Abstract
Purpose of Review
Evidence suggests that youth from marginalized racial/ethnic groups (i.e., Latino, Black, Asian American, Native American youth) engage in disinhibited eating at greater rates than their non-Latino White peers. This review aims to discuss the prevalence of disinhibited eating among youth of color, identify culturally-specific correlates that may represent promising targets for prevention or treatment, and provide recommendations for future research.
Recent Findings
We restricted our literature review to studies published between 2010 and 2020 using samples of children and adolescents of color living in the USA. The relevant literature was limited: the majority of studies focused only on prevalence rates, combined racial/ethnic groups, and utilized the same samples for multiple publications. The literature on disinhibited eating among Asian American and Native American youth was particularly sparse. Disinhibited eating prevalence varied by racial/ethnic group, sample, and type of disinhibited eating, but rates were generally the same or higher when comparing youth of color to non-Latino White youth.
Summary
Given racial/ethnic health disparities that begin in childhood and persist in adulthood, it is vital that researchers investigate ways to better address disinhibited eating in underserved populations. Recommendations for future research include the following: (1) investigating theoretically relevant mechanisms to target in prevention and/or treatment programs with youth of color; (2) conducting more in-depth studies within specific groups (e.g., Asian Americans) versus only adjusting for race/ethnicity or comparing racial/ethnic groups; and (3) performing racially, culturally, and linguistically sensitive community-based participatory research to increase relevance, acceptability, and feasibility of interventions in marginalized communities.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Faith MS, Allison DB, Geliebter A. Emotional eating and obesity: theoretical considerations and practical recommendations. Overweight and weight management: the health professional's guide to understanding and practice. Gaithersburg, MD, US: Aspen Publishers; 1997. p. 439–65.
Goldschmidt AB, Loth KA, MacLehose RF, Pisetsky EM, Berge JM, Neumark-Sztainer D. Overeating with and without loss of control: associations with weight status, weight-related characteristics, and psychosocial health. Int J Eat Disord. 2015;48(8):1150–7. https://doi.org/10.1002/eat.22465.
Kral TVE, Faith MS. Influences on child eating and weight development from a behavioral genetics perspective. J Pediatr Psychol. 2009;34(6):596–605. https://doi.org/10.1093/jpepsy/jsn037.
Shomaker LB, Tanofsky-Kraff M, Yanovski JA. Disinhibited eating and body weight in youth. In: Preedy V, Watson R, Martin C, editors. Handbook of behavior, food and nutrition. New York, NY: Springer; 2011.
Tanofsky-Kraff M. Binge eating among children and adolescents. In: Jelalian E, Steele RG, editors. Handbook of Childhood and Adolescent Obesity. Issues in Clinical Child Psychology. Boston, MA: Springer; 2008.
Shomaker LB, Tanofsky-Kraff M, Zocca JM, Courville A, Kozlosky M, Columbo KM, et al. Eating in the absence of hunger in adolescents: intake after a large-array meal compared with that after a standardized meal. Am J Clin Nutr. 2010;92(4):697–703. https://doi.org/10.3945/ajcn.2010.29812.
Zocca JM, Shomaker LB, Tanofsky-Kraff M, Columbo KM, Raciti GR, Brady SM, et al. Links between mothers’ and children’s disinhibited eating and children’s adiposity. Appetite. 2011;56(2):324–31. https://doi.org/10.1016/j.appet.2010.12.014.
Radin RM, Tanofsky-Kraff M, Shomaker LB, Kelly NR, Pickworth CK, Shank LM, et al. Metabolic characteristics of youth with loss of control eating. Eat Behav. 2015;19:86–9. https://doi.org/10.1016/j.eatbeh.2015.07.002.
Shank LM, Tanofsky-Kraff M, Radin RM, Shomaker LB, Wilfley DE, Young JF, et al. Remission of loss of control eating and changes in components of the metabolic syndrome. Int J Eat Disord. 2018;51(6):565–73. https://doi.org/10.1002/eat.22866.
Stojek MMK, Tanofsky-Kraff M, Shomaker LB, Kelly NR, Thompson KA, Mehari RD, et al. Associations of adolescent emotional and loss of control eating with 1-year changes in disordered eating, weight, and adiposity. Int J Eat Disord. 2017;50(5):551–60. https://doi.org/10.1002/eat.22636.
Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA. A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. Int J Eat Disord. 2009;42(1):26–30. https://doi.org/10.1002/eat.20580.
