Abstract
The Medical Affairs (MA) function in pharmaceutical companies creates a unique opportunity to ensure the internal linkage between Research & Development (R&D) and Commercial/Marketing functions, in addition to managing external scientific engagements with multiple stakeholders across life-science ecosystems. In recognition of the strategic value of MA, the objective of this paper is to share a comprehensive set of practical examples of the main deliverables within the MA function in the affiliate and align these with the two distinct phases; pre- and post-launch, respectively. We believe that an information gap currently exists in the available literature on these matters addressing practical aspects and examples beyond visionary, strategic thinking. Based on this contribution, further opportunities within MA can be discussed. In addition, we share our thoughts and considerations on future advancements in the role.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Global public health care requires effective disease management improvements and strategies to achieve healthier populations. In parallel, scientific advancements through translational and clinical research outcomes increasingly provide opportunities at pace for improved diagnostics and precision medicine to achieve tailor-made health care solutions. |
The Medical Affairs (MA) role has evolved in recent decades from an internally focused support function to become a strategically important function with a widened external lens keeping the customer- and patient-centric scope through “Outside-In” perspectives. |
The MA function most likely continues to play an increasingly strategic role together with colleagues within R&D and Commercial/Marketing functions to achieve the optimal science-driven dialogue and thereby ensure the alignment of common goals to improve patient outcomes. |
1 Introduction
The main goal for local Medical Affairs (MA) teams in pharmaceutical companies is to translate and contextualize the clinical value of innovative medicines to stakeholders in the health care ecosystems such as health care professionals (HCPs), payers, hospital administrators, and other health care decision makers. The MA function achieves this through its scientific and research understanding and management competencies, in addition to the unique organizational position serving as the connector between Research & Development (R&D) and Commercial/Marketing functions. In addition to the internal support in commercialization of innovative medicines, MA employees manage external scientific engagements with multiple stakeholders across academia and life-science ecosystems. The emerging, strategic importance of MA has become widely recognized [1,2,3,4,5].
Global pharma organizations ideally establish strong internal communication channels and processes for content and knowledge exchange, providing customer-facing colleagues in the affiliates with most updated and relevant information for external exchange. The flow of communication alternates, depending on life-cycle timing, pre- and post-launch, respectively. During pre-launch, where the global MA team (GMA) receives information first, due to its position closer to the global R&D teams, GMA can proactively distill and communicate relevant data for the affiliate teams. Likewise, in the post-launch period, the flow of data reverses due to the introduction of the medicine in daily clinical practice, which allows patients access to medicine, and through real-world clinical practices and user-experiences from both patients and HCPs, the insights provided by the affiliate team benefits the GMA teams in developing the value proposition further.
Roles and responsibilities in MA depend on the specific organization, e.g., whether the role is global, regional, or local. In this paper, we focus on the MA function in the affiliate, as we believe there is an information gap in the available literature in this area. While there are multiple job titles in MA, e.g., Medical Scientific Liaison (MSL), Medical Manager, Medical Lead, Medical Director, Medical Head, we will focus on the roles with external responsibilities, roles that usually hold the title of Medical Advisor or MSL. A recent progress report on the achievement of Sustainable Development Goals (SDG) from the United Nations revealed that most of the SDGs are moderately to severely off track, including SDG #3: “Ensure healthy lives and promote well-being for all” [6]. In parallel, scientific advances and digital technologies are advancing at pace, creating opportunities for improved patient diagnostics, treatments, follow-up, in turn enabling more effective health care management. A large proportion of today’s global R&D pipelines is targeted “precision medicine” [7]. A white paper “Future of Medical Affairs 2030” by the Medical Affairs Professional Society (MAPS) highlighted the role of MA to address issues of value for societies by representing the voice of patient communities in the development and access provisioning of innovative solutions [4]. In line with societal, pharmaceutical, and clinical research developments, the MA role has undergone significant development over time [2] and is expected to continue to adapt. In recognition of the strategic value of MA, the objective of this paper is to share a comprehensive set of practical examples of the main deliverables and align these with the two distinct phases: pre- and post-launch, respectively. We believe that a gap in the available literature currently exists, which addresses practical aspects beyond visionary, strategic thinking. Based on this contribution, further opportunities within MA can be discussed. Additionally, we want to share our perspectives on future advancements in the role.
