Abstract
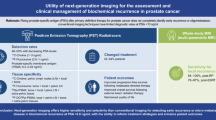
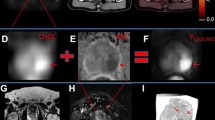
PET imaging represents an improvement in the diagnostic performance relative to conventional imaging, but several needs of the urologist are still unmet. The aim of this review is to identify limitations of currently available PET imaging and the resulting clinical consequences. Several relevant clinical settings of prostate cancer management where PET imaging is or could be used were identified. The current literature was then checked to match the currently reported performance based on PET imaging, with the clinical need to highlight current limitations. The most currently used tracers for prostate cancer are 18F-choline and 11C-choline, whereas other tracers such as Gallium-68 labeled prostate-specific membrane antigen (PSMA) and anti-1-amino-3-[18F]fluorocyclobutane-1-carboxylic acid are either experimental and/or not readily available. PET in the management of prostate cancer is of interest in any setting where cancer lesions should be identified, these are: search for the primary, initial staging, staging at recurrence and during treatment of metastatic disease. PET provides improved performance relative to conventional imaging but still has limitations. These are first associated to low quality and small studies including heterogeneous patients, making clear conclusions difficult. Moreover, there is lack of studies showing improved patient outcome and cost-effectiveness of pathways using PET. When it comes to specific clinical scenarios, PET has limited performance when used for the search of the primary or when used for the initial staging. Its most promising use is at the time point of biochemical recurrence. However, its performance at very early recurrences with low PSA levels remains limited. The use of PET needs to be explored for systemic treatment monitoring in metastatic patients. PET provides improved diagnostic performance relative to conventional imaging. Its most promising use is at the time point of biochemical recurrence after treatment with curative intent. In other clinical scenarios further improvements and research are necessary. It seems to be important to know the limitations of this imaging technology to truly improve the clinical decision making and to avoid waste of resources.
Similar content being viewed by others
References
Beauregard JM, Blouin AC, Fradet V, Caron A, Fradet Y, Lemay C et al (2015) FDG-PET/CT for pre-operative staging and prognostic stratification of patients with high-grade prostate cancer at biopsy. Cancer Imaging 15:2
Mottet N, Bellmunt J, Briers E, van den Bergh RCN, Bolla M, van Casteren NJ, Cornford P, Culine S, Joniau S, Lam T, Mason MD, Matveev V, van der Poel H, van der Kwast TH, Rouvière O, Wiegel T (2016) Guidelines on prostate cancer. European Association of Urology Web site. https://uroweb.org/guideline/prostate-cancer/. Accessed 17 May 2016
Evangelista L, Guttilla A, Zattoni F, Muzzio PC, Zattoni F (2013) Utility of choline positron emission tomography/computed tomography for lymph node involvement identification in intermediate- to high-risk prostate cancer: a systematic literature review and meta-analysis. Eur Urol 63(6):1040–1048
Evangelista L, Zattoni F, Guttilla A, Saladini G, Zattoni F, Colletti PM et al (2013) Choline PET or PET/CT and biochemical relapse of prostate cancer: a systematic review and meta-analysis. Clin Nucl Med 38(5):305–314
Passoni NM, Suardi N, Abdollah F, Picchio M, Giovacchini G, Messa C et al (2014) Utility of [11C]choline PET/CT in guiding lesion-targeted salvage therapies in patients with prostate cancer recurrence localized to a single lymph node at imaging: results from a pathologically validated series. Urol Oncol 32(1):38 e9–38 e16
