Abstract
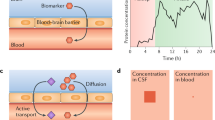
Biomarkers in Alzheimer’s disease (AD) have the potential to allow early and more accurate diagnosis, predict disease progression, stratify individuals and track response to candidate therapies in drug trials. The first fluid biomarkers reflecting aspects of AD neuropathology were identified in cerebrospinal fluid (CSF) in the 1990s. Three CSF biomarkers (amyloid-β 1–42, total tau and phospho-tau) have consistently been shown to have diagnostic utility and are incorporated into the new diagnostic criteria for AD. These markers have also been shown in longitudinal studies to predict conversion of mild cognitive impairment to AD. However, a key issue with the use of CSF biomarkers as a screening test is the invasiveness of lumbar puncture. Over the last 20 years there has been an active quest for blood biomarkers, which could be easily acquired and tested repeatedly throughout the disease course. One approach to identifying such markers is to attempt to measure candidates that have already been identified in CSF. Until recently, this approach has been limited by assay sensitivity, but newer platforms now allow single molecule-level detection. Another approach is identification of candidates in large multiplex panels that allow for multiple analytes to be quantified in parallel. While both approaches show promise, to date no blood-based biomarker or combination of biomarkers has sufficient predictive value to have utility in clinical practice. In this review, an overview of promising blood protein candidates is provided, and the challenges of validating and converting these into practicable tests are discussed.
Similar content being viewed by others
References
Dubois B, Feldman HH, Jacova C, et al. Advancing research diagnostic criteria for Alzheimer’s disease: the IWG-2 criteria. Lancet Neurol. 2014;13(6):614–29.
Motter R, Vigo-Pelfrey C, Kholodenko D, et al. Reduction of beta-amyloid peptide42 in the cerebrospinal fluid of patients with Alzheimer’s disease. Ann Neurol. 1995;38:643–8.
Vandermeeren M, Mercken M, Vanmechelen E, et al. Detection of tau proteins in normal and Alzheimer’s disease cerebrospinal fluid with a sensitive sandwich enzyme-linked immunosorbent assay. J Neurochem. 1993;61:1828–34.
Vanmechelen E, Vanderstichele H, Davidsson P, et al. Quantification of tau phosphorylated at threonine 181 in human cerebrospinal fluid: a sandwich ELISA with a synthetic phosphopeptide for standardization. Neurosci Lett. 2000;285:49–52.
Sunderland T, Linker G, Mirza N, et al. Decreased beta- amyloid 1–42 and increased tau levels in cerebrospinal fluid of patients with Alzheimer’s disease. JAMA. 2003;289:2094–103.
Tapiola T, Alafuzoff I, Herukka SK, et al. Cerebrospinal fluid [beta]-amyloid 42 and tau proteins as biomarker changes in the brain. Arch Neurol. 2009;66:382–9.
Shaw LM, Vanderstichele H, Knapik-Czajka M, Alzheimer’s Disease Neuroimaging Initiative, et al. Cerebrospinal fluid biomarker signature in Alzheimer’s disease neuroimaging initiative subjects. Ann Neurol. 2009;65:403–13.
Visser PJ, Verhey F, Knol DL, et al. Prevalence and prognostic value of cerebrospinal fluid markers of Alzheimer pathology in subjects with subjective cognitive impairment and mild cognitive impairment. The DeSCRIPA study. Lancet Neurol. 2009;8:619–27.
Mattsson N, Zetterberg H, Hansson O, et al. CSF bio- markers and incipient Alzheimer disease in patients with mild cognitive impairment. JAMA. 2009;302:385–93.
Jack CR Jr, Albert MS, Knopman DS, et al. Introduction to the recommendations from the National Institute on Aging—Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):257–62.
McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging—Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263–9.
Albert MS, DeKosky ST, Dickson D, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging—Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):270–9.
Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging—Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):280–92.
