Abstract
Background
Overuse injuries are common in sporting children and adolescents. These injuries are a particular concern when they involve the epiphyseal–physeal–metaphyseal (EPM) complex given their potential to disturb skeletal growth. Specifically, the limits of mechanical tolerance of the EPM complex to repetitive stress may be exceeded by the intense and continuous training characteristic of many youth sports today.
Objective
This article describes the present status of knowledge on the occurrence and outcome of primary periphyseal stress injuries (PPSIs) affecting the EPM complex in the extremities of children and adolescents involved in youth sports.
Methods
A comprehensive review of the sports medicine literature was conducted to determine the nature and extent of PPSIs affecting the EPM complex of the extremities among youth sports participants and the potential for consequent skeletal growth disturbance and resultant limb deformity associated with these injuries.
Results
Our initial search uncovered 128 original published scientific articles reporting relevant data on PPSIs. There were 101 case reports/series, 19 cross-sectional, 1 case–control, and 7 cohort studies with relevant data. The case reports/series studies reported 448 patients with PPSIs involving the extremities. Children and adolescents representing a variety of high impact repetitive youth sports activities—including baseball, badminton, climbing, cricket, dance, gymnastics, rugby, soccer, swimming, tennis, and volleyball—may sustain PPSIs involving the shoulder, elbow, hand and wrist, knee, and ankle and foot. Although incidence data from prospective cohort studies are lacking, data arising from cross-sectional studies suggest that PPSIs may be common in select groups of youth athletes—including the shoulder in baseball players (0–36.6%), wrist in gymnasts (10–83%) and platform divers (52.6%), and fingers in rock climbers (5–58%). Notably, not all stress-related skeletal changes detected on imaging were symptomatic in these studies. When diagnosed and treated with an appropriate period of rest and rehabilitation, most patients studied were able to return to their sport activities. However, our data also show that 57/448 PPSIs (12.7%) produced growth disturbance, and that 28/448 patients (6.2%) underwent surgery for their injuries. Absence of treatment, delayed presentation and diagnosis, and non-compliance with a rest regimen were common in cases that produced growth disturbance.
Conclusions
PPSIs may affect the extremities of children and adolescents engaged in a variety of youth sports, especially at advanced levels of training and competition. Most skeletally immature patients with PPSIs respond well to timely treatment; however, in extreme cases, PPSIs can progress to produce skeletal growth disruption which may necessitate surgical intervention. Clearly, establishing the early diagnosis of PPSIs and providing timely treatment of these injuries are needed to ensure the skeletal health of youth sports participants. Rigorous prospective longitudinal epidemiological and imaging studies designed to provide incidence rates of PPSIs and to determine the effect of PPSIs on long-term skeletal health are also necessary.







Similar content being viewed by others
References
Caine DJ. Are kids having a rough time of it in sports? Br J Sports Med. 2010;44:1–3.
Caine DJ, Provance AJ. Pediatric and adolescent injury in adventure and extreme sports. Res Sports Med. 2018;26:5–19.
Maffulli N. Children in sport: questions and controversies. In: Maffulli N, editor. Color Atlas and Text of Sports Medicine in Children and Adolescence. London: Mosby-Wolfe; 1995. p. 7–14.
Maffulli N, Caine D. The epidemiology of children’s team sports injuries. In: Maffulli N, Caine D, editors. Epidemiology of pediatric sports injuries: team sports. Med sport sci, vol 49. Basel: Karger; 2005. p. 1–8.
Schöffl V, Hoffmann P, Imhoff A, Kupper T, Schöffl I, Hochholzer T, et al. Long-term radiographic adaptations to stress of high-level and recreational rock climbing in former adolescent athletes. An 11-year prospective longitudinal study. Orthop J Sports Med. 2018;6:1–9.
Steffen K, Engebretsen L. More data needed on injury risk among elite young athletes. Br J Sports Med. 2010;44:485–9.
Youth Olympic Games. https://www.olympic.org/youth-olympic-games. Accessed 1 Mar 2020
U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd Edition. Washington, DC: U.S. Department of Health and Human Services; 2018. https://health.gov/paguidelines/second-edition/pdf/Physical_Activity_Guidelines_2nd_edition.pdf. Accessed 1 Feb 1 2020.
