Abstract
Introduction
A family history of hypertension puts young adults at a higher risk of developing hypertension, that too, at an earlier age than their parents. Recent studies suggest that the baroreflex mechanism, which takes care of the short-term regulation of blood pressure (BP), also plays a role in the long-term regulation of BP. Studies have reported decreased baroreflex sensitivity (BRS) in hypertensives. Reduced BRS is shown to herald the future occurrence of cardiovascular diseases (CVD) and helps in risk stratification
Aim
To assess BRS at rest and during the Valsalva maneuver among apparently healthy male offspring (age 18–35 years) of hypertensive patients.
Methods
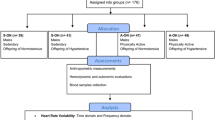
We recruited 37 participants whose parents (either/both) were hypertensive in the study group and whose parents (both) were not hypertensive in the control group. We measured basic anthropometric parameters (height, weight, waist circumference), cardiovascular parameters (heart rate and BP), short-term heart rate variability, and BRS (at rest and during Valsalva).
Results
We found that BRS at rest and BRS during the Valsalva maneuver were reduced among healthy male offspring of hypertensive parents than in healthy male offspring of non-hypertensive parents. Further, HRV indices and Valsalva ratio showed a sympathovagal imbalance in the form of decreased vagal and increased sympathetic activity.
Conclusion
The reduced BRS and sympathovagal imbalance in male offspring of hypertensive parents reveal the early risk of developing hypertension in the future.
Similar content being viewed by others
Availability of data and material
Data could be made available upon reasonable request to the corresponding author.
References
Ramakrishanan S, Gupta K. Prevalence of hypertension among Indian adults: results from the great India blood pressure survey. Indian Heart J. 2020;72:217.
Pal GK, Pal P, Nanda N, Lalitha V, Dutta TK, Adithan C. Sympathovagal imbalance in prehypertensive offspring of two parents versus one parent hypertensive. Int J Hypertens. 2011;23:2011.
Kougias P, Weakley SM, Yao Q, Lin PH, Chen C. Arterial baroreceptors in the management of systemic hypertension. Med Sci Monit. 2010;16:RA1.
Čelovská D, Staško J, Gonsorcík J, Diab A. The significance of baroreflex sensitivity in hypertensive subjects with stroke. Physiol Res. 2010;59:537–43.
Honzíková N, Fišer B. Baroreflex sensitivity and essential hypertension in adolescents. Physiol Res. 2009;58:605–12.
Bristow JD, Honour AJ, Pickering GW, Sleight P, Smyth HS. Diminished baroreflex sensitivity in high blood pressure. Circulation. 1969;39:48–54.
Parati G. Arterial baroreflex control of heart rate: determining factors and methods to assess its spontaneous modulation. J Physiol. 2005;565:706–7.
La Rovere MT. Baroreflex sensitivity as a new marker for risk stratification. Z Kardiol. 2000;89(3):44–50.
Matthews EL, Sebzda KN, Wenner MM. Altered baroreflex sensitivity in young women with a family history of hypertension. J Neurophysiol. 2019;121:1011–7.
Iorga A, Cunningham CM, Moazeni S, Ruffenach G, Umar S, Eghbali M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol Sex Differ. 2017;8:33.
Swenne CA. Baroreflex sensitivity: mechanisms and measurement. Neth Heart J. 2013;21:58–60.
La Rovere MT, Pinna GD, Raczak G. Baroreflex sensitivity: measurement and clinical implications. Ann Noninvasive Electrocardiol. 2008;13:191–207.
Yang H, Carter JR. Baroreflex sensitivity analysis: spontaneous methodology vs. Valsalva’s maneuver. Clin Auton Res. 2013;23:133–9.
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, Pratt M, Ekelund U, Yngve A, Sallis JF, Oja P. International physical activity questionnaire: 12-Country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95.
James WPT, Chunming C, Inoue S. Appropriate Asian body mass indices? Obes Rev. 2002;3:139.
Penáz J, Voigt A, Teichmann W. Beitrag zur fortlaufenden indirekten Blutdruckmessung [Contribution to the continuous indirect blood pressure measurement]. Z Gesamte Inn Med. 1976;31(24):1030–3.
