Abstract
Purpose of Review
An inefficient living donor candidate evaluation process can be a barrier to timely living donor transplantation and optimal donor satisfaction. In this review, we examine the inefficiencies of the living kidney donor evaluation and make recommendations to optimize this process.
Recent Findings
There is increasing awareness that the living donor evaluation process is inefficient, but little research has been done to date. The time to complete the evaluation can be several or even many months. Avoidable delays can lead to dialysis initiation for pre-emptive transplant candidates, lengthen dialysis time for those patients on dialysis, and reduce donor satisfaction. Opportunities to improve efficiency include the choice, timing, sequencing of evaluation tests, procedures and consults, use of navigators, and monitoring of evaluation timeliness as a quality metric.
Summary
A more efficient evaluation is expected to result in better health outcomes for patients with kidney failure and incur substantial cost savings to the healthcare system.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance ••Of major importance
Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LYC, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341(23):1725–30. https://doi.org/10.1056/NEJM199912023412303.
Rabbat CG, Thorpe KE, Russell JD, Churchill DN. Comparison of mortality risk for dialysis patients and cadaveric first renal transplant recipients in Ontario, Canada. J Am Soc Nephrol. 2000;11(5):917–22.
Ozcan H, Yucel A, Avşar UZ, et al. Kidney transplantation is superior to hemodialysis and peritoneal dialysis in terms of cognitive function, anxiety, and depression symptoms in chronic kidney disease. Transplant Proc. 2015;47(5):1348–51.
Whiting JF, Kiberd B, Kalo Z, Keown P, Roels L, Kjerulf M. Cost-effectiveness of organ donation: evaluating investment into donor action and other donor initiatives. Am J Transplant. 2004;4(4):569–73. https://doi.org/10.1111/j.1600-6143.2004.00373.x.
Tonelli M, Wiebe N, Knoll G, et al. Systematic review: kidney transplantation compared with dialysis in clinically relevant outcomes. Am J Transplant. 2011;11(10):2093–109.
Smith CR, Woodward RS, Cohen DS, et al. Cadaveric versus living donor kidney transplantation: a Medicare payment analysis. Transplantation. 2000;69(2):311–4. https://doi.org/10.1097/00007890-200001270-00020.
Nemati E, Einollahi B, Lesan Pezeshki M, Porfarziani V, Fattahi MR. Does kidney transplantation with deceased or living donor affect graft survival? Nephrourol Mon. 2014;6(4):e12182.
Moist LM, Fenton S, Kim JS, Gill JS, Ivis F, de Sa E, et al. Canadian organ replacement register (CORR): reflecting the past and embracing the future. Can J kidney Health Dis. 2014;1:26. https://doi.org/10.1186/s40697-014-0026-5.
Rodrigue JR, Schold JD, Mandelbrot DA. The decline in living kidney donation in the United States: random variation or cause for concern? Transplantation. 2013;96(9):767–73. https://doi.org/10.1097/TP.0b013e318298fa61.
Horvat LD, Shariff SZ, Garg AX. Global trends in the rates of living kidney donation. Kidney Int. 2009;75(10):1088–98. https://doi.org/10.1038/ki.2009.20.
U.S. Renal Data System. USRDS 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States Natl Institutes Heal Natl Inst Diabetes Dig Kidney Dis 2013.
Reese PP, Boudville N, Garg AX. Living kidney donation: outcomes, ethics, and uncertainty. Lancet. 2015;385(9981):2003–13. https://doi.org/10.1016/S0140-6736(14)62484-3.
Getchell LE, McKenzie SQ, Sontrop JM, Hayward JS, McCallum MK, Garg AX. Increasing the rate of living donor kidney transplantation in Ontario: donor- and recipient-identified barriers and solutions. Can J kidney Health Dis. 2017;4:205435811769866. https://doi.org/10.1177/2054358117698666.