Emery CA. Injury prevention in kids’ adventure and extreme sports: future directions. Res Sports Med. 2018;26(Supple. 1):199–211.
DiFiori JP. Overuse injury of the physis: a “growing” problem. Clin J Sport Med. 2010;20:336–7.
Armstrong N, McManus AM. Preface. The elite young athlete. Med Sport Sci. 2011;56:1–3.
Sabato T, Walch T, Caine D. The elite young athlete: strategies to ensure physical and emotional health. Open Access J Sports Med. 2016;7:99–113.
DiFiori JP, Benjamin HJ, Brenner J, Gregory A, Jayanthi N, Landry JL, et al. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Clin J Sport Med. 2014;24:3–20.
Maffulli N, Longo UG, Gougoulias N, Loppini M, Denaro V. Long-term health outcomes of youth sports injuries. Br J Sports Med. 2010;44:21–5.
Caine D, DiFiori J, Maffulli N. Physeal injuries in children’s and youth sports: reasons for concern? Br J Sports Med. 2006;40:749–60.
Schöeffl L, Schöeffl V. Epiphyseal stress fractures in the fingers of adolescents: biomechanics, pathomechanisms, and risk factors. Eur J Sports Med. 2015;3:27–37.
Hochholzer Th, Schöffl V. Epiphyseal fractures of the finger middle joints in young sport climbers. Wilderness Environ Med. 2005;16:139–42.
Ogden JA. Skeletal injury in the child. New York: Springer; 2000.
Caine D, Howe W, Ross W, Bergman G. Does repetitive physical loading inhibit radial growth in female gymnasts. Clin J Sport Med. 1997;7:102–8.
Moher D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Ann Intern Med. 2013. https://doi.org/10.7326/0003-4819-151-4-200908180-00135.
Laor T, Wall EJ, Vu LP. Physeal widening in the knee due to stress injury in child athletes. Am J Roentgenol. 2006;186:1260–4.
Bedoya MA, Jaramillo D, Chauvin NA. Overuse injuries in children. Top Magn Reson Imaging. 2015;24:67–81.
Jaramillo D, Laor T, Zaleske DJ. Indirect trauma to the growth plate: results of MR imaging after epiphyseal and metaphyseal injury in rabbits. Radiology. 1993;187:171–8.
Nguyen JC, Markhardt BK, Merrow AC, Dwek JR. Imaging of pediatric growth plate disturbances. RG. 2017;17:1791–812.
Dotter WE. Little leaguer’s shoulder. Guthrie Clin Bull. 1953;23:68–72.
Roy S, Caine D, Singer K. Stress changes of the distal radial epiphysis in young gymnasts. A report of twenty-one cases and a review of the literature. Am J Sports Med. 1985;13:301–8.
Shih C, Chang CY, Penn IW. Chronically stressed wrists in adolescent gymnasts: MR imaging appearance. Radiology. 1995;195:855–9.
Dwek JR, Chung CB. Lower extremity overuse injuries in pediatric athletes: clinical presentation, imaging findings and treatment. Clin Imaging. 2013;37:836–46.
Salter RB, Harris WR. Injuries involving the epiphyseal plate. J Bone Jt Surg. 1963;45A:587–622.
Cummings P, Weiss NS. Case series and exposure series: the role of studies without controls in providing information about the etiology of injury or disease injury prevention. Inj Prev. 1998;4:54–7.
Heyworth BE, Kramer DE, Martin DJ, Kocher MS, Bae DS. Trends in the presentation, management, and outcomes of little league shoulder. Am J Sports Med. 2016;44:1431–8.
Hansen NM Jr. Epiphyseal changes in the proximal humerus of an adolescent baseball pitcher: a case report. Am J Sports Med. 1982;10:380–4.
Adams JE. Little league shoulder: osteochondrosis of the proximal humeral epiphysis in boy baseball pitchers. Calif Med. 1966;105:22–5.
Torg JS. The little league pitcher. Am Fam Phys. 1972;6:71–6.
Cahill BR. Little league shoulder: rotational stress fracture of proximal epiphysis. J Sports Med. 1974;2:150–2.
Tullos HS, Fain RH. Little leaguer shoulder: lesions of the proximal epiphyseal plate. J Sports Med. 1974;2:152–3.
Lipscomb AB. Baseball pitching injuries in growing athletes. J Sports Med. 1975;3:25–34.
