Abstract
Purpose
To provide a systematic review and meta-analysis of published literature characterizing the prognostic value of pre-treatment, volume-based FDG-PET metrics in patients with advanced NSCLC.
Methods
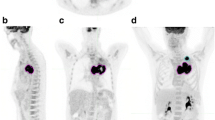
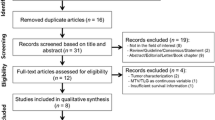
We conducted a systematic PubMed search to identify studies describing the prognostic value of volume-based PET metrics (total metabolic tumor volume [MTV] and/or total lesion glycolysis [TLG]) obtained prior to initiation of first-line systemic therapy for advanced NSCLC. Clinical endpoints examined were progression-free survival (PFS) and overall survival (OS). Hazard ratios for PFS and OS were taken directly from the original reports when available or extracted from survival curves. Inverse variance meta-analyses were performed to assess associations between PET metrics and clinical outcomes.
Results
Thirteen publications including 1,047 patients were included in our analysis. Patients from at least 9 studies received chemotherapy, at least 4 studies utilized targeted therapy, and only 1 study included patients treated with immunotherapy.
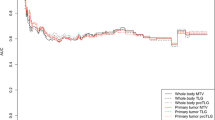
Random effects models demonstrated that high MTV is significantly associated with inferior PFS (HR 2.97, 95% CI 2.21–4.00, p < 0.001) and inferior OS (HR 2.73, 95% CI 2.18–3.41, p < 0.001). High TLG is also significantly associated with inferior PFS (HR 2.13, 95% CI 1.56–2.91, p < 0.001) and inferior OS (HR 2.06, 95% CI 1.75–2.44, p < 0.001).
Conclusion
Baseline PET metrics are powerful prognostic factors for advanced NSCLC patients who are treated with chemotherapy or targeted therapy. Further examination of the prognostic value of PET metrics for patients who receive first-line immunotherapy is warranted.





Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sung H et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Jonas DE et al (2021) Screening for lung cancer with low-dose computed tomography: an evidence review for the us preventive services task force. JAMA 325:971
Soria JC et al (2018) Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med 378(2):113–125
Reck M et al (2016) Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 375(19):1823–1833
Langer CJ et al (2016) Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomised, phase 2 cohort of the open-label KEYNOTE-021 study. Lancet Oncol 17(11):1497–1508
Mok TSK et al (2019) Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): a randomised, open-label, controlled, phase 3 trial. Lancet 393(10183):1819–1830
Gandhi L et al (2018) Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med 378(22):2078–2092
Paz-Ares L et al (2018) Pembrolizumab plus chemotherapy for squamous non-small-cell lung cancer. N Engl J Med 379(21):2040–2051
Brundage MD, Davies D, Mackillop WJ (2002) Prognostic factors in non-small cell lung cancer: a decade of progress. Chest 122(3):1037–1057
Im HJ et al (2015) Prognostic value of volumetric parameters of (18)F-FDG PET in non-small-cell lung cancer: a meta-analysis. Eur J Nucl Med Mol Imaging 42(2):241–251
Parmar MK, Torri V, Stewart L (1998) Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med 17(24):2815–2834
Yoo SW et al (2012) Metabolic tumor volume measured by F-18 FDG PET/CT can further stratify the prognosis of patients with stage IV non-small cell lung cancer. Nucl Med Mol Imaging 46(4):286–293
Zaizen Y et al (2012) Prognostic significance of total lesion glycolysis in patients with advanced non-small cell lung cancer receiving chemotherapy. Eur J Radiol 81(12):4179–4184
Chung HW et al (2014) FDG PET/CT metabolic tumor volume and total lesion glycolysis predict prognosis in patients with advanced lung adenocarcinoma. J Cancer Res Clin Oncol 140(1):89–98
Hyun MH et al (2019) Clinical implications of circulating cell-free DNA quantification and metabolic tumor burden in advanced non-small cell lung cancer. Lung Cancer 134:158–166
Nygaard AD et al (2014) The correlation between cell-free DNA and tumour burden was estimated by PET/CT in patients with advanced NSCLC. Br J Cancer 110(2):363–368
