Abstract
Introduction
Hypertension (HTN) is a co-morbidity that is commonly associated with heart failure with preserved ejection fraction (HFpEF). However, it remains unclear whether treatment of hypertension in HFpEF patients is associated with improved cardiovascular outcomes.
Aim
The purpose of this meta-analysis is to evaluate the association of anti-hypertensive medical therapy with cardiovascular outcomes in patients with HFpEF.
Methods
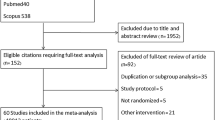
We performed a database search for studies reporting on the association of anti-hypertensive medications with cardiovascular outcomes and safety endpoints in patients with HFpEF. The databases searched include OVID Medline, Web of Science, and Embase. The primary endpoint was all-cause mortality. Secondary endpoints include cardiovascular (CV) mortality, worsening heart failure (HF), CV hospitalization, composite major adverse cardiovascular events (MACE), hyperkalemia, worsening renal function, and hypotension.
Results
A total of 12 studies with 14062 HFpEF participants (7010 treated with medical therapy versus 7052 treated with placebo) met inclusion criteria. Use of anti-hypertensive medications was not associated with lower all-cause mortality, CV mortality or CV hospitalization compared to treatment with placebo (OR 1.02, 95% CI 0.77–1.35; p = 0.9, OR 0.88, 95% CI 0.73–1.06; p = 0.19, OR 0.99, 95% CI 0.87–1.12; p = 0.83, OR 0.90, 95% CI 0.79–1.03; p = 0.11). Anti-hypertensive medications were not associated with lower risk of subsequent acute myocardial infarction (AMI) (OR 0.53, 95% CI 0.07–3.73; p = 0.5). Use of anti-hypertensive medications was associated with a statistically significant lower risk of MACE (OR 0.90, 95% CI 0.83–0.98; p = 0.02).
Conclusions
While treatment with anti-hypertensive medications was not associated with lower risk of all-cause mortality, their use may be associated with reduce risk of adverse cardiovascular outcomes in patients with HFpEF regardless of whether they have HTN. Additional high quality studies are required to clarify this association and determine the effect based on specific classes of medications.













Similar content being viewed by others
References
Ashley EA, Niebauer J. Cardiology explained. Remedica Copyright © 2004, Remedica.: London; 2004.
Tackling G, Borhade MB. Hypertensive Heart Disease, in StatPearls. StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC.: Treasure Island (FL); 2023. Ineligible companies. Disclosure: Mahesh Borhade declares no relevant financial relationships with ineligible companies.
Gazewood JD, Turner PL. Heart failure with preserved ejection fraction: diagnosis and management. Am Fam Physician. 2017;96(9):582–8.
Chobanian AV, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–71.
Levy D, et al. The progression from hypertension to congestive heart failure. JAMA. 1996;275(20):1557–62.
Vasan RS, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med. 2001;345(18):1291–7.
Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC Jr, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–16.
Heidenreich PA, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2022;145(18):e895–1032.
Verdecchia P, et al. Left ventricular mass and cardiovascular morbidity in essential hypertension: the MAVI study. J Am Coll Cardiol. 2001;38(7):1829–35.
Levy D, et al. Prognostic implications of baseline electrocardiographic features and their serial changes in subjects with left ventricular hypertrophy. Circulation. 1994;90(4):1786–93.
Devereux RB, et al. Regression of hypertensive left ventricular hypertrophy by losartan compared with atenolol: the Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial. Circulation. 2004;110(11):1456–62.
Dahlöf B, Pennert K, Hansson L. Reversal of left ventricular hypertrophy in hypertensive patients: a metaanalysis of 109 treatment studies. Oxford: Oxford University Press; 1992.
Klingbeil AU, et al. A meta-analysis of the effects of treatment on left ventricular mass in essential hypertension. Am J Med. 2003;115(1):41–6.
Ruilope LM, Schmieder RE. Left ventricular hypertrophy and clinical outcomes in hypertensive patients. Am J Hypertens. 2008;21(5):500–8.
Massie BM, et al. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359(23):2456–67.
Yusuf S, et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet. 2003;362(9386):777–81.
Hernandez AF, et al. Clinical effectiveness of beta-blockers in heart failure: findings from the OPTIMIZE-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure) Registry. J Am Coll Cardiol. 2009;53(2):184–92.
Pitt B, et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med. 2014;370(15):1383–92.
Solomon SD, et al. Angiotensin–neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med. 2019;381(17):1609–20.
Lund LH, et al. Heart failure with mid-range ejection fraction in CHARM: characteristics, outcomes and effect of candesartan across the entire ejection fraction spectrum. Eur J Heart Fail. 2018;20(8):1230–9.
Butler J, Anker SD, Packer M. Redefining heart failure with a reduced ejection fraction. JAMA. 2019;322(18):1761–2.
Pascual-Figal DA, et al. Mid-range left ventricular ejection fraction: clinical profile and cause of death in ambulatory patients with chronic heart failure. Int J Cardiol. 2017;240:265–70.
Paulus WJ, Tschöpe C. A novel paradigm for heart failure with preserved ejection fraction: comorbidities drive myocardial dysfunction and remodeling through coronary microvascular endothelial inflammation. J Am Coll Cardiol. 2013;62(4):263–71.
van Heerebeek L, et al. Low myocardial protein kinase G activity in heart failure with preserved ejection fraction. Circulation. 2012;126(7):830–9.
Anker SD, et al. Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med. 2021;385(16):1451–61.
Pandey AK, et al. Mechanisms of benefits of sodium-glucose cotransporter 2 inhibitors in heart failure with preserved ejection fraction. Eur Heart J. 2023;44(37):3640–51.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
The authors report no relevant conflicts of interest.
Compliance with ethical standards (guidelines statement)
The systematic review was conducted with a protocol in accordance with the Preferred Reporting of Items for Systematic reviews and Meta-Analyses (PRISMA) statement.
Ethical approval
The study is a systematic review and meta-analysis; no ethical approval was required.
Data availability
Not applicable.
Rights and permissions
About this article
Cite this article
Al-Sadawi, M., Tao, M., Dhaliwal, S. et al. Safety and Efficacy of Anti-Hypertensive Medications in Patients with Heart Failure with Preserved Ejection Fraction: A Systematic Review and Meta-analysis. High Blood Press Cardiovasc Prev (2024). https://doi.org/10.1007/s40292-024-00646-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40292-024-00646-0