotrophin 3 genotype and emotional adverse effects of osmotic-release oral system methylphenidate (OROS-MPH) in children with attention-deficit/hyperactivity disorder. J Psychopharmacol. 2014;28:220–6 This study provided evidence that genetic variation of the NTF3 gene was related to susceptibility of emotional side effects in response to treatment with methylphenidate.
Bilgiç A, Toker A, Işık Ü, Kılınç İ. Serum brain-derived neurotrophic factor, glial-derived neurotrophic factor, nerve growth factor, and neurotrophin-3 levels in children with attention deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry. 2017;26(3):355–63. https://doi.org/10.1007/s00787-016-0898-2.
Oades RD. Role of the serotonin system in ADHD: treatment implications. Expert Rev Neurother. 2007;7(10):1357–74.
Oades RD. Dopamine–serotonin interactions in attention-deficit hyperactivity disorder (ADHD). Prog Brain Res. 2008;172:543–65.
Ludolph AG, Kassubek J, Schmeck K, Glaser C, Wunderlich A, Buck AK, et al. Dopaminergic dysfunction in attention deficit hyperactivity disorder (ADHD), differences between pharmacologically treated and never treated young adults: a 3,4-dihdroxy-6 [18F]fluorophenyl-l-alanine PET study. Neuroimage. 2008;41(3):718–27.
Seo D, Patrick CJ, Kennealy PJ. Role of serotonin and dopamine system interactions in the neurobiology of impulsive aggression and its comorbidity with other clinical disorders. Aggress Violent Behav. 2008;13(5):383–95.
Nordquist N, Creland L. Serotonin, genetic variability, behavioral, and psychiatric disorders-a review. Ups J Med Sci. 2010;115(1):2–10.
Arnsten AF. Catecholamine influences on dorsolateral prefrontal cortical networks. Biol Psychiatry. 2011;69(12):89–99.
Volkow ND, Wang GJ, Kollins SH, Wigal TL, Newcorn JH, Telang F, et al. Evaluating dopamine reward pathway in ADHD: clinical implications. JAMA. 2009;302(10):1084–91.
Volkow ND, Wang GJ, Newcorn J, Telang F, Solanto MV, Fowler JS, et al. Depressed dopamine activity in caudate and preliminary evidence of limbic involvement in adults with attention deficit/hyperactivity disorder. Arch Gen Psychiatry. 2007;64(8):932–40.
Pliska SR, McCracken JT, Maas JW. Catecholamines in attention-deficit hyperactivity disorder: current perspective. J Am Acad Child Adolesc Psychiatry. 1996;35:264–72.
Ernst M, Zametkin AJ, Matochik JA, Jons PH, Cohen RM. Dopa decarboxilase activity in attention deficit hyperactivity disorders adults. A [fluorine-18] flouradopa positron emission tomography study. J Neurosci. 1998;18(15):5901–7.
Zametkin AJ, Ernst M. Current concepts: problems in the management and treatment of attention deficit hyperactivity disorder. N Engl J Med. 1999;340(1):40–8.
Courvoisie H. Neurometabolic functioning and neuropsychological correlates in children with ADHD-H: preliminary findings. J Neuropsychiatr Clin Neurosci. 2004;16:63–9.
Hoshino Y, Ohno Y, Yamamoto T, Kaneko M, Kumashiro H. Plasma free tryptophan concentration in children with attention deficit disorder. Folia Psychiatr Neurol Jpn. 1985;39(4):531–5.
•• Dolina S, Margalit D, Malitsky S, Rabinkov A. Attention-deficit hyperactivity disorder (ADHD) as a pyridoxine-dependent condition: urinary diagnostic biomarkers. Med Hypotheses. 2014;82(1):111–6. https://doi.org/10.1016/j.mehy.2013.11.018This study reported ratios of levels of certain enzymes to be biomarkers of ADHD and reported low concentrations of monoamines and disordered amino acid metabolism to be an inherent cause of ADHD.
Anand D, Colpo GD, Zeni G, Zeni CP, Teixeira AL. Attention- deficit/hyperactivity disorder and inflammation: What does current knowledge tell us? A systematic review. Front Psychiatry. 2017;8:228.
Oades RD, Dauvermann MR, Schimmelmann BG, Schwarz MJ, Myint AM. Attention-deficit hyperactivity disorder (ADHD) and glial integrity: S100B, cytokines and kynurenine metabolism effects of medication. Behav Brain Funct. 2010;6:29.
Oades RD, Myint AM, Dauvermann MR, Schimmelmann BG, Schwarz MJ. Attention-deficit hyperactivity disorder (ADHD) and glial integrity: an exploration of associations of cytokines and kynurenine metabolites with symptoms and attention. Behav Brain Funct. 2010;6:32.
Avcil S. Evaluation of the neutrophil/lymphocyte ratio, platelet/lymphocyte ratio, and mean platelet volume as inflammatory markers in children with attention-deficit hyperactivity disorder. Psychiatry Clin Neurosci. 2018;72(7):522–30. https://doi.org/10.1111/pcn.12659.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on ADHD
Rights and permissions
About this article
Cite this article
Mehta, T., Mannem, N., Yarasi, N.K. et al. Biomarkers for ADHD: the Present and Future Directions. Curr Dev Disord Rep 7, 85–92 (2020). https://doi.org/10.1007/s40474-020-00196-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40474-020-00196-9