Abstract
Purpose of Review
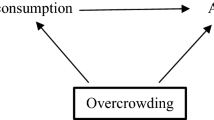
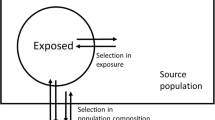
Epidemiologic research is rarely based on a random sample of a well-defined target population. We used causal directed acyclic graphs to demonstrate the types of bias that can result when selection into that sample is associated with the exposure or outcome of interest, or with both. These selection mechanisms can affect both the internal and external validity of a study. We reviewed approaches to selection mechanisms that affect valid causal inference.
Recent Findings
We noted that selection bias can refer to a number of issues with different consequences. We identified strategies for addressing selection bias when designing studies, collecting data, conducting analyses, and assessing possible bias in those analyses.
Summary
Understanding the way in which a study sample relates to the target population is critical for avoiding and addressing bias. Communication about selection bias is aided by the use of causal graphs.



Similar content being viewed by others
Notes
The related problem of transportability refers to the situation in which the study sample is not a subset of the target population [13], but we will not consider this further.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Berkson J. Limitations of the application of fourfold table analysis to hospital data. Biom Bull. 1946;2(3):47–53.
Greenland S. Response and follow-up bias in cohort studies. Am J Epidemiol. 1977;106(3):184–7.
Criqui MH. Response bias and risk ratios in epidemiologic studies. Am J Epidemiol. 1979;109(4):394–9.
Austin MA, Criqui MH, Barrett-connor E, Holdbrook MJ. The effect of response bias on the odds ratio. Am J Epidemiol. 1981;114(1):137–43.
Hernán MA, Hernández-Díaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15(5):615–25.
Didelez V, Kreiner S, Keiding N. Graphical models for inference under outcome-dependent sampling. Stat Sci. 2010;25(3):368–87.
Bareinboim E, Tian J, Pearl J. Recovering from selection bias in causal and statistical inference. In: Proceedings of the Twenty-Eighth AAAI Conference on Artificial Intelligence. 2014. p. 2410–6.
Bareinboim E, Tian J. Recovering causal effects from selection Bias. In: Proceedings of the Twenty-Ninth Conference on Artificial Intelligence. 2015. p. 3475–81.
Correa JD, Tian J, Bareinboim E. Identification of causal effects in the presence of selection bias. Proceedings of the Thirty-Third AAAI Conference on Artificial Intelligence 2019;2744–51.
• Infante-Rivard C, Cusson A. Reflection on modern methods: selection bias—a review of recent developments. Int J Epidemiol. 2018;47(5):1714–22 Translates recent work in algorithms for recoverability under selection for an epidemiology audience.
•• Westreich D, Edwards JK, Lesko CR, Cole SR, Stuart EA. Target validity and the hierarchy of study designs. Am J Epidemiol. 2018;188(2):438–43 Proposes the concept of target validity, which brings together internal and external validity.
Kohler U, Kreuter F, Stuart EA. Nonprobability sampling and causal analysis. Ann Rev Stat Appl. 2019;6(1):149–72.
Lesko CR, Buchanan AL, Westreich D, Edwards JK, Hudgens MG, Cole SR. Generalizing study results. Epidemiology. 2017;28(4):553–61.
Arah OA. Analyzing selection bias for credible causal inference: when in doubt, DAG it out. Epidemiology. 2019;30(4):517–20.
Haneuse S. Distinguishing selection bias and confounding bias in comparative effectiveness research. Med Care. 2016;54(4):e23–9.
•• Mansournia MA, Higgins JPT, Sterne JAC, Hernán MA. Biases in randomized trials: a conversation between trialists and epidemiologists. Epidemiology. 2017;28(1):54–9 Translates bias terminology from and into the world of trials. Regarding selection bias, it is particularly helpful for explaining how bias can occur even under randomization.
Dahabreh IJ, Robins JM, Haneuse SJ-PA, Hernán MA. Generalizing causal inferences from randomized trials: counterfactual and graphical identification [Internet]. 2019. Available from: http://arxiv.org/abs/1906.10792.
•• Schuessler J, Selb P. Graphical causal models for survey inference [Internet]. 2019. Available from: https://osf.io/preprints/socarxiv/hbg3m/. A very clear introduction to directed acyclic graphs, translates concepts in causal inference to survey inference, with extensions including multiple selection nodes.