Ogden CL, Fryar CD, Martin CB, Freedman DS, Carroll MD, Gu Q, Hales CM Trends in obesity prevalence by race and Hispanic origin—1999-2000 to 2017-2018. J Am Med Assoc 2020. doi:https://doi.org/10.1001/jama.2020.14590, 324, 1208, 1210.
Bisaga K, Whitaker A, Davies M, Chuang S, Feldman J, Walsh BT. Eating disorder and depressive symptoms in urban high school girls from different ethnic backgrounds. J Dev Behav Pediatr. 2005;26(4):257–66. https://doi.org/10.1097/00004703-200508000-00001.
Pernick Y, Nichols JF, Rauh MJ, Kern M, Ji M, Lawson MJ, et al. Disordered eating among a multi-racial/ethnic sample of female high-school athletes. J Adolesc Health. 2006;38(6):689–95. https://doi.org/10.1016/j.jadohealth.2005.07.003.
Striegel-Moore RH, Rosselli F, Holtzman N, Dierker L, Becker AE, Swaney G. Behavioral symptoms of eating disorders in native Americans: results from the add health survey wave III. Int J Eat Disord 2011;44(6):561–566. doi:https://doi.org/10.1002/eat.20894.
Rodgers RF, Watts AW, Austin SB, Haines J, Neumark-Sztainer D. Disordered eating in ethnic minority adolescents with overweight. International Journal of Eating Disorders. 2017;50(6):665–671. doi:https://doi.org/10.1002/eat.22652. This large, population-based study is one of two recent studies to examine disinhibited eating in Asian American youth. In a sample of 2,271 adolescents, prevalence of overeating across race by sex was investigated.
Lee-Winn AE, Reinblatt SP, Mojtabai R, Mendelson T. Gender and racial/ethnic differences in binge eating symptoms in a nationally representative sample of adolescents in the United States. Eat Behav. 2016;22:27–33. https://doi.org/10.1016/j.eatbeh.2016.03.021.
Schueller SM, Hunter JF, Figueroa C, Aguilera A. Use of digital mental health for marginalized and underserved populations. Current Treatment Options in Psychiatry. 2019;6(3):243–55. https://doi.org/10.1007/s40501-019-00181-z.
Agyemang C, Bhopal R, Bruijnzeels M. Negro, Black, Black African, African Caribbean, African American or what? Labelling African origin populations in the health arena in the 21st century. J Epidemiol Community Health 2005;59(12):1014. doi:https://doi.org/10.1136/jech.2005.035964, 1018.
Martínez DE, Gonzalez KE. “Latino” or “Hispanic”? The sociodemographic correlates of panethnic label preferences among U.S. Latinos/Hispanics. Sociological perspectives. 2020:73112142095037. https://doi.org/10.1177/0731121420950371.
Bucchianeri MM, Fernandes N, Loth K, Hannan PJ, Eisenberg ME, Neumark-Sztainer D. Body dissatisfaction: do associations with disordered eating and psychological well-being differ across race/ethnicity in adolescent girls and boys? Cultur Divers Ethnic Minor Psychol. 2016;22(1):137–46. https://doi.org/10.1037/cdp0000036.
Elliott CA, Tanofsky-Kraff M, Mirza NM. Parent report of binge eating in Hispanic, African American and Caucasian youth. Eat Behav. 2013;14(1):1–6. https://doi.org/10.1016/j.eatbeh.2012.10.007.
Nguyen-Michel ST, Unger JB, Spruijt-Metz D. Dietary correlates of emotional eating in adolescence. Appetite. 2007;49(2):494–9. https://doi.org/10.1016/j.appet.2007.03.005.
Rollins BY, Riggs NR, Spruijt-Metz D, McClain AD, Chou CP, Pentz MA. Psychometrics of the Eating in Emotional Situations Questionnaire (EESQ) among low-income Latino elementary-school children. Eat Behav. 2011;12(2):156–9. https://doi.org/10.1016/j.eatbeh.2011.01.004.
Berry JW. Marginality, stress and ethnic identification in an acculturated aboriginal community. J Cross-Cult Psychol 1970;1(3):239–252. doi:https://doi.org/10.1177/135910457000100303.
Berry JW. Immigration, acculturation, and adaptation. Appl Psychol. 1997;46(1):5–34. https://doi.org/10.1111/j.1464-0597.1997.tb01087.x.