Barnett LS. Little league shoulder syndrome. Proximal humeral epiphysiolysis in adolescent baseball pitchers—a case report. J Bone Jt Surg (USA). 1985;67:495–6.
Albert MJ, Drvaric DM. Little league shoulder: case report. Orthopaedics. 1990;13:779–81.
Carson WG, Gasser SI. Little leaguer’s shoulder. A report of 23 cases. Am J Sports Med. 1998;26:575–80.
Ricci AR, Mason DE. Little league shoulder: case report and literature review. Del Med J. 2004;76:11–4.
Flemming JL, Hollingsworth CL, Squire DL, Bisset JS. Little leaguer’s shoulder. Skelet Radiol. 2004;33:352–4.
Hatem SF, Recht MP, Profitt B. MRI of little leaguer’s shoulder. Skelet Radiol. 2006;35:103–6.
Song JC, Lazarus ML, Song AP. MRI findings in little leaguer’s shoulder. Skelet Radiol. 2006;35:107–9.
Popkin CA, Posada A, Clifford PD. Little leaguer’s shoulder. Clin Imaging. 2006;30:365–7.
Obembe O, Gaskin CM, Taffoni MJ, Anderson MW. Little leaguer’s shoulder (proximal epiphysiolysis): MRI findings in four boys. Pediatr Radiol. 2007;37:885–9.
Anton C, Podberesky DJ. Little league shoulder: a growth plate injury. Pediatr Radiol. 2010;40(Supple 1):S54.
Domes CM, Petering R, Chesnutt JC, Mirarchi A. Concurrent little leaguer’s elbow and shoulder in a 15-year-old baseball pitcher and football quarterback. Orthop. 2012;35(1):e10–97.
Reeder MT, Smith B. Little league shoulder. J Am Osteopath Assoc. 2015;115:522.
Wasylynko D. Chronic pain due to little leaguer’s shoulder in an adolescent baseball pitcher: a case report. Can Chiropr Assoc. 2015;59:383–9.
Hosokawa Y, Mihata T, Yasuo Itami Y, Neo M, Doi M. Little leaguer’s shoulder can cause severe three-dimensional humeral deformity. Clin Orthop Surg. 2017;9:537–41.
Zipser MC, Sum JC, Wilcox AG. Little league shoulder in a 15-year-old male baseball pitcher. J Orthop Sports Phys Ther. 2018;48:51.
Greenburg EM, Turner C, Huse C, Ganley TJ, McClure T, Lawrence JT. Salter–Harris fracture of the proximal humerus in an adolescent gymnast. J Orthop Sports Phys Therap. 2018;48(9):729.
Boyd KT, Batt ME. Stress fracture of the proximal humeral epiphysis in an elite junior badminton player. Br J Sports Med. 1997;31:252–3.
Kirimura K, Nageo M, Sugiyama M. High incidence of posterior glenoid dysplasia of the shoulder in young baseball players. J Shoulder Elbow Surg. 2019;28:82–7.
Drescher WR, Falliner A, Zantop T, et al. Little league shoulder syndrome in an adolescent cricket player. Br J Sports Med. 2004;38:E14.
Daldorf PG, Bryan WJ. Displaced Salter–Harris type 1 injury in a gymnast. A slipped capital humeral epiphysis. Orthop Rev. 1994;23:538–41.
Ejnisman B, Andreoli V, Pochini ADC, et al. Proximal humeral epiphysiolysis in a gymnast. Acta Orthop Bras. 2007;15(5):290–1.
Kosnik M, Paulseth S, Abzug A. Salter–Harris fracture of the proximal humerus in an adolescent gymnast. J Orthop Sports Phys Ther. 2018;48(9):729.
Johnson JN, Houchin G. Adolescent athlete’s shoulder. A case series of proximal humeral epiphysiolysis in nonthrowing athletes. Clin J Sports Med. 2006;16:84–6.
Jenkinson E, Roush MB. Shoulder pain in a female volleyball player. Syllabus of the 6th American Medical Society for Sports Medicine Annual Meeting; 1996.
Carson JT, McCambridge TM, Carrino JA, McFarland EG. Case report: bilateral epiphyseal clavicular stress-related lesions in a male gymnast. Clin Orthop Relat Res. 2012;470:307–11.