Hernán MA. Invited commentary: selection bias without colliders. Am J Epidemiol. 2017;185(11):1048–50.
VanderWeele TJ, Robins JM. Directed acyclic graphs, sufficient causes, and the properties of conditioning on a common effect. Am J Epidemiol. 2007;166(9):1096–104.
Greenland S. Quantifying biases in causal models: classical confounding vs collider-stratification bias. Epidemiology. 2003;14(3):300–6.
Jiang Z, Ding P. The directions of selection bias. Stat Probabil Lett. 2017;125:104–9.
Nguyen TQ, Dafoe A, Ogburn EL. The magnitude and direction of collider bias for binary variables. Epidemiol Methods. 2019:1–29.
• Munafò MR, Tilling K, Taylor AE, Evans DM, Davey SG. Collider scope: when selection bias can substantially influence observed associations. Int J Epidemiol. 2018;47(1):226–35 Provides intuitive explanation of collider bias as well as examples of selection bias in genetic studies.
Chaix B, Evans D, Merlo J, Suzuki E. Commentary: weighing up the dead and missing: reflections on inverse-probability weighting and principal stratification to address truncation by death. Epidemiology. 2012;23(1):129–31.
Wei L, Brookhart MA, Schneeweiss S, Mi X, Setoguchi S, Liu W, et al. Implications of M bias in epidemiologic studies: a simulation study. Am J Epidemiol. 2012;176(10):938–48.
Stoner MCD, Cole SR, Price J, Winston J, Stringer JSA. Timing of initiation of antiretroviral therapy and risk of preterm birth in studies of HIV-infected pregnant women. Epidemiology. 2018 Mar;29(2):224–9.
Cole SR, Stuart EA. Generalizing evidence from randomized clinical trials to target populations: the ACTG 320 trial. Am J Epidemiol. 2010;172(1):107–15.
Stuart EA, Cole SR, Bradshaw CP, Leaf PJ. The use of propensity scores to assess the generalizability of results from randomized trials. J R Stat Soc Ser A (Stat Soc). 2011;174(2):369–86.
Nguyen TQ, Ebnesajjad C, Cole SR, Stuart EA. Sensitivity analysis for an unobserved moderator in RCT-to-target-population generalization of treatment effects. Ann Appl Stat. 2017;11(1):225–47.
•• Dahabreh IJ, Robertson SE, Steingrimsson JA, Stuart EA, Hernan MA. Extending inferences from a randomized trial to a new target population [Internet]. 2019. Available from: http://arxiv.org/abs/1805.00550. Very clear tutorial, with code, for generalizing from a trial population using several methods.
• Arnold BF, Ercumen A, Benjamin-Chung J, Colford JMJ. Brief report: Negative controls to detect selection bias and measurement bias in epidemiologic studies. Epidemiology. 2016;27(5):637–41 Provides helpful guidance for using negative control exposures and outcomes, with DAGs and examples from the literature.
Van Gelder MMHJ, Bretveld RW, Roeleveld N. Web-based questionnaires: the future in epidemiology? Am J Epidemiol. 2010;172(11):1292–8.
Christensen T, Riis AH, Hatch EE, Wise LA, Nielsen MG, Rothman KJ, et al. Costs and efficiency of online and offline recruitment methods: a web-based cohort study. J Med Internet Res. 2017;19(3):e58.
Wise LA, Rothman KJ, Mikkelsen EM, Stanford JB, Wesselink AK, McKinnon C, et al. Design and conduct of an internet-based preconception cohort study in North America: pregnancy study online. Paediatr Perinat Epidemiol. 2015;29(4):360–71.
Hatch EE, Hahn KA, Wise LA, Mikkelsen EM, Kumar R, Fox MP, et al. Evaluation of selection bias in an internet-based study of pregnancy planners. Epidemiology. 2016;27(1):98–104.
Jackson ML, Nelson JC. The test-negative design for estimating influenza vaccine effectiveness. Vaccine. 2013;31(17):2165–8.