Alzforum. Alzbiomarker [web-based resource]. Alzheimer’s disease vs control: neurogranin (CSF). http://www.alzforum.org/alzbiomarker/meta-analysis/alzheimers-disease-vs-control-neurogranin-csf. Accessed 30 May 2016.
Alzforum. Alzbiomarker [web-based resource]. MCI-AD vs MCI-stable: neurogranin (CSF). http://www.alzforum.org/alzbiomarker/meta-analysis/mci-ad-vs-mci-stable-neurogranin-csf. Accessed 30 May 2016.
Alzforum. Alzbiomarker [web-based resource]. Alzheimer’s disease vs control: hFABP (CSF). http://www.alzforum.org/alzbiomarker/meta-analysis/alzheimers-disease-vs-control-hfabp-csf. Accessed 30 May 2016.
Alzforum. Alzbiomarker [web-based resource]. Alzheimer’s disease vs control: NSE (CSF). http://www.alzforum.org/alzbiomarker/meta-analysis/alzheimers-disease-vs-control-nse-csf. Accessed 30 May 2016.
Alzforum. Alzbiomarker [web-based resource]. Alzheimer’s disease vs control: NFL (CSF). http://www.alzforum.org/alzbiomarker/meta-analysis/alzheimers-disease-vs-control-nfl-csf. Accessed 30 May 2016.
Alzforum. Alzbiomarker [web-based resource]. Alzheimer’s disease vs control: YKL-40 (CSF)]. http://www.alzforum.org/alzbiomarker/meta-analysis/alzheimers-disease-vs-control-ykl-40-csf. Accessed 30 May 2016.
Alzforum. Alzbiomarker [web-based resource]. Alzheimer’s disease vs control: VLP-1 (CSF). http://www.alzforum.org/alzbiomarker/meta-analysis/alzheimers-disease-vs-control-vlp-1-csf. Accessed 30 May 2016.
Wellington H, Paterson RW, Portelius E, et al. Increased CSF neurogranin concentration is specific to Alzheimer disease. Neurology. 2016;86(9):829–35.
Paterson RW, Toombs J, Slattery CF, et al. Dissecting IWG-2 typical and atypical Alzheimer’s disease: insights from cerebrospinal fluid analysis. J Neurol. 2015;262(12):2722–30.
Kroksveen AC, Opsahl JA, Aye TT, et al. Proteomics of human cerebrospinal fluid: discovery and verification of biomarker candidates in neurodegenerative diseases using quantitative proteomics. J Proteomics. 2011;74(4):371–88.
Wildsmith KR, Schauer SP, Smith AM, et al. Identification of longitudinally dynamic biomarkers in Alzheimer’s disease cerebrospinal fluid by targeted proteomics. Mol Neurodegener. 2014;9:22.
Heywood WE, Galimberti D, Bliss E, et al. Identification of novel CSF biomarkers for neurodegeneration and their validation by a high-throughput multiplexed targeted proteomic assay. Mol Neurodegener. 2015;10:64.
Toledo JB, Vanderstichele H, Figurski M, et al. Alzheimer’s disease neuroimaging initiative: factors affecting Abeta plasma levels and their utility as biomarkers in ADNI. Acta Neuropathol. 2011;122:401–13.
Huang Y, Potter R, Sigurdson W, et al. Beta-amyloid dynamics in human plasma. Arch Neurol. 2012;69:1591–7.
Le Bastard N, Aerts L, Leurs J, et al. No correlation between time-linked plasma and CSF Abeta levels. Neurochem Int. 2009;55:820–825.
Hansson O, Zetterberg H, Vanmechelen E, et al. Evaluation of plasma Abeta[40] and Abeta[42] as predictors of conversion to Alzheimer’s disease in patients with mild cognitive impairment. Neurobiol Aging. 2010;31:357–67.
Devanand DP, Schupf N, Stern Y, et al. Plasma Abeta and PET PiB binding are inversely related in mild cognitive impairment. Neurology. 2011;77:125–131.
