Abstract
Purpose
To evaluate the association between children’s pain/distress levels and patient characteristics (age, sex, history of dental pain), sedation type (level of sedation, sedative regimen), nociception and pain intensity reported by the parents in sedated children undergoing minimally invasive dental treatment.
Methods
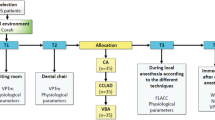
This clinical study evaluated secondary outcomes of an RCT that evaluated the efficacy of dexmedetomidine sedation with or without ketamine. Only children who had nociception levels recorded using the Analgesia Nociception Index (ANI) were included (0–100; 0 = highest nociception). FLACC scale (Face, Legs, Activity, Cry and Consolability) was used to assess children’s pain/distress (0–10; 0 = no pain/distress). Parental proxy report of the child’s pain intensity during the treatment was performed using the Visual Analogue Scale (VAS; 0–100; 0 = no pain). The association between ANI, children’s age and sex, dental pain history, sedation level, sedative regimen, and VAS with the FLACC was verified using the generalised estimation equation analysis (alpha 0.05).
Results
Participants were 31 children (51.6% boys) and their parents (90.3% mothers). Median FLACC was 3.3 (25th–75th percentiles 1.7–8.2), ANI 80.9 (74.7–85.8), and VAS 10 (1–23). FLACC associated with ANI (OR 0.96; 95% CI 0.93–0.99; p = 0.02), moderate sedation (0.13; 0.03–0.50; p = 0.003), and VAS (1.05; 1.01–1.10; p = 0.01).
Conclusion
Pain/distress was generally low and more prominent with minimal (versus moderate) sedation and higher nociception.


Similar content being viewed by others
Data availability
Data are available on request from the authors.
References
Beltramini A, Milojevic K, Pateron D. Pain assessment in newborns, infants, and children. Pediatr Ann. 2017;46(10):e387–95. https://doi.org/10.3928/19382359-20170921-03.
Berde C, Joanne W. Pain, anxiety, distress, and suffering: interrelated, but not interchangeable. J Pediatr. 2002;142(4):361–3.
Brilhante VOM, Corrêa-Faria P, Machado GCM, Costa LR. Carers’ and paediatric dentists’ perceptions of children’s pain during restorative treatment. Eur Arch Paediatr Dent. 2020;21(2):271–6. https://doi.org/10.1007/s40368-019-00486-w.
Costa LR, Bendo CB, Daher A, Heidari E, Rocha RS, Moreira APDSC, Moura LS, Banerjee A, Newton JT, Hosey MT. A curriculum for behaviour and oral healthcare management for dentally anxious children- Recommendations from the Children Experiencing Dental Anxiety: Collaboration on Research and Education (CEDACORE). Int J Paediatr Dentistry 2020; 30(5), 556–569.
Coté CJ, Wilson S. American Academy of pediatrics; American Academy of pediatric dentistry. Guidelines for monitoring and management of pediatric patients before, during, and after sedation or diagnostic and therapeutic procedures. Pediatrics. 2019;143(6): e20191000. https://doi.org/10.1542/peds.2019-1000.
Crellin D, Harrison D, Santamaria N, Babl FE. Comparison of the psychometric properties of the FLACC Scale, the MBPS and the observer applied visual analogue scale used to assess procedural pain. J Pain Res. 2021;14:881–92.
de Menezes Abreu DM, Leal SC, Frencken J. Self-Report of pain in children treated according to the atraumatic restorative treatment and the conventional restorative treatment–a pilot study. JOCPD. 2009;34(2):151–5.
Dorri M, Martinez-Zapata MJ, Walsh T, Marinho VCC, Sheiham A, Zaror C. Atraumatic restorative treatment versus conventional restorative treatment for managing dental caries. Cochrane Database of Systematic Reviews 2017 https://doi.org/10.1002/14651858.CD008072.pub2. Accessed January 19, 2021
Doyle DJ, Garmon EH. "American Society of Anesthesiologists classification (ASA class)." StatPearls [Internet]. StatPearls Publishing 2018.
e Silva LOJ, Lee JY, Bellolio F, Homme JL, Anderson JL. Intranasal ketamine for acute pain management in children: A systematic review and meta-analysis. Am J Emergency Med. 2020. https://doi.org/10.1016/j.ajem.2020.05.094.
Frankl S, Shiere F, Fogels H. Should the parent remain with the child in the dental operatory. J Dent Child. 1962;29:150–63.
Gall O, Champigneulle B, Schweitzer B, Deram T, Maupain O, Montmayeur Verchere J, Orliaguet G. Postoperative pain assessment in children: a pilot study of the usefulness of the analgesia nociception index. BJA. 2015;115(6):890–5.