2 Medical Affairs Pursuing “Inside-Out” and “Outside-In” Principles
A major competence within the MA function in the affiliate remains the clinical and scientific expertise within the designated therapy area (TA) enabling contextualization and dissemination of the clinical value of medicines demonstrated through clinical Phase 1–3 studies and Phase 4 real-world evidence (RWE) studies. Through this expertise, MA teams can collaborate with HCPs to better identify relevant patient populations who may safely and effectively benefit from innovative medicines and treatments. In addition, internal colleagues across functions are educated on medical topics to enable them to execute meaningful projects within the health care ecosystem.
The evolving role of Medical Directors was recently suggested to encompass several key skills and capabilities such as for example: “partnering for synergies”, “keeping patient-centricity”, and “sharpening competencies to ensure scientific & technological leadership” [8]. These skills are critical for successful MA teams, as they hold internal and external value and may be considered in the context of “inside-out and outside-in” principles [9].
2.1 Inside-Out
A customer-centric approach to ensure internal value is delivered to the right customer at the right time. Examples and categories are presented below.
-
Scientific and clinical research engagements and clinical education initiatives
-
o
Engage HCPs in relevant company-sponsored clinical trials and/or non-interventional post-marketing studies or serve as the focal point of contact for clinical investigators when running investigator-sponsored research within mutually agreed research areas.
-
o
Ensure company-sponsored clinical trial completions which fulfill regulatory requirements to achieve market authorizations of novel, innovative medicines.
-
o
-
Ensure patient access to new, innovative medicines in liaison with national payer entities, writing up clinical dossiers for HTA evaluation and sometimes negotiation, based on modern analytics and scientific approaches.
-
Customer- and patient-centered communication
-
o
Communication of scientific and clinical content, disease awareness or product-related information using multiple channels, via both virtual and physical engagements, using the channel preferred by the HCP, and with content that meets HCP requirements. Patient representatives may be activated through collaborative projects to, e.g., increase awareness of disease burden and incorporate patient perspectives.
-
o
2.2 Outside-In
The pharmaceutical company aims to understand the needs of the various players within the health care ecosystem in which it operates through active listening and engagement with relevant stakeholders and thereby develop improved company strategies and action plans that make a difference for patients or society through mutually agreeable goals.
-
Medical and clinical insights collection
-
o
Through external peer-to-peer collaborations, observations are obtained and reported internally. These insights aim to impact strategic planning and execution within the organization, either confirming strategy or modifying strategy.
-
o
-
Public-Private Partnerships
-
o
Co-create projects to deliver improved patient identification and diagnosis, improve patient access to innovative medicines, or ensure continued patient support and follow-up in the long term.
-
o
-
Patient-centricity
-
o
Involve patient representatives in projects, to consider their input in the development phase, and thereby develop solutions more likely to hold value for patients.
-
o
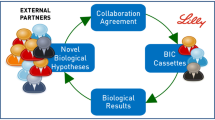
In Fig. 1 the inside-out and outside-in approach is presented.
2.3 Where is the Current Attention Within These Principles?
The primary deliverable for the local MA team remains to be translation and contextualization of the clinical value of medicines to the relevant stakeholders in the health care ecosystem. However, in parallel with technological and biological advances, increased attention has been given to outside-in principles. Collectively, the current focus in MA deliverables centers around the following categories:
-
Clinical research collaboration and engagements.
-
Clinical insight management, including collection, management, and actioning.
-
RWE generation, e.g., through national registries, regional databases, and other RWD sources.
-
Health technology assessments and clinical dossier creation.
-
Clinical data analysis, publication, and dissemination
Therefore, while MA colleagues historically primarily executed their work according to “inside-out strategies”, to address the perceived unmet medical needs among HCPs, the approach has broadened to encompass the external needs and views through “outside-in strategies”. Via these strategies, MA colleagues focus on observing and understanding the external needs in the wider ecosystem, which includes clinicians, researchers, patients, and payer perspectives, amongst others. With these combined insights, the local cross-functional team will be better equipped to address unmet medical needs. A key enabler for MA staff is their non-promotional role, which can provide valuable insights to impact the development of both pipeline and marketed products, and ensure unbiased, objective, and balanced medical/clinical data exchange and discussions with HCPs and Key External Experts (KEEs). This supports the MA to become a trusted partner within the health care system.
We speculate that in the future, the focus on outside-in principles within pharma will increasingly help companies take larger responsibilities within societal challenges to deliver sustainable health care solutions, improve health inequalities, and thereby improve the quality of patient’s lives, also in line with SDGs [6].