Berry JW, Kim U, Minde T, Mok D. Comparative studies of acculturative stress. Int Migr Rev. 1987;21(3):491–511. https://doi.org/10.1177/019791838702100303.
Simmons S, Limbers CA. Acculturative stress and emotional eating in Latino adolescents. Eating and Weight Disorders. 2019;24(5):905. https://doi.org/10.1007/s40519-018-0602-2This is one of the only recent studies investigating correlates of disinhibited eating among Latino adolescents. The roles of acculturative stress and generational status on emotional eating were examined.
Higgins Neyland MK, Bardone-Cone AM. Tests of escape theory of binge eating among Latinas. Cult Divers Ethn Minor Psychol. 2017;23(3):373–81. https://doi.org/10.1037/cdp0000130.
Cassidy OL, Matheson B, Osborn R, Vannucci A, Kozlosky M, Shomaker LB, et al. Loss of control eating in African-American and Caucasian youth. Eat Behav. 2012;13(2):174–8. https://doi.org/10.1016/j.eatbeh.2012.01.003.
Kronenfeld LW, Reba-Harrelson L, Von Holle A, Reyes ML, Bulik CM. Ethnic and racial differences in body size perception and satisfaction. Body Image. 2010;7(2):131–6. https://doi.org/10.1016/j.bodyim.2009.11.002.
Neumark-Sztainer D, Falkner N, Story M, Perry C, Hannan PJ, Mulert S. Weight-teasing among adolescents: correlations with weight status and disordered eating behaviors. Int J Obes Relat Metab Disord. 2002;26(1):123–31. https://doi.org/10.1038/sj.ijo.0801853.
Musci RJ, Hart SR, Ialongo N. Internalizing antecedents and consequences of binge-eating behaviors in a community-based, urban sample of African American females. Prev Sci. 2014;15(4):570–8. https://doi.org/10.1007/s11121-013-0411-9.
Cassidy O, Eichen DM, Burke NL, Patmore J, Shore A, Radin RM, et al. Engaging African American adolescents and stakeholders to adapt interpersonal psychotherapy for weight gain prevention. J Black Psychol. 2018;44(2):128–61. https://doi.org/10.1177/0095798417747142.
Goode RW, Cowell MM, Mazzeo SE, Cooper-Lewter C, Forte A, Olayia O-I, et al. Binge eating and binge-eating disorder in Black women: a systematic review. Int J Eat Disord. 2020;53(4):491–507. https://doi.org/10.1002/eat.23217.
Coleman A, O'Neil J, Ferris AM. The mediation effect between everyday discrimination, gender role conflict, emotional eating, and obesity in African American fathers and sons. Psychology of Men & Masculinities. 2019;20(2):182–193. doi:https://doi.org/10.1037/men0000201. This study is one of the only recent studies that investigated factors that uniquely contribute to disinhibited eating in Black youth. The roles of discrimination and gender role conflict on emotional eating were examined among Black boys.
Kelly NR, Cotter EW, Guidinger C, Williamson G. Perceived discrimination, emotion dysregulation and loss of control eating in young men. Eat Behav. 2020;37:101387. https://doi.org/10.1016/j.eatbeh.2020.101387.
Striegel-Moore RH, Rosselli F, Holtzman N, Dierker L, Becker AE, Swaney G. Behavioral symptoms of eating disorders in native Americans: results from the ADD health survey wave III. The International Journal of Eating Disorders 2011;44(6):561–566. doi:https://doi.org/10.1002/eat.20894.
Nagata JM, Garber AK, Tabler JL, Murray SB, Bibbins-Domingo K. Prevalence and correlates of disordered eating behaviors among young adults with overweight or obesity. J Gen Intern Med. 2018;33(8):1337–43. https://doi.org/10.1007/s11606-018-4465-zThis study, which utilized a large, nationally representative sample, is the only recent study to examine disinhibited eating in Native American young adults. In a sample of 14,322 young adults, the authors examined the prevalence of binge eating behaviors across race.
Belcher BR, Nguyen-Rodriguez ST, McClain AD, Hsu Y-W, Unger JB, Spruijt-Metz D. The influence of worries on emotional eating, weight concerns, and body mass index in Latina female youth. J Adolesc Health. 2011;48(5):487–92. https://doi.org/10.1016/j.jadohealth.2010.08.008.