•• Graham JM, Courtney AE. The adoption of a one-day donor assessment model in a living kidney donor transplant program: a quality improvement project. Am J Kidney Dis November. 2017. https://doi.org/10.1053/j.ajkd.2017.07.013. This study reports on a quality improvement project to complete the living kidney donor evaluation in 1 day.
•• Habbous S, Arnold J, Begen MA, et al. Duration of living kidney transplant donor evaluations: findings from 2 multi-center cohort studies. Am J Kidney Dis. 2018:(Accepted, Jan 11, 2018). This study reports the time to complete various steps in the living donor evaluation across multiple transplant centers.
Sanner MA. The donation process of living kidney donors. Nephrol Dial Transplant. 2005;20(8):1707–13. https://doi.org/10.1093/ndt/gfh861.
Living Donor Kidney Transplantation 2020: A UK strategy. NHS. odt.nhs.uk/pdf/ldkt_2020_strategy.pdf. Accessed 30 Nov 2017.
Thiessen C, Kulkarni S, Reese PP, Gordon EJ. A call for research on individuals who opt out of living kidney donation: challenges and opportunities. Transplantation. 2016;100(12):2527–32. https://doi.org/10.1097/TP.0000000000001408.
Moore DR, Feurer ID, Zaydfudim V, Hoy H, Zavala EY, Shaffer D, et al. Evaluation of living kidney donors: variables that affect donation. Prog Transplant. 2012;22(4):385–92. https://doi.org/10.7182/pit2012570.
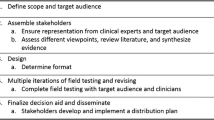
Moore DR, Serur D, Rudow DL, Rodrigue JR, Hays R, Cooper M. Living donor kidney transplantation: improving efficiencies in live kidney donor evaluation-recommendations from a consensus conference. Clin J Am Soc Nephrol. 2015;10(9):1678–86. https://doi.org/10.2215/CJN.01040115.
LaPointe Rudow D, Hays R, Baliga P, et al. Consensus conference on best practices in live kidney donation: recommendations to optimize education, access, and care. Am J Transplant. 2015;15(4):914–22.
• Lentine KL, Kasiske BL, Levey AS, et al. KDIGO clinical practice guideline on the evaluation and care of living kidney donors. Transplantation. 2017;101(8S Suppl 1):S7–S105. This is a set of evidence-based and expert-driven guidelines on living donor evaluations.
Spital A, Taylor JS. Primum non Nocere and living organ donation: a response to Dr. Klintmalm. Am J Transplant. 2008;8(6):1352–3. https://doi.org/10.1111/j.1600-6143.2008.02238.x.
Wright L, Faith K, Richardson R, Grant D. Ethical guidelines for the evaluation of living organ donors. Can J Surg. 2004;47(6):408–13.
Lapasia JB, Kong S, Busque S, Scandling JD, Chertow GM, Tan JC. Living donor evaluation and exclusion: the Stanford experience. Clin Transpl. 2011;25(5):697–704. https://doi.org/10.1111/j.1399-0012.2010.01336.x.
Perlis N, Connelly M, D’A Honey JR, Pace KT, Stewart R. Evaluating potential live-renal donors: causes for rejection, deferral and planned procedure type, a single-centre experience. Can Urol Assoc J. 2013;7(1–2):41–5. https://doi.org/10.5489/cuaj.216.
Taylor LA, Bahreman N, Hayat MJ, Hoey F, Rajasekaran G, Segev DL. Living kidney donors and their family caregivers: developing an evidence-based educational and social support website. Prog Transplant. 2012;22(2):119–28. https://doi.org/10.7182/pit2012611.
Moore DR, Feurer ID, Zavala EY, Shaffer D, Karp S, Hoy H, et al. A web-based application for initial screening of living kidney donors: development, implementation and evaluation. Am J Transplant. 2013;13(2):450–7. https://doi.org/10.1111/j.1600-6143.2012.04340.x.