Husarik DB, Miralbell R, Dubs M, John H, Giger OT, Gelet A et al (2008) Evaluation of [(18)F]-choline PET/CT for staging and restaging of prostate cancer. Eur J Nucl Med Mol Imaging 35(2):253–263
Rinnab L, Mottaghy FM, Blumstein NM, Reske SN, Hautmann RE, Hohl K et al (2007) Evaluation of [11C]-choline positron-emission/computed tomography in patients with increasing prostate-specific antigen levels after primary treatment for prostate cancer. BJU Int 100(4):786–793
Schilling D, Schlemmer HP, Wagner PH, Bottcher P, Merseburger AS, Aschoff P et al (2008) Histological verification of 11C-choline-positron emission/computed tomography-positive lymph nodes in patients with biochemical failure after treatment for localized prostate cancer. BJU Int 102(4):446–451
Incerti E, Fodor A, Mapelli P, Fiorino C, Alongi P, Kirienko M et al (2015) Radiation treatment of lymph node recurrence from prostate cancer: is 11C-choline PET/CT predictive of survival outcomes? J Nucl Med 56(12):1836–1842
Gerke O, Poulsen MH, Hoilund-Carlsen PF (2015) Added value of cost-utility analysis in simple diagnostic studies of accuracy: (18)F-fluoromethylcholine PET/CT in prostate cancer staging. Am J Nucl Med Mol Imaging 5(2):183–194
van Hove A, Savoie PH, Maurin C, Brunelle S, Gravis G, Salem N et al (2014) Comparison of image-guided targeted biopsies versus systematic randomized biopsies in the detection of prostate cancer: a systematic literature review of well-designed studies. World J Urol 32(4):847–858
Siddiqui MM, Rais-Bahrami S, Turkbey B, George AK, Rothwax J, Shakir N et al (2015) Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 313(4):390–397
Chan J, Syndikus I, Mahmood S, Bell L, Vinjamuri S (2015) Is choline PET useful for identifying intraprostatic tumour lesions? A literature review. Nucl Med Commun 36(9):871–880
Campos-Fernandes JL, Bastien L, Nicolaiew N, Robert G, Terry S, Vacherot F et al (2009) Prostate cancer detection rate in patients with repeated extended 21-sample needle biopsy. Eur Urol 55(3):600–606
Afshar-Oromieh A, Haberkorn U, Hadaschik B, Habl G, Eder M, Eisenhut M et al (2013) PET/MRI with a 68Ga-PSMA ligand for the detection of prostate cancer. Eur J Nucl Med Mol Imaging 40(10):1629–1630
Briganti A, Abdollah F, Nini A, Suardi N, Gallina A, Capitanio U et al (2012) Performance characteristics of computed tomography in detecting lymph node metastases in contemporary patients with prostate cancer treated with extended pelvic lymph node dissection. Eur Urol 61(6):1132–1138
Shen G, Deng H, Hu S, Jia Z (2014) Comparison of choline-PET/CT, MRI, SPECT, and bone scintigraphy in the diagnosis of bone metastases in patients with prostate cancer: a meta-analysis. Skeletal Radiol 43(11):1503–1513
Budiharto T, Joniau S, Lerut E, Van den Bergh L, Mottaghy F, Deroose CM et al (2011) Prospective evaluation of 11C-choline positron emission tomography/computed tomography and diffusion-weighted magnetic resonance imaging for the nodal staging of prostate cancer with a high risk of lymph node metastases. Eur Urol 60(1):125–130
Hellman S, Weichselbaum RR (1995) Oligometastases. J Clin Oncol 13(1):8–10
Suardi N, Gandaglia G, Gallina A, Di Trapani E, Scattoni V, Vizziello D et al (2015) Long-term outcomes of salvage lymph node dissection for clinically recurrent prostate cancer: results of a single-institution series with a minimum follow-up of 5 years. Eur Urol 67(2):299–309
Pound CR, Partin AW (2000) What does prostate-specific antigen recurrence mean? Curr Urol Rep 1(1):28–35