Ellman H. Anterior angulation deformity of the radial head. An unusual lesion occurring in juvenile baseball players. J Bone Jt Surg Am. 1975;57:776–8.
Podestra L, Sherman MF, Bonamo JR. Distal humeral epiphyseal separation in a young athlete. A case report. Arch Phys Med Rehabil. 1993;74:1216–8.
Chan D, Aldridge MJ, Maffulli N, Davies AM. Chronic stress injuries of the elbow in young gymnasts. Br J Radiol. 1991;64:1111–8.
Maffulli N, Chan D, Aldridge MJ. Derangement of the articular surfaces of the elbow in young gymnasts. J Ped Orthop. 1992;12:344–50.
Huckaby MC, Kruse D, Gibbs LH. MRI findings of proximal radial physeal injury in a gymnast. Pediatr Radiol. 2012;42:1395–400.
Oda R, Fujiwara H, Ichimaru K, Morihara T, Ikeda T, Kubo T. Chronic slipping of bilateral humeral epiphyses in a gymnastist. J Pediatr Orthop B. 2015;24:67–70.
Miller SM, Wyatt CW, Ellis HB, Wilson PL. Proximal radial epiphyseal injuries in gymnasts. Pediatric Research in Sports Medicine Annual Meeting, Dallas, TX, January 26–28; 2017.
Santelli J, McCambridge T, Valasek AE, Standford K. Proximal radial head fractures in young gymnasts. Clin J Sport Med. 2019;29:e1–3.
Inagaki H, Inoue G. Stress fracture of the scaphoid combined with the distal radial epiphysiolysis. Br J Sports Med. 1997;31:256–7.
Kwon SW, Hong SJ, Nho JH, Moon S, Jung KJ. Physeal fracture in the wrist and hand due to stress injury in a child climber. Med. 2018;97:34.
Gerber SP, Griffin PP, Simmons BP. Case Report: Breakdancer’s wrist. J Ped Orthop. 1986;6:98–9.
Read MT. Stress fractures of the distal radius in adolescent gymnasts. Br J Sports Med. 1981;15:272–6.
Fliegel CP. Stress related widening of the radial growth plate in adolescents. Ann Radiol. 1986;29:374–6.
Carter SR, Aldridge MJ. Stress injury of the distal radial growth plate. J Bone Jt Surg (GB). 1988;70:834–6.
Carter SR, Aldridge MJ, Fitzgerald R, Davies AM. Stress changes of the wrist in gymnasts. Br J Radiol. 1988;61:109–12.
Resnick DL. Case 6: a12-year-old gymnast with intermittent pain in the wrist. Radiographics. 1988;8(2):246–8.
Yong-Hing K, Wedge JN, Bowen CV. Chronic injury to the distal ulnar and radial growth plates in an adolescent gymnast. J Bone Jt Surg (USA). 1988;70:1087–9.
Vender MI, Watson K. Acquired Madelung-like deformity in a gymnast. J Hand Surg (USA). 1988;13:19–21.
Albanese SA, Palmer AK, Kerr DR, Carpenter CW, Lisi D, Levinsohn M. Wrist pain and distal growth plate closure of the radius in gymnasts. J Ped Orthop. 1989;9:23–8.
Ruggles DL, Peterson HA, Scott SG. Radial growth plate injury in a female gymnast. Med Sci Sports Exerc. 1991;23:393–6.
Li DK, Lloyd-Smith R. Wrist pain in an adolescent gymnast. Clin J Sports Med. 1991;1:259–61.
Tolat AR, Sanderson PL, DeSmet L, Stanley JK. The gymnast’s wrist: acquired positive ulnar variance following chronic epiphyseal injury. J Hand Surg. 1992;17:678–81.
Carek PJ, Fumich RM. Stress fracture of the distal radius. Not just a risk for elite gymnasts. Phys Sportsmed. 1992;20(5):115–8.
Nattiv A, Mandelbaum BR. Injuries and special concerns in female gymnasts. Detecting, treating, and preventing common problems. Phys Sportsmed. 1993;21:66–82.
De Smet L, Claessens A, Fabrey G. Gymnast wrist. Acta Orthop Belg. 1993;59:377–80.
Liebling MS, Berdon WE, Ruzal-Shapiro C, Levin TL, Roye D, Wilkinson R. Gymnast’s wrist (pseudorickets growth plate abnormality) in adolescent athletes: findings on plain films and MR imaging. AJR. 1995;164:157–9.