Richardson R, Connelly M, Dipchand C, Garg AX, Ghanekar A, Houde I, et al. Kidney paired donation protocol for participating donors 2014. Transplantation. 2015;99(10 Suppl 1):S1–S88. https://doi.org/10.1097/TP.0000000000000918.
Tierney J, Shaffer D. Transplantation of ABO A2 kidneys into O recipients: do IgM anti-A1 titers matter? Clin Transpl. 2015;29(4):379–82. https://doi.org/10.1111/ctr.12527.
Crafter SR, Bell L, Foster BJ. Balancing organ quality, HLA-matching, and waiting times: impact of a pediatric priority allocation policy for deceased donor kidneys in Quebec. Transplantation. 2007;83(11):1411–5. https://doi.org/10.1097/01.tp.0000266580.19614.f7.
Mulley WR, Kanellis J. Understanding crossmatch testing in organ transplantation: a case-based guide for the general nephrologist. Nephrology. 2011;16(2):125–33. https://doi.org/10.1111/j.1440-1797.2010.01414.x.
Winters JL, Gloor JM, Pineda AA, Stegall MD, Moore SB. Plasma exchange conditioning for ABO-incompatible renal transplantation. J Clin Apher. 2004;19(2):79–85. https://doi.org/10.1002/jca.20002.
Mierzejewska B, Durlik M, Lisik W, et al. Current approaches in national kidney paired donation programs. Ann Transplant. 2013;18:112–24.
Reikie BA, Kroczak T, McGregor TB. Challenges for the travelling donor: variability between donor workup and donor surgery in the Canadian kidney paired exchange program. Transplant Proc. 2017;49(6):1232–6.
Ashlagi I, Gilchrist DS, Roth AE, Rees MA. Nonsimultaneous chains and dominos in kidney- paired donation-revisited. Am J Transplant. 2011;11(5):984–94. https://doi.org/10.1111/j.1600-6143.2011.03481.x.
Gentry SE, Montgomery RA, Segev DL. Kidney paired donation: fundamentals, limitations, and expansions. Am J Kidney Dis. 2011;57(1):144–51. https://doi.org/10.1053/j.ajkd.2010.10.005.
Bray M, Wang W, Song PX-K, et al. Planning for uncertainty and fallbacks can increase the number of transplants in a kidney-paired donation program. Am J Transplant. 2015;15(10):2636–45.
Ferrari P, Fidler S, Woodroffe C, Tassone G, D’Orsogna L. Comparison of time on the deceased donor kidney waitlist versus time on the kidney paired donation registry in the Australian program. Transpl Int. 2012;25(10):1026–31. https://doi.org/10.1111/j.1432-2277.2012.01541.x.
Allen RDM, Pleass HCC, Woodroffe C, Clayton PA, Ferrari P. Challenges of kidney paired donation transplants involving multiple donor and recipient surgeons across Australia. ANZ J Surg. 2016; https://doi.org/10.1111/ans.13517.
Allen R, Pleass H, Clayton PA, Woodroffe C, Ferrari P. Outcomes of kidney paired donation transplants in relation to shipping and cold ischaemia time. Transpl Int. 2016;29(4):425–31. https://doi.org/10.1111/tri.12719.
Henderson ML, Gross JA. Living organ donation and informed consent in the United States: strategies to improve the process. J Law Med Ethics. 2017;45(1):66–76. https://doi.org/10.1177/1073110517703101.
• Lam NN, Lentine KL, Garg AX. Renal and cardiac assessment of living kidney donor candidates. Nat Rev Nephrol. 2017;13(7):420–8. https://doi.org/10.1038/nrneph.2017.43. This is a review of the renal and cardiac evaluation for living donor candidates, comparing guidelines and suggesting areas for efficiency improvement.
Delanaye P, Schaeffner E, Ebert N, et al. Normal reference values for glomerular filtration rate: what do we really know? Nephrol Dial Transplant. 2012;27(7):2664–72.