3 Medical Affairs Deliverables and Suggested Timing
Medical Affairs is responsible for scientific expertise internally and provides an interface between the company and external audiences, such as key opinion leaders (KOLs), KEEs and HCPs, by engaging in non-promotional, fair, and balanced scientific exchange.
In Fig. 2, an overview of the main MA deliverables in support of either pre-or post-launch activities is given. The proposed timing indicates when a suggested activity will most likely take place during the life cycle of a medicinal product. A detailed summary of MA-led activities and associated timing is presented in the Supplementary Information. Notably, several of these activities are relevant throughout the medicine life cycle.
Multiple factors may influence the prioritization and timing of medical activities to ensure optimal implementation and launch of a new, innovative medicine upon local, regulatory approval and reimbursement. Some of these factors include:
-
How do company strategies for new innovative medicines balance versus existing business opportunities?
-
Is the company entering a new TA, or is the company already an expert within the TA?
-
Does the MA team have experience within the TA through previous activities?
-
Is the new medicine a “first in class” medicine, which means that prescribing physicians will manage a new treatment principle, a new mode of administration?
-
Have clinical evidence gaps been identified?
-
Did investigator sites within the country participate in the Phase 1–3 Clinical Development Program?
All the above considerations (not exhaustive) inform the senior leaders’ strategic planning and decisions, which may influence the extent and timing of MA team engagement.
4 Opportunities Ahead
The global trends, which suggest that the MA function should play a larger, more strategic role in the affiliate [1,2,3,4,5], were recently confirmed in a Nordic setting [10]. The research concluded that Nordic pharma executives consider that a scientifically skilled workforce is key to ensure pharma success going forward. The MA role was rated among the most important for future success (after the Market Access manager). One major challenge listed in the report was that HCPs often close their doors to salespeople. Moreover, the Nordic pharma executives predicted that the use of RWE will be increasingly important in the future [10]. It is expected that RWE will be essential for local payer and regulatory decision making. This is likely guided by the continued and increased availability of local disease-specific registries aiming to capture and analyze the effectiveness and tolerability of non-interventional daily clinical practice data across disease areas [11]. Furthermore, data reporting guidelines have been developed to ensure the highest quality and validity of data. Examples include the international standards for health economics and outcomes research and its use in health care decision making (ISPOR) [12]; STaRT-RWE: structured template for planning and reporting on the implementation of RWE studies [13]; and STROBE: strengthening the reporting of observational studies in epidemiology [14] to name a few.
In recent decades, we have seen a vast development of country-specific registries, e.g., within European rheumatology [15]. In line with this initiative, an opportunity for the affiliate is to further enhance the cross-country RWE collaboration as suggested by Burns et al. [16]. According to Naidoo et al. [17] RWE may increase technical and regulatory success, thus serving as an important means for pharmaceutical companies to reduce financial risks associated with investing in costly R&D programs. It is argued that Health Technology Assessment (HTA) agencies are exploring the use of RWE to contribute to the benefit-risk assessment of drugs. Sievers et al. [18] consider that early collaboration between relevant public/private stakeholders in the post-license phase can help bridge the gaps between regulatory and HTA perspectives with the aim to address uncertainties regarding evidence needs, and to optimize drug development as well as monitoring of appropriate use. This will likely enable cost reductions and minimize duplication of post-launch studies, which may, in turn, delay patient access. Taken together, competencies within study methodologies for design and analysis purposes will continuously be of huge importance, with the purpose of enabling data gap analysis and discussing local study development, conduct, and reporting among relevant stakeholders externally.
5 Perspectives
A recent survey by Deloitte reported five major impactful areas to ensure future societal improvements, such as curative therapies, customized treatments, digital therapeutics, prevention and early detection, and non-pharmacological interventions [19]. In line with these, and with expectations from Nordic executives [10], we speculate that major competency needs for MA professionals in the future will center around the following:
-
continued superior knowledge on up-to-date clinical research advancements
-
data science competencies including analysis and identification of clinical data gaps, study design, data analysis skills, strategic data publication, and dissemination
-
in-depth health care system understanding
-
the ability to develop and execute sustainable projects and health care solutions
-
willingness to partner and collaborate with multiple stakeholders across the evolving health care ecosystem.
