Abstract
Aims
This was to compare sleepiness, occlusion, dental arch and palatal dimensions between children with attention deficit hyperactivity disorders (ADHD) and healthy children (control group).
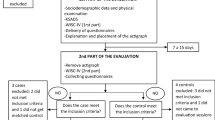
Methods
15 children with ADHD (10 boys, 5 girls, mean age 10.98 years) and 36 healthy age matched children (21 boys, 15 girls, mean age 10.60 years) were included. Intra-oral three-dimensional scans of the teeth and palate were performed to evaluate the occlusion, dental arch and palatal dimensions. Sleepiness was evaluated from the questionnaires. The differences between the two groups were analysed by Fisher’s exact test and general linear models adjusted for age and gender.
Results
The ADHD children had a significantly narrower dental arch at the gingival level of the canines (p < 0.05) and a tendency to increased prevalence of posterior cross-bite compared to the controls (13.3 vs. 0.0%, p = 0.086). The ADHD children snored significantly more (p < 0.05) and slept restlessly significantly more often (p < 0.0005) compared to the controls. The ADHD children had a tendency to sleep fewer hours during the night (p = 0.066) and felt inadequately rested in the morning (p = 0.051) compared to the controls.
Conclusion
The results indicate that sleepiness and palatal width, especially the more anterior skeletal part of the palate, may be affected in children with ADHD. The results may prove valuable in the diagnosis and treatment planning of children with ADHD. Further studies are needed to investigate sleep and dental relations in children with ADHD.

Similar content being viewed by others
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders DMS-5, Washington, DC. 2013.
Atmetlla G, Burgos V, Carrillo A, Chaskel R. Behavior and orofacial characteristics of children with attention-deficit hyperactivity disorder during a dental visit. J Clin Pediatr Dent. 2006;30:183–90.
Ashizawa T, Sarkar P. Myotonic dystrophy types 1 and 2. In: Aminoff MJ, Boller F, Swaab DF, editors. Handbook of clinical neurology. Amsterdam: Elsevier; 2011. p. 193–237.
Beiske KK, Kjelsberg FN, Ruud EA, Stavem K. Reliability and validity of a Norwegian version of the Epworth sleepiness scale. Sleep Breath. 2009;13(1):65–72.
Björk A, Krebs A, Solow B. A method for epidemiological registration of malocclusion. Acta Odont Scand. 1964;1:27–41.
Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. J Am Acad Child Adolesc Psychiatry. 2009;48:894–908.
Dahlberg G. Statistical methods for medical and biological students. New York: Interscience Publications press; 1940.
Davies W. Sex differences in attention deficit hyperactivity disorder: candidate genetic and endocrine mechanisms. Front Neuroendocrinol. 2014;35:331–46.
Galland BC, Tripp EG, Gray A, Taylor BJ. Apnea-hypopnea indices and snoring in children diagnosed with ADHD: a matched case-control study. Sleep Breath. 2011;15:455–62.
Gerlach M, Deckert J, Rothenberger A, Warnke A. Pathogenesis and pathophysiology of attention-deficit/hyperactivity disorder: from childhood to adulthood. J Neural Transm. 2008;115:151–3.
Gillberg C, Gillberg IC, Rasmussen P, et al. Co-existing disorders in ADHD—implications for diagnosis and intervention. Eur Child Adolesc Psychiatry. 2004;13:180–92.
Helm S. Prevalence of malocclusion in relation to development of the dentition. An epidemiological study of Danish school children. Acta Odontol Scand. 1970;58:1+.
Herman JH. Attention deficit/hyperactivity disorder and sleep in children. Sleep Med Clin. 2015;10:143–9.
Houston WJ. The analysis of errors in orthodontic measurements. Am J Orthod. 1983;83:382–90.
Huang YS, Guilleminault C, Li HY, et al. Attention-deficit/hyperactivity disorder with obstructive sleep apnea: a treatment outcome study. Sleep Med. 2007;8:18–30.
Janssen KC, Phillipson S, O’Connor J, Johns MW. Validation of the Epworth Sleepiness Scale for children and adolescents using Rasch analysis. Sleep Med. 2007;33:30–5.
Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–5.
Johns MW. Sensitivity and specificity of the multiple sleep latency test (MSLT), the maintenance of wakefulness test and the Epworth sleepiness scale: failure of the MSLT as a gold standard. J Sleep Res. 2000;9(1):5–11.
Khaledi-Paveh B, Khazaie H, Nasouri M, Ghadami MR, Tahmasian M. Evaluation of Berlin questionnaire validity for sleep apnea risk in sleep clinic populations. Basic Clin Neurosci. 2016;7:43–8.
Kiliaridis S, Mejersjo C, Thilander B. Muscle function and craniofacial morphology: a clinical study in patients with myotonic dystrophy. Eur J Orthod. 1989;11:131–8.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Lione R, Buongiorno M, Franchi L, Cozza P. Evaluation of maxillary arch dimensions and palatal morphology in mouth-breathing children by using digital dental casts. Int J Pediatr Otorhinolaryngol. 2014;78:91–5.