Coen JJ, Zietman AL, Thakral H, Shipley WU (2002) Radical radiation for localized prostate cancer: local persistence of disease results in a late wave of metastases. J Clin Oncol 20(15):3199–3205
Beresford MJ, Gillatt D, Benson RJ, Ajithkumar T (2010) A systematic review of the role of imaging before salvage radiotherapy for post-prostatectomy biochemical recurrence. Clin Oncol (R Coll Radiol) 22(1):46–55
Stephenson AJ, Scardino PT, Kattan MW, Pisansky TM, Slawin KM, Klein EA et al (2007) Predicting the outcome of salvage radiation therapy for recurrent prostate cancer after radical prostatectomy. J Clin Oncol 25(15):2035–2041
Chade DC, Shariat SF, Cronin AM, Savage CJ, Karnes RJ, Blute ML et al (2011) Salvage radical prostatectomy for radiation-recurrent prostate cancer: a multi-institutional collaboration. Eur Urol 60(2):205–210
Castellucci P, Ceci F, Graziani T, Schiavina R, Brunocilla E, Mazzarotto R et al (2014) Early biochemical relapse after radical prostatectomy: which prostate cancer patients may benefit from a restaging 11C-Choline PET/CT scan before salvage radiation therapy? J Nucl Med 55(9):1424–1429
Giovacchini G, Picchio M, Briganti A, Cozzarini C, Scattoni V, Salonia A et al (2010) [11C]choline positron emission tomography/computerized tomography to restage prostate cancer cases with biochemical failure after radical prostatectomy and no disease evidence on conventional imaging. J Urol 184(3):938–943
Giovacchini G, Picchio M, Scattoni V, Garcia Parra R, Briganti A, Gianolli L et al (2010) PSA doubling time for prediction of [(11)C]choline PET/CT findings in prostate cancer patients with biochemical failure after radical prostatectomy. Eur J Nucl Med Mol Imaging 37(6):1106–1116
Mitchell CR, Lowe VJ, Rangel LJ, Hung JC, Kwon ED, Karnes RJ (2013) Operational characteristics of (11)c-choline positron emission tomography/computerized tomography for prostate cancer with biochemical recurrence after initial treatment. J Urol 189(4):1308–1313
Rybalov M, Breeuwsma AJ, Leliveld AM, Pruim J, Dierckx RA, de Jong IJ (2013) Impact of total PSA, PSA doubling time and PSA velocity on detection rates of 11C-Choline positron emission tomography in recurrent prostate cancer. World J Urol 31(2):319–323
Wu LM, Xu JR, Gu HY, Hua J, Zhu J, Chen J et al (2013) Role of magnetic resonance imaging in the detection of local prostate cancer recurrence after external beam radiotherapy and radical prostatectomy. Clin Oncol (R Coll Radiol) 25(4):252–264
Lecouvet FE, Simon M, Tombal B, Jamart J, Vande Berg BC, Simoni P (2010) Whole-body MRI (WB-MRI) versus axial skeleton MRI (AS-MRI) to detect and measure bone metastases in prostate cancer (PCa). Eur Radiol 20(12):2973–2982
Imbriaco M, Larson SM, Yeung HW, Mawlawi OR, Erdi Y, Venkatraman ES et al (1998) A new parameter for measuring metastatic bone involvement by prostate cancer: the Bone Scan Index. Clin Cancer Res 4(7):1765–1772
Tombal B, Rezazadeh A, Therasse P, Van Cangh PJ, Vande Berg B, Lecouvet FE (2005) Magnetic resonance imaging of the axial skeleton enables objective measurement of tumor response on prostate cancer bone metastases. Prostate 65(2):178–187
Wibmer AG, Burger IA, Sala E, Hricak H, Weber WA, Vargas HA (2016) Molecular imaging of prostate cancer. Radiographics 36(1):142–159
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any conflict of interest to declare.
Ethical standards statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Walz, J., Pignot, G., Salem, N. et al. The urologist’s unmet clinical needs in prostate cancer. Clin Transl Imaging 4, 433–438 (2016). https://doi.org/10.1007/s40336-016-0199-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-016-0199-2