Wesseling KH. Physiocal, calibrating finger vascular physiology for Finapres. Homeostasis. 1995;36:67–82.
Guelen I, Westerhof BE, van der Sar GL, van Montfrans GA, Kiemeneij F, Wesseling KH, Bos WJ. Validation of brachial artery pressure reconstruction from finger arterial pressure. J Hypertens. 2008;26:1321–7.
Demirel S, Attigah N, Bruijnen H, Macek L, Hakimi M, Able T, Böckler D. Changes in baroreceptor sensitivity after eversion carotid endarterectomy. J Vasc Surg. 2012;55:1322–8.
Westerhof BE, Gisolf J, Stok WJ, Wesseling AKH, Karemaker JM. Time-domain cross-correlation baroreflex sensitivity: performance on the EUROBAVAR data set. J Hypertens. 2004;22:1371–80.
Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, Prabhakaran D. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens. 2014;32:1170–7.
Gupta R, Xavier D. Hypertension: the most important non communicable disease risk factor in India. Indian Heart J. 2018;70:565–72.
Deng AY. Genetic basis of polygenic hypertension. Hum Mol Genet. 2007;16(R2):R195–202.
Mussalo H, Vanninen E, Ikäheimo R, Laitinen T, Laakso M, Länsimies E, Hartikainen J. Baroreflex sensitivity in essential and secondary hypertension. Clin Auton Res. 2002;12:465–71.
Cherfan M, Vallée A, Kab S, Salameh P, Goldberg M, Zins M, Blacher J. Unhealthy behaviors and risk of uncontrolled hypertension among treated individuals—the CONSTANCES population-based study. Sci Rep. 2020;10.
Javorka M, Zila I, Balhárek T, Javorka K. Heart rate recovery after exercise: relations to heart rate variability and complexity. Braz J Med Biol Res. 2002;35:991–1000.
Laborde S, Mosley E, Thayer JF. Heart rate variability and cardiac vagal tone in psychophysiological research—recommendations for experiment planning, data analysis, and data reporting. Front Psychol. 2017;8:213.
Malpas SC. Sympathetic nervous system overactivity and its role in the development of cardiovascular disease. Physiol Rev. 2010;90:513–57.
Electrophysiology TF. Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Circulation. 1996;93(5):1043–65.
Mathias C, Bannister R. Investigation of autonomic disorders. In: Mathias C, Bannister R, editors. Auton Fail Textb Clin Disord Auton Nerv Syst. 4th ed. Great Britain: Oxford University Press; 1999. p. 169–95.
Farah BQ, do Prado WL, dos Tenório TRS, Ritti-Dias RM. Heart rate variability and its relationship with central and general obesity in obese normotensive adolescents. Einstein (Sao Paulo). 2013;11:285–90.
Li CH, Sun ZJ, Lu FH, Chou YT, Yang YC, Chang CJ, Wu JS. Epidemiological evidence of increased waist circumference, but not body mass index, associated with impaired baroreflex sensitivity. Obes Res Clin Pract. 2020;14:158–63.
Huang CC, Lai YR, Lien CY, Benz C, Kung CT, Chiang YF, Lu CH. Effectiveness of different methods for baroreflex sensitivity assessment in determining the severity of cardiovascular autonomic neuropathy in patients with Parkinson’s disease. Front Neurosci. 2022;25:86.
Eguchi K, Tomizawa H, Ishikawa J, Hoshide S, Pickering TG, Shimada K, Kario K. Factors associated with baroreflex sensitivity: association with morning blood pressure. Hypertens Res. 2007;30:723–8.
Acknowledgements
The authors are thankful to all the participants who took part in the study, and we thank the Indian Council of Medical Research for approving our project under short term studentship 2020 (Reference ID: 2020-06494).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research funding
None declared.
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Human and animal rights statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards Informed consent was obtained from all individuals included in this study. The study was commenced after getting approval from the Institutional Ethics committee (Human) (JIP/IEC/2020/236).
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chandrasekaran, P., Kuppusamy, S., Subramanian, S.K. et al. Altered baroreflex sensitivity at rest and during Valsalva maneuver in healthy male offspring of hypertensive patients. High Blood Press Cardiovasc Prev 30, 73–81 (2023). https://doi.org/10.1007/s40292-023-00559-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-023-00559-4