Margallo VS, Muxfeldt ES, Guimaraes GM, Salles GF. Diagnostic accuracy of the Berlin questionnaire in detecting obstructive sleep apnea in patients with resistant hypertension. J Hypertens. 2014;32:2030–6.
Nespoli L, Caprioglio A, Brunetti L, Nosetti L. Obstructive sleep apnea syndrome in childhood. Early Hum Dev. 2013;89:33–7.
Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–91.
Pirelli P, Saponara M, Guilleminault C. Rapid maxillary expansion in children with obstructive sleep apnea syndrome. Sleep. 2004;27:761–6.
Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. JCPP. 2015;56:345–65.
Proffit WR, Fields HW, Sarver DM. Contemporary orthodontics. St. Louis: Mosby Elsevier; 2007.
Ricketts RM. Respiratory obstruction syndrome. Am J Orthod. 1968;54:495–507.
Sabuncuoglu O. Understanding the relationships between breastfeeding, malocclusion, ADHD, sleep-disordered breathing and traumatic dental injuries. Med Hypotheses. 2013;80:315–20.
Sadeh A, Pergamin L, Bar-Haim Y. Sleep in children with attention-deficit hyperactivity disorder: a meta-analysis of polysomnographic studies. Sleep Med Rev. 2006;10:381–98.
Sedky K, Bennett DS, Carvalho KS. Attention deficit hyperactivity disorder and sleep disordered breathing in pediatric populations: a meta-analysis. Sleep Med Rev. 2014;18:349–56.
Sinha D, Guilleminault C. Sleep disordered breathing in children. Indian J Med Res. 2010;131:311–20.
Solow B. The dentoalveolar compensatory mechanism: background and clinical implications. Br J Orthod. 1980;7:145–61.
Solow B, Siersbaek-Nielsen S. Growth changes in head posture related to craniofacial development. Am J Orthod. 1986;89:132–40.
Solow B, Sonnesen L. Head posture and malocclusions. Eur J Orthod. 1998;20:685–93.
Solow B, Tallgren A. Head posture and craniofacial morphology. Am J Phys Anthrop. 1976;44:417–36.
Solow B, Ovesen J, Nielsen PW, Wildschiodtz G, Tallgren A. Head posture in obstructive sleep apnoea. Eur J Orthod. 1993;15:107–14.
Sundhedsstyrelsen. National Clinical Guideline for the Detection and Treatment of ADHD in Children and Adolescents - Focusing on the diagnosis “Disruption of Activity and Attention” and “Attention Disorder Without Hyperactivity According to the ICD-10”. 2014.
Tanaka MM, Johnston LE. The prediction of the size of unerupted canines and premolars in a contemporary orthodontic population. J Am Dent Assoc. 1974;88:798–801.
Thapar A, Cooper M. Attention deficit hyperactivity disorder. Lancet. 2016;387:1240–50.
Timms DJ. The effect of rapid maxillary expansion on nasal airway resistance. Br J Orthod. 1986;13:221–8.
White BC, Woodside DG, Cole P. The effect of rapid maxillary expansion on nasal airway resistance. J Otolaryngol. 1989;18:137–43.
Wiebe S, Carrier J, Frenette S, Gruber R. Sleep and sleepiness in children with attention deficit/hyperactivity disorder and controls. J Sleep Res. 2013;22:41–9.
Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490–9.
Acknowledgements
We extend our sincere gratitude to the families and children who participated in the study and to the persons who have made the recruitment of the ADHD and control children possible: Dorthe Barsøe, head of Furesø ADHD- and autismecenter, Syvstjernen, Bente Velling Johansen, head of ADHD Borupgårdskolen, Helsingør, Ruth Jacobsen, head of the community dental service of Copenhagen, and Stine Mia Ørstrup, head of the community dental clinic at Panum. Scanorto A/S is thanked for providing free access to the intraoral scanner and to the OnyxCeph software. Thank you to M.Sc. Ib Jarle Christensen, Hvidovre Hospital, for statistical assistance.
Funding
Scanorto A/S provided free access to the intraoral scanner and Image Instruments provided free access to the OnyxCeph software.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study was approved by the Scientific-Ethical Committee of Copenhagen (H-1-2014-130) and the Danish data protection agency (j.nr. 2015-57-0121).
Informed consent
Oral and written informed consent was given by the children’s parents/guardian.
Rights and permissions
About this article
Cite this article
Andersson, H., Sonnesen, L. Sleepiness, occlusion, dental arch and palatal dimensions in children attention deficit hyperactivity disorder (ADHD). Eur Arch Paediatr Dent 19, 91–97 (2018). https://doi.org/10.1007/s40368-018-0330-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40368-018-0330-3