Baxter GM. Imaging in renal transplantation. Ultrasound Q. 2003;19(3):123–38.
Cosgrove DO, Chan KE. Renal transplants: what ultrasound can and cannot do. Ultrasound Q. 2008;24(2):77–87. https://doi.org/10.1097/RUQ.0b013e31817c5e46.
Burgos FJ, Pascual J, Marcen R, García-Navas R, Gómez V, Ortuño J. The role of imaging techniques in renal transplantation. World J Urol. 2004;22(5):399–404. https://doi.org/10.1007/s00345-004-0412-1.
el-Diasty TA, Shokeir AA, el-Ghar MEA, Gad HM, Refaie AF, el-Din ABS. Contrast enhanced spiral computerized tomography in live kidney donors: a single session for anatomical and functional assessment. J Urol. 2004;171(1):31–4. https://doi.org/10.1097/01.ju.0000099784.52825.8e.
Kok NFM, Dols LFC, Hunink MGM, Alwayn IPJ, Tran KTC, Weimar W, et al. Complex vascular anatomy in live kidney donation: imaging and consequences for clinical outcome. Transplantation. 2008;85(12):1760–5. https://doi.org/10.1097/TP.0b013e318172802d.
Halleck F, Diederichs G, Koehlitz T, et al. Volume matters: CT-based renal cortex volume measurement in the evaluation of living kidney donors. Transpl Int. 2013;26(12):1208–16.
Herts BR, Sharma N, Lieber M, Freire M, Goldfarb DA, Poggio ED. Estimating glomerular filtration rate in kidney donors: a model constructed with renal volume measurements from donor CT scans. Radiology. 2009;252(1):109–16. https://doi.org/10.1148/radiol.2521081873.
Huang N, Foster MC, Lentine KL, Garg AX, Poggio ED, Kasiske BL, et al. Estimated GFR for living kidney donor evaluation. Am J Transplant. 2016;16(1):171–80. https://doi.org/10.1111/ajt.13540.
Gaillard F, Flamant M, Lemoine S, et al. Estimated or measured GFR in living kidney donors work-up? Am J Transplant. 2016;16(10):3024–32.
Rodrigue JR, Pavlakis M, Danovitch GM, et al. Evaluating living kidney donors: relationship types, psychosocial criteria, and consent processes at US transplant programs. Am J Transplant. 2007;7(10):2326–32.
Sullivan C, Leon JB, Sayre SS, et al. Impact of navigators on completion of steps in the kidney transplant process: a randomized, controlled trial. Clin J Am Soc Nephrol. 2012;7(10):1639–45. https://doi.org/10.2215/CJN.11731111.
Transplant Ambassador Program “brings the patients to the patients.” Can-SOLVE CKD. 2017. https://cansolveckd.ca/2017/09/26/bringing-the-patients-to-the-patients/. Accessed 13 Dec 2017.
Jacobs C, Thomas C. Financial considerations in living organ donation. Prog Transplant. 2003;13(2):130–6. https://doi.org/10.1177/152692480301300210.
Klarenbach S, Gill JS, Knoll G, Caulfield T, Boudville N, Prasad GVR, et al. Economic consequences incurred by living kidney donors: a Canadian multi-center prospective study. Am J Transplant. 2014;14(4):916–22. https://doi.org/10.1111/ajt.12662.
Tushla L, Rudow DL, Milton J, Rodrigue JR, Schold JD, Hays R. Living-donor kidney transplantation: reducing financial barriers to live kidney donation—recommendations from a consensus conference. Clin J Am Soc Nephrol. 2015;10(9):1696–702. https://doi.org/10.2215/CJN.01000115.
Tong A, Chapman JR, Wong G, Craig JC. Perspectives of transplant physicians and surgeons on reimbursement, compensation, and incentives for living kidney donors. Am J Kidney Dis. 2014;64(4):622–32. https://doi.org/10.1053/j.ajkd.2014.02.019.