Lui JK, Laws SM, Li QX, AIBL Research Group, et al. Plasma amyloid-beta as a biomarker in Alzheimer’s disease: the AIBL study of aging. J Alzheimers Dis. 2010;20:1233–42.
Figurski MJ, Waligorska T, Toledo J, et al. Improved protocol for measurement of plasma beta-amyloid in longitudinal evaluation of Alzheimer’s Disease Neuroimaging Initiative study patients. Alzheimers Dement. 2012;8:250–60.
Olsson B, Lautner R, Andreasson U, et al. CSF and blood biomarkers for the diagnosis of Alzheimer’s disease: a systematic review and meta-analysis. Lancet Neurol. 2016;15(7):673–84.
Alzforum. Alzbiomarker [web-based resource]. http://www.alzforum.org/alzbiomarker. Accessed 9 May 2016.
Sparks DL, Kryscio RJ, Sabbagh MN, et al. Tau is reduced in AD plasma and validation of employed ELISA methods. Am J Neurodegener Dis. 2012;1(1):99–106.
Wang T, Xiao S, Liu Y, et al. The efficacy of plasma biomarkers in early diagnosis of Alzheimer’s disease. Int J Geriatr Psychiatry. 2014;29(7):713–9.
Chiu MJ, Yang SY, Horng HE, et al. Combined plasma biomarkers for diagnosing mild cognition impairment and Alzheimer’s disease. ACS Chem Neurosci. 2013;4(12):1530–6.
Chiu MJ, Chen YF, Chen TF, et al. Plasma tau as a window to the brain-negative associations with brain volume and memory function in mild cognitive impairment and early Alzheimer’s disease. Hum Brain Mapp. 2014;35(7):3132–42.
Zetterberg H, Wilson D, Andreasson U, et al. Plasma tau levels in Alzheimer’s disease. Alzheimers Res Ther. 2013;5(2):9.
Wilson DH, Rissin DM, Kan CW, et al. The Simoa HD-1 analyzer: a novel fully automated digital immunoassay analyzer with single-molecule sensitivity and multiplexing. J Lab Autom. 2016;21(4):533–47.
Janelidze S, Stomrud E, Palmqvist S, et al. Plasma β-amyloid in Alzheimer’s disease and vascular disease. Sci Reports 2016;6:26801. doi:10.1038/srep26801.
Dage JL, Wennberg AMV, Airey DC, et al. Levels of tau protein in plasma are associated with neurodegeneration and cognitive function in a population based elderly cohort. Neurology. 2016. doi:10.1016/j.jalz.2016.06.001.
Neselius S, Zetterberg H, Blennow K, et al. Olympic boxing is associated with elevated levels of the neuronal protein tau in plasma. Brain Inj. 2013;27(4):425–33.
de Jong D, Jansen RW, Pijnenburg YA, et al. CSF neurofilament proteins in the differential diagnosis of dementia. J Neurol Neurosurg Psychiatry. 2007;78(9):936–8.
Scherling CS, Hall T, Berisha F, et al. Cerebrospinal fluid neurofilament concentration reflects disease severity in frontotemporal degeneration. Ann Neurol. 2014;75(1):116–26.
Wilke C, Preische O, Deuschle C, et al. Neurofilament light chain in FTD is elevated not only in cerebrospinal fluid, but also in serum. J Neurol Neurosurg Psychiatry. 2016. doi:10.1136/jnnp-2015-312972.
Rohrer JD, Woollacott IOC, Dick KM, et al. Serum neurofilament light chain protein is a measure of disease intensity in frontotemporal dementia. Neurology. 2016;87(13):1329–36.
Bacioglu M, Maia LF, Preische O, et al. Neurofilament light chain in blood and CSF as marker of disease progression in mouse models and in neurodegenerative diseases. Neuron. 2016;91:1–11.
Kuhle J, Barro C, Andreasson U, et al. Comparison of three analytical platforms for quantification of the neurofilament light chain in blood samples: ELISA, electrochemiluminescence immunoassay and Simoa. Clin Chem Lab Med. 2016;54(10):1655–61. doi:10.1515/cclm-2015-1195.
