Abstract
Introduction
An impact of the sympathetic nervous system in the higher rate of cardiovascular events in the early morning compared to the evening has been claimed. Augmented sympathetic vasoconstriction increases cardiovascular risk by augmenting pulse pressure and cardiac afterload. Type 2 diabetes (T2DM) further increases sympathetic neurovascular transduction and cardiovascular risk.
Aim
We assessed whether peripheral vasoconstriction triggered by a standardized sympathetic stressor is augmented at 6am vs 9pm in adults between 50–80 years with type 2 diabetes (T2DM50-80) vs healthy ones (H50-80).
Methods
Mean values of sympathetic vasoconstrictor responsiveness (SVR), vascular conductance (VC), brachial artery blood flow, and mean arterial pressure were measured on the contralateral forearm over two 5-minute bouts of rest and handgrip-mediated sympathetic stimulation, respectively.
Results
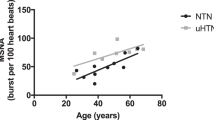
Although baseline VC values were lower (p < 0.01) in the morning vs evening in both groups, SVR values in response to sympathoexcitation were similar in H50-80 (− 0.43 ± 12.44 vs − 2.57 ± 11.63 %, p = 0.73) and T2DM50-80 (+6.64 ± 10.67 vs +5.21 ± 7.64 %, p = 0.90), but higher (p < 0.01) in T2DM50-80 vs H50-80 at both day hours. Individuals with T2DM reported positive SVR values and VC change-scores, while healthy individuals reported statistically different (p < 0.02) negative SVR values and VC change-scores.
Conclusion
Peripheral vasoconstriction triggered by a standardized sympathetic stressor is similar between morning and evening, regardless of T2DM and different baseline VC values. However, peripheral vasoconstriction responsiveness is blunted in individuals with T2DM as handgrip-mediated sympathoexcitation induces vasodilation in the contralateral forearm in adults with T2DM and vasoconstriction in healthy age-matched controls, highlighting a neurovascular response altered by T2DM.


Similar content being viewed by others
Reference
Elliott WJ. Cyclic and circadian variations in cardiovascular events. Am J Hypertens. 2001;14:291S-295S. https://doi.org/10.1016/S0895-7061(01)02174-4.
Atkinson G, Jones H, Ainslie PN. Circadian variation in the circulatory responses to exercise: Relevance to the morning peaks in strokes and cardiac events. Eur J Appl Physiol. 2010;108:15–29. https://doi.org/10.1007/s00421-009-1243-y.
Gentilin A, Moghetti P, Cevese A, Mattioli AV, Schena F, Tarperi C. Circadian and sex differences in carotid-femoral pulse wave velocity in young individuals and elderly with and without type 2 diabetes. Front Cardiovasc Med. 2022;9:952621. https://doi.org/10.3389/FCVM.2022.952621.
Muller JE, Tofler GH, Verrier RL. Sympathetic activity as the cause of the morning increase in cardiac events. A likely culprit, but the evidence remains circumstantial. Circulation. 1995;91:2508–9. https://doi.org/10.1161/01.CIR.91.10.2508.
Del Pinto R, Grassi G, Ferri C, Pengo MF, Lombardi C, Pucci G, et al. Diagnostic and therapeutic approach to sleep disorders, high blood pressure and cardiovascular diseases: a consensus document by the Italian Society of Hypertension (SIIA). High Blood Press Cardiovasc Prev. 2021;28:85–102. https://doi.org/10.1007/S40292-021-00436-Y.
Panza JA, Epstein SE, Quyyumi AA. Circadian variation in vascular tone and its relation to alpha-sympathetic vasoconstrictor activity. N Engl J Med. 1991;325:986–90. https://doi.org/10.1056/NEJM199110033251402.
Otto ME, Svatikova A, De Mattos Barretto RB, Santos S, Hoffmann M, Khandheria B, et al. Early morning attenuation of endothelial function in healthy humans. Circulation. 2004;109:2507–10. https://doi.org/10.1161/01.CIR.0000128207.26863.C4.
Somers VK, Dyken ME, Mark AL, Abboud FM. Sympathetic-nerve activity during sleep in normal subjects. N Engl J Med. 1993;328:303–7. https://doi.org/10.1056/NEJM199302043280502.
Dyson KS, Shoemaker JK, Hughson RL. Effect of acute sympathetic nervous system activation on flow-mediated dilation of brachial artery. Am J Physiol - Hear Circ Physiol. 2006;290:H1446–53. https://doi.org/10.1152/ajpheart.00771.2005.
Gentilin A, Moghetti P, Cevese A, Schena F, Tarperi C. Sympathetic-mediated blunting of forearm vasodilation is similar between young men and women. Biol Sex Differ. 2022;13:33. https://doi.org/10.1186/S13293-022-00444-0.
Kollias GE, Stamatelopoulos KS, Papaioannou TG, Zakopoulos NA, Alevizaki M, Alexopoulos GP, et al. Diurnal variation of endothelial function and arterial stiffness in hypertension. J Hum Hypertens. 2009;23:597–604. https://doi.org/10.1038/JHH.2009.2.
