Abstract
Treatment options for hepatocellular carcinoma (HCC) have changed significantly, beginning in 1994 with the establishment of successful long-term outcomes for HCC patients within Milan criteria who went on to receive liver transplantation (LT). Improved outcomes for patients with HCC undergoing LT led to challenges in determining the optimal liver allocation policy, which could provide relatively equal access for patients with and without HCC in the face of a long-standing critical shortage of available donor organs. United Network for Organ Sharing/Organ Procurement Transplantation Network (UNOS/OPTN) policy changes have aimed to optimize data collection for patients transplanted with HCC, improve the diagnostic criteria required for HCC, and reduce the disparity in access to transplantation for HCC and non-HCC patients observed between high- and low-model for end-stage liver disease (MELD) regions. Although current understanding of HCC tumor biology remains suboptimal, continued careful analysis of waitlist and post-transplant outcomes for both HCC and non-HCC patients combined with refinements to the allocation policy will hopefully result in improved survival both for waitlisted and post-transplant patients.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •Of importance
Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334(11):693–9.
Pomfret EA, Washburn K, Wald C, Nalesnik MA, Douglas D, Russo M, et al. Report of a national conference on liver allocation in patients with hepatocellular carcinoma in the United States. Liver Transpl. 2010;16(3):262–78. doi:10.1002/lt.21999.
Clavien PA, Lesurtel M, Bossuyt PM, Gores GJ, Langer B, Perrier A, et al. Recommendations for liver transplantation for hepatocellular carcinoma: an international consensus conference report. Lancet Oncol. 2012;13(1):e11–22. This consensus report provides current recommendations for liver transplantation candidacy, tumor downstaging, management of patients on the waiting list, and post-transplant management.
Mazzaferro V, Llovet JM, Miceli R, Bhoori S, Schiavo M, Mariani L, et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. 2009;10(1):35–43.
Ioannou GN, Perkins JD, Carithers Jr RL. Liver transplantation for hepatocellular carcinoma: impact of the MELD allocation system and predictors of survival. Gastroenterology. 2008;134(5):1342–51.
Llovet JM. Evidence-based medicine in the treatment of hepatocellular carcinoma. J Gastroenterol Hepatol. 2002;17 Suppl 3:S428–33. Review.
Yao FY, Xiao L, Bass NM, Kerlan R, Ascher NL, Roberts JP. Liver transplantation for hepatocellular carcinoma: validation of the UCSF-expanded criteria based on preoperative imaging. Am J Transplant. 2007;7(11):2587–96.
Organ Procurement and Transplantation Network. Policy 9.3.F.iv imaging requirements for class 5 lesions Effective 3/1/2016 https://optn.transplant.hrsa.gov/media/1200/optn_policies.pdf.
Mehta N, Sarkar M, Dodge JL, Fidelman N, Roberts JP, Yao FY. Intention to treat outcome of T1 hepatocellular carcinoma with the “wait and not ablate” approach until meeting T2 criteria for liver transplant listing. Liver Transpl. 2016;22(2):178–87. This study highlights current understanding of HCC biology and demonstrates the overall low risk of waitlist dropout.
Freeman Jr RB, Wiesner RH, Roberts JP, McDiarmid S, Dykstra DM, Merion RM. Improving liver allocation: MELD and PELD. Am J Transplant. 2004;4 Suppl 9:114–31.
Koteish A, Thuluvath PJ. Screening for hepatocellular carcinoma. J Vasc Interv Radiol. 2002;13(9 Pt 2):S185–90. Review.
Kubota K, Ina H, Okada Y, Irie T. Growth rate of primary single hepatocellular carcinoma: determining optimal screening interval with contrast enhanced computed tomography. Dig Dis Sci. 2003;48(3):581–6.
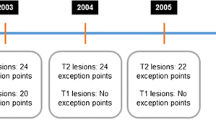
Wald C, Russo MW, Heimbach JK, Hussain HK, Pomfret EA, Bruix J. New OPTN/UNOS policy for liver transplant allocation: standardization of liver imaging, diagnosis, classification, and reporting of hepatocellular carcinoma. Radiology. 2013;266(2):376–82.
Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33(2):464–70.
Wedd JP, Nordstrom E, Nydam T, Durham J, Zimmerman M, Johnson T, et al. Hepatocellular carcinoma in patients listed for liver transplantation: current and future allocation policy and management strategies for the individual patient. Liver Transpl. 2015;21(12):1543–52.
Heimbach JK, Hirose R, Stock PG, Schladt DP, Xiong H, Liu J, et al. Delayed hepatocellular carcinoma model for end-stage liver disease exception score improves disparity in access to liver transplant in the United States. Hepatology. 2015;61(5):1643–50. Current HCC policy changes are based on modeling outcomes proposed by this study. The authors review the current variability in MELD at the time of transplant and suggest a delay in exception points as way to improve the disparity observed between high- and low-MELD regions.
Sharma P, Harper AM, Hernandez JL, Heffron T, Mulligan DC, Wiesner RH, et al. Reduced priority MELD score for hepatocellular carcinoma does not adversely impact candidate survival awaiting liver transplantation. Am J Transplant. 2006;6(8):1957–62.
Wiesner RH, Freeman RB, Mulligan DC. Liver transplantation for hepatocellular cancer: the impact of the MELD allocation policy. Gastroenterology. 2004;127(5 Suppl 1):S261–7.
Washburn K, Edwards E, Harper A, Freeman R. Hepatocellular carcinoma patients are advantaged in the current liver transplant allocation system. Am J Transplant. 2010;10(7):1643–8.
Freeman Jr RB, Steffick DE, Guidinger MK, Farmer DG, Berg CL, Merion RM. Liver and intestine transplantation in the United States, 1997–2006. Am J Transplant. 2008;8(4 Pt 2):958–76.
Terzi E, Ray Kim W, Sanchez W, Charlton MR, Schmeltzer P, Gores GJ, et al. Impact of multiple transarterial chemoembolization treatments on hepatocellular carcinoma for patients awaiting liver transplantation. Liver Transpl. 2015;21(2):248–57.
Ravaioli M, Grazi GL, Piscaglia F, Trevisani F, Cescon M, Ercolani G, et al. Liver transplantation for hepatocellular carcinoma: results of down-staging in patients initially outside the Milan selection criteria. Am J Transplant. 2008;8(12):2547–57.
Yao FY, Kerlan Jr RK, Hirose R, Davern 3rd TJ, Bass NM, Feng S, et al. Excellent outcome following down-staging of hepatocellular carcinoma prior to liver transplantation: an intention-to-treat analysis. Hepatology. 2008;48(3):819–27.
Yao FY, Mehta N, Flemming J, Dodge J, Hameed B, Fix O, et al. Downstaging of hepatocellular cancer before liver transplant: long-term outcome compared to tumors within Milan criteria. Hepatology. 2015;61(6):1968–77.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Julie Heimbach and Caroline Jadlowiec declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Liver Transplantation
Rights and permissions
About this article
Cite this article
Jadlowiec, C.C., Heimbach, J.K. Advances in How We Prioritize Liver Allocation for Hepatocellular Carcinoma in the USA. Curr Transpl Rep 3, 334–340 (2016). https://doi.org/10.1007/s40472-016-0127-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-016-0127-4