Sullivan SG, Tchetgen EJT, Cowling BJ. Theoretical basis of the test-negative study design for assessment of influenza vaccine effectiveness. Am J Epidemiol. 2016;184(5):345–53.
Feng S, Cowling BJ, Kelly H, Sullivan SG. Estimating influenza vaccine effectiveness with the test-negative design using alternative control groups: a systematic review and meta-analysis. Am J Epidemiol. 2018;187(2):389–97.
Segaloff HE, Cheng B, Miller A V, Petrie JG, Malosh RE, Cheng C, et al. Influenza vaccine effectiveness in the inpatient setting; evaluation of potential bias in the test negative design by use of alternate control groups. Am J Epidemiol. 2019.
Westreich D, Hudgens MG. Invited commentary: beware the test-negative design. Am J Epidemiol. 2016;184(5):354–6.
Lewnard JA, Tedijanto C, Cowling BJ, Lipsitch M. Measurement of vaccine direct effects under the test-negative design. Am J Epidemiol. 2018;187(12):2686–97.
Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158(9):915–20.
Danaei G, Tavakkoli M, Hernán MA. Bias in observational studies of prevalent users: lessons for comparative effectiveness research from a meta-analysis of statins. Am J Epidemiol. 2012;175(4):250–62.
McCandless LC. Statin use and fracture risk: can we quantify the healthy-user effect? Epidemiology. 2013;24(5):743–52.
Flanders WD, Eldridge RC, McClellan W. A nearly unavoidable mechanism for collider bias with index-event studies. Epidemiology. 2014;25(5):762–4.
Banack HR, Kaufman JS. The “obesity paradox” explained. Epidemiology. 2013;24(3):461–2.
Tchetgen EJT, Glymour MM, Shpitser I, Weuve J. Rejoinder: to weight or not to weight?: on the relation between inverse-probability weighting and principal stratification for truncation by death. Epidemiology. 2012;23(1):132–7.
Shardell M, Hicks GE, Ferrucci L. Doubly robust estimation and causal inference in longitudinal studies with dropout and truncation by death. Biostatistics. 2015;16(1):155–68.
Hernán MA, Schisterman EF, Hernández-Díaz S. Invited commentary: composite outcomes as an attempt to escape from selection bias and related paradoxes. Am J Epidemiol. 2014;179(3):368–70.
Tchetgen Tchetgen EJ, Phiri K, Shapiro R. A simple regression-based approach to account for survival bias in birth outcomes research. Epidemiology. 2015;26(4):473–80.
• Long DL, Howard G, Long DM, Judd S, Manly JJ, McClure LA, et al. An investigation of selection bias in estimating racial disparity in stroke risk factors. Am J Epidemiol. 2019;188(3):587–97 A clear, straightforward application of inverse probability weighting and a survivor average causal effect approach.
•• Young JG, Stensrud MJ, Tchetgen Tchetgen EJ, Hernán MA. A causal framework for classical statistical estimands in failure-time settings with competing events. Stat Med. 2020;39(8):1199–236 A thorough examination of what is implied by various estimands in the face of competing events.
Hernán MA, Sauer BC, Hernández-Díaz S, Platt R, Shrier I. Specifying a target trial prevents immortal time bias and other self-inflicted injuries in observational analyses. J Clin Epidemiol. 2016;79:70–5.
Cain LE, Robins JM, Lanoy E, Logan R, Costagliola D, Hernán MA. When to start treatment? A systematic approach to the comparison of dynamic regimes using observational data. Int J Biostat. 2010;6(2):1–42.
Young JG, Cain LE, Robins JM, O’Reilly EJ, Hernán MA. Comparative effectiveness of dynamic treatment regimes: an application of the parametric g-formula. Stat Biosci. 2011;3(1):119–43.
Little RJA. Regression with missing X’s: a review. J Am Stat Assoc. 1992;87(420):1227–37.
Bartlett JW, Harel O, Carpenter JR. Asymptotically unbiased estimation of exposure odds ratios in complete records logistic regression. Am J Epidemiol. 2014;182(8):730–6.
Moreno-Betancur M, Lee KJ, Leacy FP, White IR, Simpson JA, Carlin JB. Canonical causal diagrams to guide the treatment of missing data in epidemiologic studies. Am J Epidemiol. 2018;187(12):2705–15.