Gentilin A, Tarperi C, Skroce K, Cevese A, Schena F. Effect of acute sympathetic activation on leg vasodilation before and after endurance exercise. J Smooth Muscle Res. 2021;57:53–67. https://doi.org/10.1540/JSMR.57.
Chen L, Yang G. Recent advances in circadian rhythms in cardiovascular system. Front Pharmacol. 2015;6:71. https://doi.org/10.3389/FPHAR.2015.00071.
Wu H, Norton V, Cui K, Zhu B, Bhattacharjee S, Lu YW, et al. Diabetes and Its Cardiovascular Complications: Comprehensive Network and Systematic Analyses. Front Cardiovasc Med. 2022;9:841928. https://doi.org/10.3389/FCVM.2022.841928.
Schiavoni M, Cosentino F, Camici GG, Luescher TF. Diabetes and endothelial dysfunction: What’s the culprit? High Blood Press Cardiovasc Prev. 2007;14:5–10. https://doi.org/10.2165/00151642-200714010-00002/FIGURES/3.
Wang Y, Jiang W, Chen H, Zhou H, Liu Z, Liu Z, et al. Sympathetic nervous system mediates cardiac remodeling after myocardial infarction in a circadian disruption model. Front Cardiovasc Med. 2021;8:668387. https://doi.org/10.3389/FCVM.2021.668387.
Emdin M. Autonomic nervous system in diabetes. Ital Hear J Suppl. 2001;2:857–62.
Young BE, Holwerda SW, Vranish JR, Keller DM, Fadel PJ. Sympathetic Transduction in Type 2 Diabetes Mellitus. Hypertens (Dallas, Tex 1979). 2019;74:201–7. https://doi.org/10.1161/HYPERTENSIONAHA.119.12928.
Buckwalter JB, Clifford PS. The paradox of sympathetic vasoconstriction in exercising skeletal muscle. Exerc Sport Sci Rev. 2001;29:159–63. https://doi.org/10.1097/00003677-200110000-00005.
Thomas GD, Segal SS. Neural control of muscle blood flow during exercise. J Appl Physiol. 2004;97:731–8. https://doi.org/10.1152/japplphysiol.00076.2004.
Cosentino F, Grant PJ, Aboyans V, Bailey CJ, Ceriello A, Delgado V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2020;41:255–323. https://doi.org/10.1093/EURHEARTJ/EHZ486.
Cheshire WP, Freeman R, Gibbons CH, Cortelli P, Wenning GK, Hilz MJ, et al. Electrodiagnostic assessment of the autonomic nervous system: A consensus statement endorsed by the American Autonomic Society, American Academy of Neurology, and the International Federation of Clinical Neurophysiology. Clin Neurophysiol. 2021;132:666–82. https://doi.org/10.1016/J.CLINPH.2020.11.024.
Michikami D, Kamiya A, Fu Q, Niimi Y, Iwase S, Mano T, et al. Forearm elevation augments sympathetic activation during handgrip exercise in humans. Clin Sci. 2002;103:295–301. https://doi.org/10.1042/cs1030295.
Saito M, Mano T, Abe H, Iwase S. Responses in muscle sympathetic nerve activity to sustained hand-grips of different tensions in humans. Eur J Appl Physiol Occup Physiol. 1986;55:493–8. https://doi.org/10.1007/BF00421643.
Saito M, Mano T, Iwase S. Changes in muscle sympathetic nerve activity and calf blood flow during static handgrip exercise. Eur J Appl Physiol Occup Physiol. 1990;60:277–81. https://doi.org/10.1007/BF00379396.
Kaijser L. Neurogenic forearm vasodilatation during contralateral isometric exercise is attenuated in diabetes mellitus. Clin Auton Res. 1991;1:239–42. https://doi.org/10.1007/BF01824993.
Jacobsen TN, Hansen J, Nielsen HV, Wildschiødtz G, Kassis E, Larsen B, et al. Skeletal muscle vascular responses in human limbs to isometric handgrip. Eur J Appl Physiol Occup Physiol. 1994;69:147–53. https://doi.org/10.1007/BF00609407.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
None declared.
Ethical Statement
The study was approved by the Ethics Board of the University of Verona (3293CESC) and conducted following the declaration of Helsinki. Informed oral and written consent was obtained from all participants before starting any test.
Funding
None declared.
Data Availability
The data are available from the corresponding author on reasonable request.
Authors’ contributions
Study concept and design (AG); subject recruitment, data acquisition and analysis (AG); formal analysis and investigation (AG); data interpretation (AG, AC, PM, AVM, FS, CT); original draft preparation (AG); review and critical revision of the manuscript (AG, AC, PM, AVM, FS, CT); all authors read and approved the final version of this manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gentilin, A., Moghetti, P., Cevese, A. et al. Circadian Variations in Sympathetic Vasoconstriction in Older Adults with and Without Type 2 Diabetes. High Blood Press Cardiovasc Prev 30, 55–62 (2023). https://doi.org/10.1007/s40292-022-00557-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40292-022-00557-y