Gisslén M, Price RW, Andreasson U, et al. Plasma concentration of the neurofilament light protein (NFL) is a biomarker of CNS injury in HIV infection: a cross-sectional study. EBioMedicine. 2015;22(3):135–40.
O’Bryant SE, Gupta V, Henriksen K, STAR-B and BBBIG working groups, et al. Guidelines for the standardization of preanalytic variables for blood-based biomarker studies in Alzheimer’s disease research. Alzheimers Dement. 2015;11(5):549–60.
Ray S, Britschgi M, Herbert C, et al. Classification and prediction of clinical Alzheimer’s diagnosis based on plasma signaling proteins. Nat Med. 2007;13(11):1359–62.
Soares HD, Chen Y, Sabbagh M, et al. Identifying early markers of Alzheimer’s disease using quantitative multiplex proteomic immunoassay panels. Ann N Y Acad Sci. 2009;1180:56–67.
Björkqvist M, Ohlsson M, Minthon L, et al. Evaluation of a previously suggested plasma biomarker panel to identify Alzheimer’s disease. PLoS One. 2012;7(1):e29868.
Casanova R, Varma S, Simpson B, et al. Blood metabolite markers of preclinical Alzheimer’s disease in two longitudinally followed cohorts of older individuals. Alzheimers Dement. 2016;12(7):815–22.
Doecke JD, Laws SM, Faux NG, et al. Blood-based protein biomarkers for diagnosis of Alzheimer disease. Arch Neurol. 2012;69(10):1318–1325.
Zhang R, Barker L, Pinchev D, et al. Mining biomarkers in human sera using proteomic tools. Proteomics. 2004;4(1):244–56.
Trushina E, Dutta T, Persson XT, et al. Identification of altered metabolic pathways in plasma and CSF in mild cognitive impairment and Alzheimer’s disease using metabolomics. PLoS One. 2013;8(5):e63644.
Sattlecker M, Kiddle SJ, Newhouse S, et al. AddNeuroMed Consortium. Alzheimer’s disease biomarker discovery using SOMAscan multiplexed protein technology. Alzheimers Dement. 2014;10(6):724–34.
Lopez MF, Mikulskis A, Kuzdzal S, et al. High-resolution serum proteomic profiling of Alzheimer disease samples reveals disease-specific, carrier-protein-bound mass signatures. Clin Chem. 2005;51:1946–54.
Jaeger PA, Lucin KM, Britschgi M, et al. Network-driven plasma proteomics expose molecular changes in the Alzheimer’s brain. Mol Neurodegener. 2016;11:31. doi:10.1186/s13024-016-0095-2.
Hu WT, Holtzman DM, Fagan AM, et al. Plasma multianalyte profiling in mild cognitive impairment and Alzheimer disease. Neurology. 2012;79:897–905.
Mapstone M, Cheema AK, Fiandaca MS, et al. Plasma phospholipids identify antecedent memory impairment in older adults. Nat Med. 2014;20:415–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ashvini Keshavan and Amanda Heslegrave have nothing to declare. Henrik Zetterberg is one of the founders of Brain Biomarker Solutions in Gothenburg AB, a GU Venture-based platform company at the University of Gothenburg, Sweden. Jonathan M. Schott has funding from Alzheimer’s Research UK, the Medical Research Council, AVID Radiopharmaceuticals, the Wolfson Foundation, the Brain Research Trust and EU Horizon 20:20 but none has influenced the preparation of this paper.
Funding
No funding was received for the preparation of this paper.
Additional information
H. Zetterberg and J. M. Schott are joint senior author of this article.
Rights and permissions
About this article
Cite this article
Keshavan, A., Heslegrave, A., Zetterberg, H. et al. Blood Biomarkers for Alzheimer’s Disease: Much Promise, Cautious Progress. Mol Diagn Ther 21, 13–22 (2017). https://doi.org/10.1007/s40291-016-0241-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40291-016-0241-0