Chamberlin A, Nguyen-Rodriguez S, Gray VB, Reiboldt W, Peterson C, Spruijt-Metz D. Academic-related factors and emotional eating in adolescents. The Journal of School Health. 2018;88(7):493–9. https://doi.org/10.1111/josh.12638.
Egbert AH, Haedt-Matt A, Smith KE, Culbert K, Engel S, Goldschmidt AB. Momentary associations between positive affect dimensions and dysregulated eating during puberty in a diverse sample of youth with overweight/obesity. International Journal of Eating Disorders. 2020;n/a(n/a). https://doi.org/10.1002/eat.23342This is one of the only recent studies looking at age cohort differences in factors related to overeating among a diverse sample of youth. This study used ecological momentary assessment to investigate factors associated with more granular changes in overeating.
Pluhar EI, Abdullah S, Burton ET. Endorsement of binge eating symptoms in a sample of predominantly non-Hispanic Black adolescents. Clin Pediatr 2020;59(8):766–772. doi:https://doi.org/10.1177/0009922820915897.
Neumark-Sztainer D, Bauer KW, Friend S, Hannan PJ, Story M, Berge JM. Family weight talk and dieting: how much do they matter for body dissatisfaction and disordered eating behaviors in adolescent girls? J Adolesc Health. 2010;47(3):270–6. https://doi.org/10.1016/j.jadohealth.2010.02.001.
Olvera N, Dempsey A, Gonzalez E, Abrahamson C. Weight-related teasing, emotional eating, and weight control behaviors in Hispanic and African American girls. Eat Behav. 2013;14(4):513–7. https://doi.org/10.1016/j.eatbeh.2013.06.012.
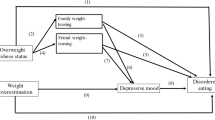
Olvera N, McCarley K, Matthews-Ewald MR, Fisher F, Jones M, Flynn EG. Pathways for disordered eating behaviors in minority girls: the role of adiposity, peer weight-related teasing, and desire to be thinner. J Early Adolesc. 2015;37(3):367–86. https://doi.org/10.1177/0272431615609155.
Berge JM, Wall M, Larson N, Eisenberg ME, Loth KA, Neumark-Sztainer D. The unique and additive associations of family functioning and parenting practices with disordered eating behaviors in diverse adolescents. J Behav Med. 2014;37(2):205–17. https://doi.org/10.1007/s10865-012-9478-1.
Ledoux T, Watson K, Baranowski J, Tepper BJ, Baranowski T. Overeating styles and adiposity among multiethnic youth. Appetite. 2011;56(1):71–7. https://doi.org/10.1016/j.appet.2010.11.145.
Marcelo AK, Yates TM. Young children's ethnic-racial identity moderates the impact of early discrimination experiences on child behavior problems. Cult Divers Ethn Minor Psychol. 2019;25(2):253–65. https://doi.org/10.1037/cdp0000220.
Lacey JH. Pathogenesis. In: Downey LJ, Malkin JC, editors. Current approaches: bulimia nervosa. Southhampton, UK: Duphar; 1986. p. 17–26.
Lacey JH, Coker S, Birtchnell SA. Bulimia: factors associated with its etiology and maintenance. Int J Eat Disord. 1986;5(3):475–87. https://doi.org/10.1002/1098-108X(198603)5:3<475::AID-EAT2260050306>3.0.CO;2-0.
Beccia AL, Jesdale WM, Lapane KL. Associations between perceived everyday discrimination, discrimination attributions, and binge eating among Latinas: Results from the National Latino and Asian American Study. Annals of Epidemiology. 2020;45:32–9. https://doi.org/10.1016/j.annepidem.2020.03.012This study utilized a sample of 1,014 Latinas drawn from a large, nationally representative community survey and investigated the relationships between binge eating, discrimination, and discrimination attribution.
Phinney JS. Ethnic identity in adolescents and adults: review of research. Psychol Bull. 1990;108(3):499–514. https://doi.org/10.1037/0033-2909.108.3.499.
Umaña-Taylor AJ, Yazedjian A, Bámaca-Gómez M. Developing the ethnic identity scale using Eriksonian and social identity perspectives. Identity. 2004;4(1):9–38. https://doi.org/10.1207/S1532706XID0401_2.
Pascoe EA, Richman LS. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531–54. https://doi.org/10.1037/a0016059.