We anticipate that future successful MA teams will benefit from widening their collaborations with external stakeholders, including patient groups, health care providers, payers, and politicians, and engaging with these in data-driven discussions to co-lead the transformation of sustainable health care solutions. The value and insights gained from these external collaborations will be fed into the value chain in the company, including R&D, Marketing, and Regulatory Affairs, to ensure that drugs and therapies are developed, tested, and launched effectively and sustainably. Furtner and colleagues recently described the opportunity within MA to take a leadership role in the tactical implementation of environmental, social, and governance (ESG) tactics through the conduct of sustainable and climate-friendly clinical studies, educational symposia, and conduct of meetings, e.g., by utilization of digital platforms and virtual solutions and thus act as a socially responsible entity within the company embracing compliant and sustainable ESG policies [20].
Overall, the future success of MA in pharmaceutical companies will likely be characterized by increased focus on patient-centricity, the use of digital technologies and RWD utilization, extensive creation of RWE, greater collaboration and co-creation with new stakeholders, and increased regulatory scrutiny. Medical Affairs teams will need to adapt to these changes to ensure that they continue to play a critical role. See Table 1 for further details for expected major competency needs and value drivers.
Looking ahead, competency development in the MA teams is first and foremost needed to meet expectations and maximize opportunities within the “outside-in” strategic approach. In previous years, in which most of the industry provided primary care medications, MA employees were generally medical doctors, who held the necessary expert competencies to partake in a dialogue with general practitioners and answer their questions on the optimal use of medicine. Through research and medicinal advancements, which introduced precision medicines, gene therapies, rare disease management, vaccines, and additional advanced technologies, the importance of the hospital setting has advanced significantly [2]. Thus, today, in addition to hiring medical doctors, most companies have broadened the staffing policy within MA to employ competencies within Biomedicine, Molecular Biology, Pharmaceutical sciences, and Biochemistry, amongst others.
Second, continued capability building in MA has received increased attention. This has resulted in advanced capabilities within data generation planning (RWE, pragmatic trials, PROs). Digital competences enable MA engagements with HCPs using more channels, more complex set-ups of educational meetings, for example, hybrid meetings, and social listening projects, where information/activity regarding disease and management of diseases is analyzed in a structural approach.
Third, the strategic focus in the affiliate to optimize diagnostics, treatment initiation and follow-up of patients through co-creation with both HCPs and patients, to collaborate with new stakeholders and between pharmaceutical companies on, e.g., disease awareness and evolutions within, e.g., RWE and digital tools, has proved to be successful. As an example, MAPS, which is a non-profit global MA organization for MA professionals, has developed a platform with access to training and educational material for members, who also are encouraged to contribute and develop new materials [5].
Key competencies are required within evidence generation to bridge data gaps and generate meaningful evidence in support of improved patient outcomes and evidence reflecting real-world clinical setting.
Further, insight gathering and understanding of the value proposition of the KEEs will continue to be of importance to establish collaborations with health care organizations to identify and establish projects and studies in support of a joint value proposition to improve patient outcomes.
Global MA is usually the strategic driver for defining innovative and scientific value propositions for the company’s products, through their understanding of patients, physicians, and global business trends. Global MA defines the medical and value evidence strategies and drives evidence generation with the goal of improving patient health outcomes based on patient, disease, and clinical landscape insights gained through patient and HCP engagements. Furthermore, GMA ensures aligned and compliant communication to patients, HCPs, regulators, and payers. Thus, strong and transparent partnerships between the global and affiliate MA teams are critical for the ultimate success of innovative medicines in the local markets during pre- and post-launch periods. Thus, ”glocalization” potentially plays a critical part in effective MA and strengthening the partnership between global and affiliate MA in critical areas such as insight generation, understanding clinical practices and identifying the most critical points for close GMA and affiliate collaboration will be of future importance. The glocalization model offers further strengthening of the MA strategic contribution and planning, including local insights collection, and analysis to further support evidence generation planning and execution, acknowledging the local insights and experience of innovative treatment.
As the MA role continues to evolve, to address emerging demands and new opportunities, a unified national or regional certification in MA could potentially be valuable. Such certification might support and help address the needs for new competencies and capabilities, and thereby suggest uniform yet personalized and compliant ways to engage with stakeholders and expert networks. Other areas of value considered are how to generate the most relevant clinical evidence and data; rapid tech evolution; increasing adoption and compliance in new communication channels.