Groenwold RHH, Donders ART, Roes KCB, Harrell FE, Moons KGM. Dealing with missing outcome data in randomized trials and observational studies. Am J Epidemiol. 2012;175(3):210–7.
Harel O, Mitchell EM, Perkins NJ, Cole SR, Tchetgen Tchetgen EJ, Sun B, et al. Multiple imputation for incomplete data in epidemiologic studies. Am J Epidemiol. 2018;187(3):576–84.
Haneuse S, Schildcrout J, Crane P, Sonnen J, Breitner J, Larson E. Adjustment for selection bias in observational studies with application to the analysis of autopsy data. Neuroepidemiology. 2009;32(3):229–39.
Westreich D. Berkson’s bias, selection bias, and missing data. Epidemiology. 2012;23(1):159–64.
Howe CJ, Cain LE, Hogan JW. Are all biases missing data problems? Curr Epidemiol Rep. 2015;2(3):162–71.
Robins JM, Finkelstein DM. Correcting for noncompliance and dependent censoring in an AIDS clinical trial with inverse probability of censoring weighted (IPCW) log-rank tests. Biometrics. 2000;56(3):779–88.
Howe CJ, Cole SR, Lau B, Napravnik S, Eron JJJ. Selection bias due to loss to follow up in cohort studies. Epidemiology. 2016;27(1):91–7.
Modest AM, Wise LA, Fox MP, Weuve J, Penzias AS, Hacker MR. IVF success corrected for drop-out: use of inverse probability weighting. Hum Reprod. 2018;33(12):2295–301.
Banack HR, Harper S, Kaufman JS. Accounting for selection bias in studies of acute cardiac events. Can J Cardiol. 2018;34(6):709–16.
• Jackson JW. Diagnosing covariate balance across levels of right-censoring before and after application of inverse-probability-of-censoring weights. Am J Epidemiol. 2019;188(12):1–9 Method for assessing whether models for selection succeed at balancing measured covariates when used to construct inverse probability weights, with example code.
Haneuse S, Bogart A, Jazic I, Westbrook EO, Boudreau D, Theis MK, et al. Learning about missing data mechanisms in electronic health records-based research: a survey-based approach. Epidemiology. 2016;27(1):82–90.
Sun B, Perkins NJ, Cole SR, Harel O, Mitchell EM, Schisterman EF, et al. Inverse-probability-weighted estimation for monotone and nonmonotone missing data. Am J Epidemiol. 2018;187(3):585–91.
Fox MP, Lash TL. Quantitative bias analysis for study and grant planning. Ann Epidemiol. 2020 Mar;43:32–6.
Geneletti S, Mason A, Best N. Adjusting for selection effects in epidemiologic studies. Epidemiology. 2011;22(1):36–9.
Thompson CA, Arah OA. Selection bias modeling using observed data augmented with imputed record-level probabilities. Ann Epidemiol. 2014;24(10):747–53.
Greenland S. Basic methods for sensitivity analysis of biases. Int J Epidemiol. 1996;25(6):1107–16.
Khoury MJ, Flanders WD, James LM, Erickson JD. Human teratogens, prenatal mortality, and selection bias. Am J Epidemiol. 1989;130(2):361–70.
Patorno E, Huybrechts KF, Bateman BT, Cohen JM, Desai RJ, Mogun H, et al. Lithium use in pregnancy and the risk of cardiac malformations. N Engl J Med. 2017;376(23):2245–54.
Lash TL, Fox MP, MacLehose RF, Maldonado G, McCandless LC, Greenland S. Good practices for quantitative bias analysis. Int J Epidemiol. 2014;43(6):1969–85.
Howards PP, Johnson CY, Honein MA, Flanders WD. Adjusting for bias due to incomplete case ascertainment in case-control studies of birth defects. Am J Epidemiol. 2015;181(8):595–607.
Stensrud MJ, Valberg M, Røysland K, Aalen OO. Exploring selection bias by causal frailty models: the magnitude matters. Epidemiology. 2017;28(3):379–86.
Shardell M, Scharfstein DO, Vlahov D, Galai N. Sensitivity analysis using elicited expert information for inference with coarsened data: illustration of censored discrete event times in the AIDS Link to Intravenous Experience (ALIVE) study. Am J Epidemiol. 2008;168(12):1460–9.