Smith TB, Silva L. Ethnic identity and personal well-being of people of color: a meta-analysis. J Couns Psychol. 2011;58(1):42–60. https://doi.org/10.1037/a0021528.
Shuttlesworth ME, Zotter D. Disordered eating in African American and Caucasian women: the role of ethnic identity. J Black Stud. 2011;42(6):906–22. https://doi.org/10.1177/0021934710396368.
Kelly NR, Smith TM, GCN H, Guidinger C, Williamson G, Budd EL, et al. Perceptions of general and postpresidential election discrimination are associated with loss of control eating among racially/ethnically diverse young men. International Journal of Eating Disorders. 2018;51(1):28–38. https://doi.org/10.1002/eat.22803This study utilized a sample of 798 Black, Latino, and Asian American young men and investigated the relationship between discrimination and LOC-eating, with ethnic identity serving as a moderator.
Guidinger C, Williamson G, Kelly NR. Cultural values and ethnic identity are important considerations in the link between emotion dysregulation and loss of control eating in Asian/Asian American men. Appetite. 2020;151:104693. https://doi.org/10.1016/j.appet.2020.104693.
West CE, Goldschmidt AB, Mason SM, Neumark-Sztainer D. Differences in risk factors for binge eating by socioeconomic status in a community-based sample of adolescents: Findings from Project EAT. International Journal of Eating Disorders. 2019;52(6):659–68. https://doi.org/10.1002/eat.23079This study investigated the longitudinal relationship between food insecurity and binge eating risk among a sample of 2,179 adolescents.
Tester JM, Lang TC, Laraia BA. Disordered eating behaviours and food insecurity: a qualitative study about children with obesity in low-income households. Obes Res Clin Pract. 2015;10(5):544–52. https://doi.org/10.1016/j.orcp.2015.11.007.
Kral TVE, Chittams J, Moore RH. Relationship between food insecurity, child weight status, and parent-reported child eating and snacking behaviors. Journal for Specialists in Pediatric Nursing. 2017;22(2):e12177. https://doi.org/10.1111/jspn.12177.
Drewnowski A. The cost of US foods as related to their nutritive value. Am J Clin Nutr. 2010;92(5):1181–8. https://doi.org/10.3945/ajcn.2010.29300.
Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A. Household food security in the United States in 2016. In: Service ER, editor. Economic Research Report. ERR-237 ed: U.S. Department of Agriculture; 2017.
Jernigan VBB, Huyser KR, Valdes J, Simonds VW. Food insecurity among American Indians and Alaska natives: a national profile using the current population survey-food security supplement. J Hunger Environ Nutr 2017;12(1):1–10. doi:https://doi.org/10.1080/19320248.2016.1227750.
Semega J, Kollar M, Creamer J, Mohanty A. Income and poverty in the United States: 2018. In: Bureau USC, editor. P60–266(RV) ed. Washington, DC: U.S. Government Printing Office; 2020.
Yu M, Lombe M, Nebbitt VE. Food stamp program participation, informal supports, household food security and child food security: a comparison of African American and Caucasian households in poverty. Child Youth Serv Rev. 2010;32(5):767–73. https://doi.org/10.1016/j.childyouth.2010.01.015.
Odoms-Young A, Bruce MA. Examining the impact of structural racism on food insecurity: Implications for addressing racial/ethnic disparities. Fam Community Health. 2018;41 Suppl 2 Suppl, Food Insecurity and Obesity(Suppl 2 FOOD INSECURITY AND OBESITY):S3-S6. doi:https://doi.org/10.1097/FCH.0000000000000183.
Min J, Wen X, Xue H, Wang Y. Ethnic disparities in childhood BMI trajectories and obesity and potential causes among 29,250 US children: findings from the early childhood longitudinal study-birth and kindergarten cohorts. Int J Obes 2018;42(9):1661–1670. doi:https://doi.org/10.1038/s41366-018-0091-4.
Kit BK, Kuklina E, Carroll MD, Ostchega Y, Freedman DS, Ogden CL. Prevalence of and trends in dyslipidemia and blood pressure among US children and adolescents, 1999-2012. JAMA Pediatr. 2015;169(3):272–9. https://doi.org/10.1001/jamapediatrics.2014.3216.
Jayawardene WP, Lohrmann D, Dickinson S, Talagala S, Torabi M. Clinical measures of obesity and cumulative cardiometabolic risk in adolescents: obesity and cardiometabolic risk in adolescents. Clinical Obesity. 2017;7(1):11–21. https://doi.org/10.1111/cob.12171.