The current value of MA from the affiliate perspective and the opportunities that lie ahead of MAs to ensure better health and quality of life for future generations and sustainable societies have been presented. It has been shown that MA is highly fascinating for several reasons, at times even challenging and complex, due to the varying deliverables and accompanying competencies needed.
6 Conclusion
The MA function remains central in the pharma company’s liaison with numerous stakeholders internally and externally. Through scientific and research knowledge, MA professionals generate and disseminate clinical practice relevant data and contextualize it in current clinical practices aiming for continued improvements of patient outcomes.
Medical Affairs objectives increasingly focus on meeting the needs of external health care stakeholders such as senior clinicians, hospital administrators, regional health care directors, and national health organizations. Therefore, patient- and HCP-centricity is a cornerstone as we arrange our agendas according to the Outside-In principles enabling the MA function to act as the eyes and the ears of pharma companies through external engagements. Observing, listening to, and exploring mutual goals with health care decision makers may prove essential for future success within MA.
With increasing health care expenditures due to evolving population demographics and associated impact of people living with chronic diseases worldwide and the coinciding health care and research technological advancements, the need for public-private partnering to meet the societal health challenges through innovative health care solutions is increasing. For the MA function per se, and pharma companies in general, this calls for co-develop innovative, sustainable, cost-effective, and climate-friendly solutions to improve patient outcomes.
The expected strategic role of MA in pharmaceutical companies as communicated by various authors in recent years was recently confirmed through qualitative research in which Nordic executives speculate that the future successful pharma affiliates to a larger extent will rely on MA professionals in addition to skilled deliverables within Health Economics, Governmental Affairs, and Market Access. Also, roles with digital expertise will be crucial. This is most likely caused by the current and future advancements and opportunities within precision medicine and orphan disease management requiring specific diagnostics and other sophisticated patient-evaluations prior to treatment initiation and care management. Evidently, the ability to identify the appropriate patient population suitable for personalized treatment may require specific education of the HCPs, which will likely be a responsibility of MA personnel in many cases.
The future holds promise of increasing needs for skilled and competent MA colleagues to generate and disseminate clinical, scientific data in support of medicine commercialization. It will be crucial for the function to acquire new knowledge and competencies within digital health solutions, artificial intelligence, and machine learning algorithms relevant to clinical practices. The ability to build sustainable external relationships and to collaborate on mutually agreeable goals to co-create practice relevant projects remains crucial to success. Competencies within data science to outline and fill specific evidence gaps in the current treatment traditions will only increase.
References
McKinsey and Company. A vision for Medical Affairs in 2025: https://www.mckinsey.com/industries/life-sciences/our-insights/a-vision-for-medical-affairs-in-2025. Accessed 7 Jun 2023.
Bedenkov A, Rajadhyaksha V, Beekman M, Moreno C, Fong PC, Agustin L, et al. Developing medical affairs leaders who create the future. Pharmaceut Med. 2020;34(5):301–7. https://doi.org/10.1007/s40290-020-00351-y.
Bedenkov A, Moreno C, Agustin L, Jain N, Newman A, Feng L, et al. Customer centricity in medical affairs needs human-centric artificial intelligence. Pharmaceut Med. 2021;35(1):21–9. https://doi.org/10.1007/s40290-020-00378-1.
MAPS. The future of medical affairs. 2030. https://medicalaffairs.org/. Accessed 7 Jun 2023.
MAPS. The Mission, Value, and Roles of Medical Affairs in MedTech. https://medicalaffairs.org/medical-affairs-medtech-white-paper/. Accessed 7 Jun 2023.
UN report on the progress towards the Sustainable Development Goals submitted in response to General Assembly resolution 70/1, Transforming Our World: the 2030 Agenda for Sustainable Development. April, 2023. https://hlpf.un.org/sites/default/files/2023-04/SDG%20Progress%20Report%20Special%20Edition.pdf. Accessed 7 Jun 2023.
PhRma. Innovation in the Biopharmaceutical Pipeline. Dec, 2021: https://phrma.org/-/media/Project/PhRMA/PhRMA-Org/PhRMA-Org/PDF/G-I/Innovation_in_Biopharmaceuticals.pdf. Accessed 7 Jun 2023.
Bedenkov A, Rajadhyaksha V, Moreno C, Goncalves S, Fong PC, Ipatov A, et al. The 7+ habits of highly effective medical directors. Pharmaceut Med. 2021;35(5):267–79. https://doi.org/10.1007/s40290-021-00403-x.