Sharma A et al (2018) Role of various metabolic parameters derived from baseline 18F-FDG PET/CT as prognostic markers in non-small cell lung cancer patients undergoing platinum-based chemotherapy. Clin Nucl Med 43(1):e8–e17
Ho TY et al (2015) Total lesion glycolysis determined per RECIST 1.1 criteria predicts survival in EGFR mutation-negative patients with advanced lung adenocarcinoma. Clin Nucl Med 40(6):e295–e299
Han EJ et al (2015) Prognostic value of early response assessment using 18F-FDG PET/CT in chemotherapy-treated patients with non-small-cell lung cancer. Nucl Med Commun 36(12):1187–1194
Liao S et al (2012) Prognostic value of the quantitative metabolic volumetric measurement on 18F-FDG PET/CT in Stage IV nonsurgical small-cell lung cancer. Acad Radiol 19(1):69–77
Ooi H et al (2016) Fluorodeoxyglucose uptake in advanced non-small cell lung cancer with and without pulmonary lymphangitic carcinomatosis. Anticancer Res 36(8):4313–4320
Pellegrino S et al (2019) Total metabolic tumor volume by 18F-FDG PET/CT for the prediction of outcome in patients with non-small cell lung cancer. Ann Nucl Med 33(12):937–944
Wang D et al (2016) Prognostic value of baseline 18F-FDG PET/CT functional parameters in patients with advanced lung adenocarcinoma stratified by EGFR mutation status. PLoS ONE 11(6):e0158307
Seban RD et al (2020) FDG-PET biomarkers associated with long-term benefit from first-line immunotherapy in patients with advanced non-small cell lung cancer. Ann Nucl Med 34(12):968–974
Chin AL et al (2018) Prognostic value of pretreatment FDG-PET parameters in high-dose image-guided radiotherapy for oligometastatic non-small-cell lung cancer. Clin Lung Cancer 19(5):e581–e588
Olivier A et al (2014) Higher predictive value of tumour and node [18F]-FDG PET metabolic volume and TLG in advanced lung cancer under chemotherapy. Nucl Med Commun 35(9):908–915
Seban RD et al (2020) Baseline metabolic tumor burden on FDG PET/CT scans predicts outcome in advanced NSCLC patients treated with immune checkpoint inhibitors. Eur J Nucl Med Mol Imaging 47(5):1147–1157
Winther-Larsen A et al (2016) Metabolic tumor burden as marker of outcome in advanced EGFR wild-type NSCLC patients treated with erlotinib. Lung Cancer 94:81–87
Minamimoto R et al (2019) 18 F-FDG and 11 C-4DST PET/CT for evaluating response to platinum-based doublet chemotherapy in advanced non-small cell lung cancer: a prospective study. EJNMMI Res 9(1):4
Brodin NP et al (2021) Validating the SumMean. Pract Radiat Oncol 11(1):e46–e51
Andraos T et al (2020) Prognostic value of FDG-PET metrics for advanced NSCLC patients treated with first-line immunotherapy. IJROBP 108:e116–e117
Palma DA et al (2019) Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomised, phase 2, open-label trial. Lancet 393(10185):2051–2058
Gomez DR et al (2016) Local consolidative therapy versus maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer without progression after first-line systemic therapy: a multicentre, randomised, controlled, phase 2 study. Lancet Oncol 17(12):1672–1682
Iyengar P et al (2018) Consolidative radiotherapy for limited metastatic non-small-cell lung cancer: a phase 2 randomized clinical Trial. JAMA Oncol 4(1):e173501
Funding
This work was supported by RefleXion Medical, Inc. (Hayward, CA, USA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Berkowitz has no relevant financial or non-financial interests to disclose. Dr. Halmos is a consultant at AstraZeneca, Boehringer Ingelheim, Genentech/Roche, Pfizer, Lilly, Foundation Medicine, Guardant Health, Takeda, Novartis, Merck, Bristol-Myers Squibb, Spectrum Pharmaceuticals and TPT Therapeutics. Dr. Cheng is a consultant at AstraZeneca and Bayer, and she received research grants from Roche/Genentech, Spectrum Pharmaceuticals, and Vaccinex. Mr. Huntzinger is an employee at RefleXion Medical, where he also has stock and stock options. Dr. Ohri is a consultant at Merck and AstraZeneca.
Ethical approval
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Berkowitz, A.C., Halmos, B., Cheng, H. et al. FDG-PET metrics in advanced non-small cell lung cancer (NSCLC): a review and meta-analysis. Clin Transl Imaging 11, 381–387 (2023). https://doi.org/10.1007/s40336-023-00542-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-023-00542-y