DiFiori JP, Mandelbaum BR. Wrist pain in a young gymnasts: unusual radiographic findings and MRI evidence of growth plate injury. Med Sci Sports Exerc. 1996;28:1453–8.
Bak K, Boeckstyns M. Epiphysiodesis for bilateral irregular closure of the distal radial physis in a gymnast. Scand J Med Sci Sports. 1997;7:363–6.
Frizzell JB, Brunet G. Stress changes of the distal radial physis. Can Assoc Radiol J. 1997;48:54–5.
Howe WB, Caine D, Bergman GD, Keeler LW. Wrist pain—gymnastics. Med Sci Sports Exerc. 1997;29:S151.
Brooks TJ. Madelung deformity in a collegiate gymnast: a case report. J Athl Train. 2001;36:170–3.
Barkdell T, Annunziata CC. Acquired Madelung-type deformity in a gymnast. Med Sci Sports Exerc. 2007;39(5):S133–4.
Dwek JR, Cardoso F, Chung CR. MR Imaging of overuse injuries in the skeletally immature gymnasts: spectrum of soft-tissue and osseous lesions in the hand and wrists. Pediatr Radiol. 2009;39:1310–6.
Poletto ED, Pollock AN. Radial epiphysitis (aka Gymnast Wrist). Pediatr Emerg Care. 2012;28(5):484–5.
Ashwell ZR, Richardson ML. Case report: gymnast’s wrist in a 12-year-old female with MRI correlation. Radiol Case Rep. 2019;14:360–4.
Mauck B, Kelly D, Sheffer B, Rambo A, Calandruccio JH. Gymnast’s wrist (distal radial physeal stress syndrome). Orthop Clin N Am. 2020;51:493–7.
Hochholzer T, Schöffl V, Krause R. Finger-epiphysen-verletzungen jugendlicher sportkletterer. Sport Orthop Traumatol. 1997;13:100–3.
Chell J, Stevens K, Preston B, Davis TRC. Bilateral fractures of the middle phalanx of the middle finger in an adolescent climber. Am J Sports Med. 1999;27:817–9.
Bayer T, Schöffl VR, Lenhart M, Herold T. Epiphyseal stress fractures of finger phalanges in adolescent climbing athletes: a 3.0-Teslas magnetic resonance imaging evaluation. Skelet Radiol. 2013;42:1521–5.
Schöffl V, Popp D, Kupper T, Schöffl I. Injury trends in rock climbers: evaluation of a case series of 911 injuries between 2009–2012. Wildern Environ Med. 2015;26:62–7.
Desaldeleer AS, Le Nen D. Bilateral fracture of the base of the middle phalanx in a climber: literature review and a case report. Orthop Traumatol Surg Res. 2016;102(3):409–11.
El-Sheikh Y, Lutter C, Schöffl I, Schöffl V. Surgical management of proximal interphalangeal joint repetitive stress epiphyseal fracture nonunion in elite sport climbers. J Hand Surg Am. 2018;43(6):572.e1-572.e5. https://doi.org/10.1016/j.jhsa.2017.10.009.
Halsey T, Johnson M, Jones G. Epiphyseal stress fractures of the fingers in an adolescent climber: a potential “Maslow’s Hammer” in terms of clinical reasoning. Curr Sports Med Rep. 2019;18:431–3.
Attkiss KJ, Bunckle HJ. Physeal growth arrest of the distal phalanx of the thumb in an adolescent pianist: a case report. J Hand Surg. 1998;23A:532–5.
Schoffl V, Hochholzer T, Winkerlmann H, Strecker W. Pulley injuries in rock climbers. Wildern Environ Med. 2003;41:94–100
Quaine F, Vigouroux L, Martin L. Effect of simulated rock climbing finger postures on force sharing among the fingers. Clin Biomech. 2003;18:365–8.
Lutter C, Tischer T, Hotfiel T, Frank L, Enz A, Simon N, et al. Current trends in sport climbing injuries after the inclusion into the Olympic program. Analysis of 633 injuries within the years 2017/2018. MLTJ. 2020;2:201–10.
Sato T, Shinozaki T, Fukudo T, Watanabe H, Aoki J, Yanagawa T, et al. Atypical growth plate closure: a possible chronic Salter and Harris type V injury. J Pediatr Orthop. 2002;11:155–8.