Hays R, Rodrigue JR, Cohen D, Danovitch G, Matas A, Schold J, et al. Financial neutrality for living organ donors: reasoning, rationale, definitions, and implementation strategies. Am J Transplant. 2016;16(7):1973–81. https://doi.org/10.1111/ajt.13813.
Warren PH, Gifford KA, Hong BA, Merion RM, Ojo AO. Development of the National Living Donor Assistance Center: reducing financial disincentives to living organ donation. Prog Transplant. 2014;24(1):76–81. https://doi.org/10.7182/pit2014593.
Vlaicu S, Klarenbach S, Yang RC, Dempster T, Garg AX. Current Canadian initiatives to reimburse live organ donors for their non-medical expenses. Can J Public Health. 2007;98(6):481–3.
CORR Annual statistics 2017. https://www.cihi.ca/en/corr-annual-statistics-2017. Accessed 17 July 2017.
Hays R, Waterman AD. Improving preemptive transplant education to increase living donation rates: reaching patients earlier in their disease adjustment process. Prog Transplant. 2008;18(4):251–6. https://doi.org/10.1177/152692480801800407.
Jay CL, Dean PG, Helmick RA, Stegall MD. Reassessing preemptive kidney transplantation in the United States: are we making progress? Transplantation. 2016;100(5):1120–7. https://doi.org/10.1097/TP.0000000000000944.
Kurowski A, Sańko-Resmer J, Wyzgał J, Kurowski A. Assessment of health-related quality of life of patients after kidney transplantation in comparison with hemodialysis and peritoneal dialysis. Ann Transplant. 2014;19:576–85.
Haller MC, Kainz A, Baer H, Oberbauer R. Dialysis vintage and outcomes after kidney transplantation: a retrospective cohort study. Clin J Am Soc Nephrol. 2017;12(1):122–30. https://doi.org/10.2215/CJN.04120416.
Okechukwu CN, Lopes AA, Stack AG, Feng S, Wolfe RA, Port FK. Impact of years of dialysis therapy on mortality risk and the characteristics of longer term dialysis survivors. Am J Kidney Dis. 2002;39(3):533–8. https://doi.org/10.1053/ajkd.2002.31403.
•• Habbous S, McArthur E, Begen MA, et al. Initiating maintenance dialysis prior to living kidney donor transplantation when a donor candidate evaluation is well underway. Transplantation. 2017:(accepted Dec 22, 2017). This study reports on the loss of potential preemptive transplants, as up to 1/3 of transplant recipients started dialysis despite having a living donor whose evaluation was at least 3 months underway.
Wish JB. Introduction to quality improvement. Am J Kidney Dis 1998;32(6 Suppl 4):S161–4.
Funding
Steven Habbous is supported by the Canadian Institutes of Health Research Frederick Banting and Charles Best Canada Doctoral Scholarship. Dr. Amit Garg was supported by the Dr. Adam Linton Chair in Kidney Health Analytics and a Clinician Investigator Award from the Canadian Institutes of Health Research. Dr. Ngan N. Lam was supported by a Kidney Research Scientist Core Education and National Training Program (KRESCENT) New Investigator Award. Canadians Seeking Solutions and Innovations to Overcome Chronic Kidney Disease (CAN-SOLVE CKD) is a patient-orientated research network to transform the care of people affected by kidney disease; CAN-SOLVE CKD was integral to highlighting this issue and providing some patient perspective.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Garg received an investigator initiated award from Astellas, in partnership, to support a Canadian Institutes of Health Research grant in living kidney donation.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Live Kidney Donation
Rights and permissions
About this article
Cite this article
Habbous, S., Garg, A.X. & Lam, N.N. Optimizing Efficiency in the Evaluation of Living Donor Candidates: Best Practices and Implications. Curr Transpl Rep 5, 55–63 (2018). https://doi.org/10.1007/s40472-018-0184-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-018-0184-y