Frau M, Moi L, Cabiddu F. Outside-in, inside-out, and blended marketing strategy approach: a longitudinal case study. IntJ Mark Stud. 2020;12(3):1. https://doi.org/10.5539/ijms.v12n3p1.
DLIMI. Forward Thinkers Review, 2022 by DLIMI, Atrium, and SPI: https://dlimi.com/forside/forward-thinkers-review/. Accessed 7 Jun 2023.
Thor Petersen C, Jensen KJ, Rosenzweig M, von Osmanski BI, Ankarfeldt MZ, Petersen J. Mapping outcomes and registries used in current Danish pharmacoepidemiological research. Clin Epidemiol. 2022;26(14):521–42. https://doi.org/10.2147/CLEP.S341480.
ISPOR Good Practices and More: https://www.ispor.org/heor-resources/good-practices. Accessed 5 May 2023.
Wang SV, Pinheiro S, Hua W, Arlett P, Uyama Y, Berlin JA, et al. STaRT-RWE: structured template for planning and reporting on the implementation of real world evidence studies. BMJ. 2021;372:m4856. https://doi.org/10.1136/bmj.m4856.
STROBE: Strengthening the reporting of observational studies in epidemiology https://www.strobe-statement.org/. Accessed 8 May 2023.
Christiansen SN, Ørnbjerg LM, Rasmussen SH, Loft AG, Askling J, Iannone F, et al. European bio-naïve spondyloarthritis patients initiating TNF inhibitor: time trends in baseline characteristics, treatment retention and response. Rheumatology (Oxford). 2022;61(9):3799–807. https://doi.org/10.1093/rheumatology/keab945.
Burns L, Roux NL, Kalesnik-Orszulak R, Christian J, Hukkelhoven M, Rockhold F, et al. Real-world evidence for regulatory decision-making: guidance from around the world. Clin Ther. 2022;44(3):420–37. https://doi.org/10.1016/j.clinthera.2022.01.012.
Naidoo P, Bouharati C, Rambiritch V, Jose N, Karamchand S, Chilton R, et al. Real-world evidence and product development: Opportunities, challenges and risk mitigation. Wien Klin Wochenschr. 2021;133(15–16):840–6. https://doi.org/10.1007/s00508-021-01851-w.
Sievers H, Joos A, Hiligsmann M. Real-world evidence: perspectives on challenges, value, and alignment of regulatory and national health technology assessment data collection requirements. Int J Technol Assess Health Care. 2021;37: e40. https://doi.org/10.1017/S0266462321000131.
Biopharma leaders prioritize R&D, technological transformation, and global market presence. Findings from a new survey and analysis of investor calls in the first half of 2020 - a report by Deloitte, 2020 www.2.deloitte.com/xe/en/insights/industry/life-sciences/pharmaceutical-industry-trends. Accessed 7 Jun 2023.
Furtner D, Hutas G, Tan BJW, et al. Journey from an enabler to a strategic leader: integration of the medical affairs function in ESG initiatives and values. Pharm Med. 2023. https://doi.org/10.1007/s40290-023-00485-9.
Acknowledgments
Many thanks to Dr. Alexandr Bedenkov and Dr. Anne Bloch Thomsen for their review of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding has been received for this manuscript. The open access fee was paid by Pfizer Denmark.
Conflicts of Interest/Competing Interests
Anupma Dhanda Farrington, Anne Grete Frøstrup, and Palle Dahl are full-time employees of Lundbeck Pharma A/S, Pfizer Denmark, and AstraZeneca A/S, respectively. Anne Grete Frøstrup has Pfizer Inc. stock options. Palle Dahl holds stock options at AstraZeneca A/S. All statements or opinions expressed in the manuscript are those of the authors and do not necessarily represent the opinions of their employers (Lundbeck Pharma A/S, Pfizer Denmark, and AstraZeneca A/S).
Availability of Data and Material
Not applicable.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Availability of Data and Material
Not applicable.
Code Availability
Not applicable.
Authors' Contributions
All authors contributed equally to researching, authoring, and reviewing the manuscript. All authors have read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Farrington, A.D., Frøstrup, A.G. & Dahl, P. The Value and Deliverables of Medical Affairs: Affiliate Perspectives and Future Expectations. Pharm Med 37, 417–424 (2023). https://doi.org/10.1007/s40290-023-00501-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40290-023-00501-y