Domzalski M, Mackenzie W. Growth arrest of the proximal tibial physis with recurvatum and valgus deformity of the knee. Knee. 2009;16:412–6.
Wall EJ. Knee injury: gymnastics. Med Sci Sports Exerc. 1997;29(suppl):S152.
Blatnik TR, Briskin S. Bilateral knee pain in a high-level gymnast. Clin J Sport Med. 2013;23:77–9.
Godshall RW, Hansen CA, Rising DC. Stress fractures through the distal femoral epiphysis in athletes. A previously unreported entity. Am J Sports Med. 1981;9:114–6.
Borders H. Physeal stress injury. Pediatr Adolesc MSK MRI, J Herman Kan, pp. 78–83.
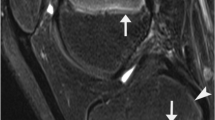
Tony G, Charron A, Tins B, Lalam R, Tyrrell PNM, Singh J, et al. Intra-epiphyseal stress injury of the proximal tibial epiphysis: preliminary experience of magnetic resonance imaging findings. Eur J Radiol. 2014;83:2051–7.
Ehara S. Physeal stress injury to the knee. AJR. 2006;187:W554.
Nanni M, Butt S, Mansour R. Stress-induced Salter–Harris I growth plate injury of the proximal tibia: first report. Skelet Radiol. 2005;34:405–10.
Cahill BR. Stress fracture of the proximal tibial epiphysis: a case report. Am J Sports Med. 1977;5:186–7.
Dempewolf M, Kwan K, Sherman B, Schlechter J. Youth kicker’s knee: lateral distal femoral hemi-physeal arrest secondary to chronic repetitive microtrauma. J Am Acad Orthop Surg. 2019;3:1–6.
Weber PC. Salter–Harris type II stress fracture in a young athlete. Orthopaedics. 1988;11:309–11.
Kadel NJ, Goldstein J, Hewberg AH, Trempman E. Salter–Harris stress fracture of the proximal first metatarsal: a case report. Foot Ankle Intern. 2001;22:252–5.
Shybut TB, Rose DJ, Strongwater AM. Second metatarsal physeal arrest in an adolescent Flamenco dancer: a case report. Foot Ankle Int. 2008;29:859–62.
Bernholdt DL, Garzon-Muvdi J, Chhabra A, McFarland EG. Stress fracture of the distal tibial physis in an adolescent recreational dancer. Am J Sports Med. 2013;41:1649–52.
Csonka A, Sikarinkul E, Gargyan I, Boa K, Varga E. Operative management of bilateral Salter–Harris type III fractures of the proximal phalanges of the great toes of a 10-year-old female ballet dancer: a case report. J Pediatr Orthop B. 2016;25:393–6.
Shah S. Premature growth plate closure in a ballet dancer en Pointe. Clin J Sport Med. 2017;27(5):e69–71.
Wall EJ. Growth plate overuse syndrome of the ankle in athletes. Med Sci Sports Exerc. 1997;5:299.
Percy EC, Gamble FO. An epiphyseal stress fracture of the foot and shin splints in an anomalous calf muscle in a runner. Br J Sports Med. 1980;14:110–3.
Schapiro A, Laor T. ‘Soccer toe:’ Chronic physeal injury of the great toe metatarsal in a skeletally immature child—a case report. SA J Radiol. 2020;24(1):1834. https://doi.org/10.4102/sajr.v24i1.1834.
Caine D, Knutzen K, Howe W, Keeler L, Sheppard L, Heinrichs D, et al. A three-year epidemiological study of injuries affecting young female gymnasts. Phys Ther Sport. 2003;4:10–23.
DiFiori JP, Caine DJ, Malina RM. Wrist pain, distal radial physeal injury, and ulnar variance in the young gymnast. Am J Sports Med. 2006;34:840–9.
Bejjami FJ, Halpern N, Pio A, Dominguez R, Voloshin A, Frankel VH. Musculoskeletal demands on Flamenco dancers: a clinical and biomechanical study. Foot Ankle. 1988;8:254–6.
Torg JS, Pollack H, Sweterlitsch P. The effect of competitive pitching on the shoulders and elbows of baseball players. Pediatrics. 1972;49:267–72.