Huang T-HH, Lee W-CC. Bounding formulas for selection bias. Am J Epidemiol. 2015;182(10):868–72.
Smith LH, VanderWeele TJ. Bounding bias due to selection. Epidemiology. 2019;30(4):509–16.
Smith LH, VanderWeele TJ. Simple sensitivity analysis for control selection bias. Epidemiology. 2020;31(5).
Flanders WD, Ye D. Limits for the magnitude of M-bias and certain other types of structural selection bias. Epidemiology. 2019;30(4):501–8.
Tudball M, Zhao Q, Hughes R, Tilling K, Bowden J. An interval estimation approach to sample selection bias [Internet]. 2019. Available from: http://arxiv.org/abs/1906.10159.
VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268–75.
Heckman JJ. Sample selection bias as a specification error. Econometrica. 1979;47(1):153–61.
Bärnighausen T, Bor J, Wandira-Kazibwe S, Canning D. Correcting HIV prevalence estimates for survey nonparticipation using Heckman-type selection models. Epidemiology. 2011;22(1):27–35.
McGovern ME, Bärnighausen T, Marra G, Radice R. On the assumption of bivariate normality in selection models. Epidemiology. 2015;26(2):229–37.
Marra G, Radice R, Bärnighausen T, Wood SN, McGovern ME. A simultaneous equation approach to estimating HIV prevalence with nonignorable missing responses. J Am Stat Assoc. 2017;112(518):484–96.
Marden JR, Wang L, Tchetgen Tchetgen EJ, Walter S, Glymour MM, Wirth KE, et al. Implementation of instrumental variable bounds for data missing not at random. Epidemiology. 2018;29(3):1.
• West BT, McCabe SE. Alternative approaches to assessing nonresponse bias in longitudinal survey estimates: an application to substance-use outcomes among young adults in the United States. Am J Epidemiol. 2017;185(7):591–600 Application and comparison of multiple methods for estimating prevalence under selection, with a recommendation for a procedure for sensitivity analysis.
Vansteelandt S, Walter S, Tchetgen ET. Eliminating survivor bias in two-stage instrumental variable estimators. Epidemiology. 2018;29(4):536–41.
Swanson SA. A practical guide to selection bias in instrumental variable analyses. Epidemiology. 2019;30(3):345–9.
• Hughes RA, Davies NM, Davey Smith G, Tilling K. Selection bias when estimating average treatment effects using one-sample instrumental variable analysis. Epidemiology. 2019;30(3):350–7 Describes using DAGs selection mechanisms under which two-stage least squares is biased.
Smit RAJJ, Trompet S, Dekkers OM, Jukema JW, le Cessie S. Survival bias in Mendelian randomization studies: a threat to causal inference. Epidemiology. 2019;30(6):813–6.
Mostofsky E, Coull BA, Mittleman MA. Analysis of observational self-matched data to examine acute triggers of outcome events with abrupt onset. Epidemiology. 2018;29(6):804–16.
Mooney SJ. Invited commentary: the tao of clinical cohort analysis—when the transitions that can be spoken of are not the true transitions. Am J Epidemiol. 2017;185(8):636–8.
Dowd JB, Hamoudi A. Is life expectancy really falling for groups of low socio-economic status? Lagged selection bias and artefactual trends in mortality. Int J Epidemiol. 2014;43(4):983–8.
Bolzern J, Mnyama N, Bosanquet K, Torgerson DJ. A review of cluster randomized trials found statistical evidence of selection bias. J Clin Epidemiol. 2018;99:106–12.
Uschner D, Hilgers RD, Heussen N. The impact of selection bias in randomized multi-arm parallel group clinical trials. PLoS One. 2018;13(1):1–18.
Acknowledgements
I am grateful to Joy Shi for the helpful comments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that there is no conflict of interest.
Human and Animal Rights
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Epidemiologic Methods
Rights and permissions
About this article
Cite this article
Smith, L.H. Selection Mechanisms and Their Consequences: Understanding and Addressing Selection Bias. Curr Epidemiol Rep 7, 179–189 (2020). https://doi.org/10.1007/s40471-020-00241-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40471-020-00241-6