Gazi M, Abitağaoğlu S, Turan G, Köksal C, Akgün FN, Arı DE. Evaluation of the effects of dexmedetomidine and remifentanil on pain with the analgesia nociception index in the perioperative period in hysteroscopies under general anesthesia: a randomised prospective study. Saudi Med J. 2018;39(10):1017.
Hosey MT. Managing anxious children: the use of conscious sedation in paediatric dentistry. Int J Paediatr Dent. 2002;12(5):359–72. https://doi.org/10.1046/j.1365-263x.2002.03792.x.
Howard R, Carter B, Curry J, Morton N, Rivett K, Tyrrell J, Walker S, Williams G. Association of paediatric anaesthetists of Great Britain and Ireland. Postoperat Pain Paediatr Anaesth. 2008;18:36–63.
IASP Terminology- IASP. iasp-pain.org. Available from https://www.iasp- pain.org/resources/terminology/#pain. Accessed November 10, 2020.
Jeanne M, Logier R, De Jonckheere J, Tavernier B. Validation of a graphic measurement of heart rate variability to assess analgesia/nociception balance during general anesthesia. In 2009 Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 1840–1843.
Julien-Marsollier F, Rachdi K, Caballero MJ, Ayanmanesh F, Vacher T, Horlin AL, Skhiri A, Brasher C, Michelet D, Dahmani S. Evaluation of the analgesia nociception index for monitoring intraoperative analgesia in children. Br J Anaesth. 2018;121(2):462–8. https://doi.org/10.1016/j.bja.2018.03.034.
Kang MS, Park J, Kim J. Agreement of postoperative pain assessment by parents and clinicians in children undergoing orthopedic surgery. J Trauma Nurs. 2020;27(5):302–9.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–63. https://doi.org/10.1016/j.jcm.2016.02.012.
Mahmoud M, Mason KP. Dexmedetomidine: review, update, and future considerations of paediatric perioperative and periprocedural applications and limitations. Br J Anaesth. 2015;115(2):171–82. https://doi.org/10.1093/bja/aev226.
Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B, Freiberger D, Lui PL. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985;32(4):429–34.
Merkel SI, Voepel-Lewis T, Shayevitz JR, Malviya S. The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurs. 1997;23:293–7.
Naranjo-Hernández D, Reina-Tosina J, Roa LM. Sensor technologies to manage the physiological traits of chronic pain: a review. Sensors. 2020;20(2):365. https://doi.org/10.3390/s20020365.
Sabourdin N, Arnaout M, Louvet N, Guye ML, Piana F, Constant I. Pain monitoring in anesthetised children: first assessment of skin conductance and analgesia- nociception index at different infusion rates of remifentanil. Pediatr Anesth. 2013;23(2):149–55.
Sado-Filho J, Corrêa-Faria P, Viana KA, Mendes FM, Mason KP, Costa LR, Costa PS. Intranasal dexmedetomidine compared to a combination of intranasal dexmedetomidine with ketamine for sedation of children requiring dental treatment: a randomised clinical trial. J Clin Med. 2021;10(13):2840. https://doi.org/10.3390/jcm10132840.
Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. PLoS Med. 2010;7: e1000251.
Scott J, Huskisson EC. Graphic representation of pain. Pain. 1976;2(2):175–84. https://doi.org/10.1016/0304-3959(76)90113-5.
The Joint Commission. Speak up: Anesthesia and Sedation. Available online:https://www.jointcommission.org/-/media/tjc/documents/resources/speak-up/speak-up-anesthesia-infographic-5-15-2020.pdf. Accessed 6 March 2022.
Tracey I, Mantyh PW. The cerebral signature for pain perception and its modulation. Neuron. 2007;55(3):377–91.
Acknowledgements
This study was funded by the Foundation for Research Support of the State of Goiás (Fundação de Amparo à Pesquisa do Estado de Goiás—FAPEG), Process number 201710267000525. Three authors (PCF, LGA and LRC) received research grants from the National Council for Scientific and Technological Development (CNPq) and the Coordination of Improvement of Higher Education Personnel (CAPES). The authors thank the Pediatric Dental Clinic research group (COP), which helped collect data.
Author information
Authors and Affiliations
Contributions
DAB, PCF, AAA, LGA and LRC conceived the ideas. DAB, AAA and PCF collected the data. DAB, PCF and LRC analysed the data. DAB led the writing. DAB, PCF, AAA, LGA, and LRC read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Baroni, D.A., Corrêa-Faria, P., Anabuki, A.A. et al. Nociception associated with pain/distress in young children sedated for dental treatment: a clinical study with objective and subjective measures. Eur Arch Paediatr Dent 24, 255–262 (2023). https://doi.org/10.1007/s40368-023-00782-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40368-023-00782-6