Bullock A, Sheff K, Moore K, Manson S. Obesity and overweight in American Indian and Alaska native children, 2006-2015. Am J Public Health. 2017;107(9):1502–7. https://doi.org/10.2105/AJPH.2017.303904.
Divers J, Mayer-Davis EJ, Lawrence JM, Isom S, Dabelea D, Dolan L et al. Trends in incidence of type 1 and type 2 diabetes among youths — Selected counties and Indian reservations, United States, 2002–2015. Morbidity and Mortality Weekly Report. 2020;69(6):161–5. doi:https://doi.org/10.15585/mmwr.mm6906a3.
Brown AF, Liang L-J, Vassar SD, Escarce JJ, Merkin SS, Cheng E, Richards A, Seeman T, Longstreth Jr WT Trends in racial/ethnic and nativity disparities in cardiovascular health among adults without prevalent cardiovascular disease in the United States, 1988 to 2014. Ann Intern Med 2018;168(8):541–549. doi:https://doi.org/10.7326/M17-0996.
Hutchinson RN, Shin S. Systematic review of health disparities for cardiovascular diseases and associated factors among American Indian and Alaska native populations. PLoS One. 2014;9(1):e80973. https://doi.org/10.1371/journal.pone.0080973.
Nguyen-Rodriguez ST, McClain AD, Spruijt-Metz D. Anxiety mediates the relationship between sleep onset latency and emotional eating in minority children. Eat Behav. 2010;11(4):297–300. https://doi.org/10.1016/j.eatbeh.2010.07.003.
Scheurich JJ, Young MD. Coloring epistemologies: are our research epistemologies racially biased? Educ Res. 1997;26(4):4–16. https://doi.org/10.2307/1176879.
Ford DY, Moore JL, Whiting GW, Grantham TC. Conducting cross-cultural research: controversy, cautions, concerns, and considerations. Roeper Rev. 2008;30(2):82–92. https://doi.org/10.1080/02783190801954924.
Burke NL, Tanofsky-Kraff M, Crosby R, Mehari RD, Marwitz SE, Broadney MM, Shomaker LB, Kelly NR, Schvey NA, Cassidy O, Yanovski SZ, Yanovski JA Measurement invariance of the eating disorder examination in Black and White children and adolescents. Int J Eat Disord 2017;50(7):758–768. doi:https://doi.org/10.1002/eat.22713.
Sue DW, Sue D. Counseling the culturally different. 3rd ed. New York: John Wiley; 1999.
Cassidy O, Sbrocco T, Tanofsky-Kraff M. Utilizing non-traditional research designs to explore culture-specific risk factors for eating disorders in African American adolescents. Adv Eat Disord. 2015;3(1):91–102. https://doi.org/10.1080/21662630.2014.948470.
Bender MS, Clark MJ. Cultural adaptation for ethnic diversity: a review of obesity interventions for preschool children. Calif J Health Promot. 2011;9(2):40–60.
Clark MJ. Cross-cultural research: challenge and competence. Int J Nurs Pract. 2012;18(s2):28–37. https://doi.org/10.1111/j.1440-172X.2012.02026.x.
Rodgers GP, Gibbons GH. Obesity and hypertension in the time of COVID-19. JAMA. 2020. doi:https://doi.org/10.1001/jama.2020.16753. This article discusses health disparities in obesity, hypertension, and COVID-19 among communities of color, as well as the roles structural racism and social determinants of health play.
Adler N, Cutler D, Fielding J, Galea S, Glymour M, Koh H et al. Addressing social determinants of health and health disparities: A vital direction for health and health care. NAM Perspectives. 2016;6. doi:https://doi.org/10.31478/201609t.
Funding
This work if funded by the Defense Health Agency MED 83-10180 (M. Haigney).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Disclaimer
The opinions and assertions expressed herein are those of the authors and are not to be construed as reflecting the views of the U.S. Department of Defense.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Food Addiction
Rights and permissions
About this article
Cite this article
Neyland, M.K.H., Rice, A., Shank, L.M. et al. Prevalence and Correlates of Disinhibited Eating in Youth from Marginalized Racial/Ethnic Groups. Curr Addict Rep 8, 1–11 (2021). https://doi.org/10.1007/s40429-020-00347-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40429-020-00347-3