Kanematsu Y, Matsuura T, Kashiwaguchi S, Iwase T, Suzue N, Iwame T, et al. Epidemiology of shoulder injuries in young baseball players and grading of radiologic findings of Little Leaguer’s shoulder. J Med Investig. 2015;62:123–5.
Pennock AT, Dwek J, Levy E, Stearns P, Manning J, Dennis MM, et al. Shoulder MRI abnormalities in asymptomatic little league baseball players. Orthop J Sports Med. 2018;6(2):2325967118756825.
Zhang C, Shen S, Zhang W, Qiu L, Qingying W, Wang F, et al. Effect of long-term diving on the morphology and growth of the distal radial epiphyseal plate of young divers: a magnetic resonance imaging study. Clin J Sports Med. 2019;29(4):312–7.
Auberge T, Zenny JC, Duvallet A, Godefroy D, Horreard P, Chevrot A. Study of bone maturation and osteo-articular lesions in top level sportsmen: a review of 105 cases. J Radiol (Paris). 1984;65:555–61.
Szot Z, Boron Z, Galaj Z. Overloading changes in the motor system occurring in elite gymnasts. Int J Sports Med. 1985;6:36–40.
Caine D, Roy S, Singer KM, Broekhoff J. Stress changes of the distal radial growth plate. A radiographic survey of 60 young competitive gymnasts and an epidemiologic review of the related literature. Am J Sports Med. 1992;20:290–8.
DeSmet L, Claessons A, Lefevre J, Beunen J. Gymnast wrist: an epidemiological survey of the ulnar variance in elite female gymnasts. Am J Sports Med. 1994;22:846–50.
Chang CY, Shih C, Penn IW, Tiu CM, Chang T, Wu JJ. Wrist injuries in adolescent gymnasts of a Chinese opera school: radiographic survey. Radiology. 1995;195:861–4.
DiFiori JP, Puffer JC, Mandelbaum BR, Dorey F. Distal radial growth plate injury and positive ulnar variance in non-elite gymnasts. Am J Sports Med. 1997;25:763–8.
DiFiori JP, Puffer JP, Aish B, Dorey F. Wrist pain, distal radial physeal injury, and ulnar variance in young gymnasts: does a relationship exist? Am J Sports Med. 2002;30:879–85.
Guerra MRV, Estelles JRD, Abdouni YA, Falcochio DF, Rosa JRP, Catani LH. Frequency of wrist growth plate injury in young gymnasts at a training center. Acta Orthop Bras. 2016;24:204–7.
Kraan RBJ, Kox LS, Mens MA, Kuijer PPFM, Maas M. Damage of the distal radial physis in young gymnasts: can three-dimensional assessment of physeal volume on MRI serve as a biomarker? Eur Radiol. 2019;29:6364–71.
Kraan RBJ, Kox LS, Oostra RJ, Kuijer PPFM, Maas M. The distal radial physis: exploring normal anatomy on MRI enables interpretation of stress related changes in young gymnasts. Eur J Sport Sci. 2020;20:1197–205.
Schlegel C, Buchler U, Kriemler S. Finger injuries of elite rock climbers. Schweizerische Zeitschrift fur Sportsmeizin und Sportstraumatologies. 2002;50(1):7–10.
Schöffl V, Hochholzer T, Imhoff A. Radiographic changes in the hands and fingers of young, high-level climbers. Am J Sports Med. 2004;32(7):1688–94.
Garcia K, Jarmillo D, Rubesova E. Ultrasound evaluation of stress injuries and physiological adaptations in the fingers of adolescent competitive rock climbers. Pediatr Radiol. 2018;48:366–73.
Bartschi N, Scheibler A, Schweizer A. Symptomatic epiphyseal sprains and stress fractures of the finger phalanges in adolescent sport climbers. Hand Surg Rehab. 2019;38:251–6.
Meyers RN, Howell DR, Provance AJ. The association of finger growth plate injury history and speed climbing in youth competition climbers. Wilderness Environ Med. 2020;17:812.
Sabato T, Caine D. Epidemiology of injury in community club and youth sports organizations. In: Caine D, Purcell L, editors. Injury in pediatric and adolescent sport: epidemiology, treatment and prevention. Switzerland: Springer Publishers; 2006.
Caine D, Caine C, Maffulli N. Incidence and distribution of pediatric sport-related injuries. Clin J Sport Med. 2006;16:501–14.
Holt JB, Stearns PH, Bastrom TP, Dennis MM, Dwek JR, Pennock AT. The curse of the all-star team: a single-season prospective shoulder MRI study of Little League baseball players. J Pediatr Orthop. 2020;40(1):e19-24.
Lishen Q, Jianhua O. Epiphyseal injury in gymnasts. Chin J Sports Med. 1983;2:7–12.
Caine D, Cochrane B, Caine C, Zemper E. An epidemiological investigation of injuries affecting young competitive female gymnasts. Am J Sports Med. 1989;17:811–20.
Dixon M, Fricker P. Injuries to elite gymnasts over 10 years. Med Sci Sports Exerc. 1993;25:1322–9.
Schöffl V, Hochholzer T, Imhoff A, Schöffl L. Radiographic adaptations to the stress of high-level rock climbing in junior athletes: a 5-year longitudinal study of the German junior national team and a group of rectreational climbers. Am J Sports Med. 2007;35(1):86–92.
Knowles SB, Marshall SW, Guskiewicz KM. Issues in estimating risks and rates in sports injury research. J Athl Train. 2006;41:207–15.
Materne O, Chamari K, Farooq A, Weir A, Hölmich P, Bahr R, et al. Injury incidence and burden in a youth elite football academy: a four-season prospective study of 551 players aged from under 9 to under 19 years. Br J Sports Med. 2020. https://doi.org/10.1136/bjsports-2020-102859.
Bahr R, Clarsen B, Derman W, Dvorak J, Emery CA, Finch CF, et al. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE Extension for Sport Injury and Illness Surveillance (STROBE-SIIS)). Br J Sports Med. 2020;54:372–89.
Micheli LJ, Klein JD. Sports injuries in children and adolescents. Br J Sports Med. 1991;25:6–9.
Tipton CM, Matthes RD, Maynard JA. Influence of chronic exercise on rat bones. Med Sci Sports Exerc. 1972;4:55.
Kiiskinen A. Physical training and connective tissues in young mice: physical properties of Achilles tendons and long bones. Growth. 1977;41:123–37.
Simon MR. The effects of dynamic loading on the growth of epiphyseal cartilage in the rat. Acta Anat. 1978;102:176–83.
Matsuda JJ, Zernicke RF, Vailas AC, Barnard RJ. Structural and mechanical adaptation of immature bone to strenuous exercise. J Appl Physiol. 1986;60:2028–34.
Friberg O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine. 1983;8:643–51.
McCaw ST, Bates BT. Biomechanical implications of mild leg length inequality. Br J Sports Med. 1991;25:10–3.
Morscher E. Etiology and pathophysiology of leg length discrepancies. Prog Orthop Surg. 1977;1:9–19.
Golightly YM, Allen KD, Helmick CG, Schwartz TA, Renner JB, Jordan JM. Hazard of incident and progressive knee and hip radiographic osteoarthritis and chronic joint symptoms in individuals with and without limb length inequality. J Rheumatol. 2010;3(7):2133–40.
Caine DJ, Golightly YM. Osteoarthritis as an outcome of paediatric sport: an epidemiological perspective. Br J Sport Med. 2011;45:298–303.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dennis Caine, Rachel Meyers, Jie Nguyen, Volker Schöffl, and Nicola Maffulli declare that they have no competing interests.
Funding
No sources of funding were used to assist in the preparation of this article.
Authorship contributions
DC wrote the first draft of the manuscript. RM assisted with the systematic search and retrieval of the literature following PRISMA guidelines. She also developed the PRISMA flowchart. VS and NM provided clinical interpretation of case studies reviewed and assisted with the development of the summary tables. JN provided imaging and clinical interpretation of case studies and assisted with the development of the summary and supplementary tables. RM, JN, VS, and NM assisted with revisions of the original manuscript. All authors read and approved the final manuscript.
Data availability statement
Supplementary information in the form of six summary tables (Supplementary Information Tables S1–S6) is available to authorized users [see title page for information] or from the author on request. These summary tables correspond to results discussed in Sects. 3.2.1–3.2.6.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Caine, D., Meyers, R., Nguyen, J. et al. Primary Periphyseal Stress Injuries in Young Athletes: A Systematic Review. Sports Med 52, 741–772 (2022). https://doi.org/10.1007/s40279-021-01511-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-021-01511-z