Abstract
Background
Foam rolling (FR) has been demonstrated to acutely enhance joint range of motion (ROM). However, data syntheses pooling the effect sizes across studies are scarce. It is, furthermore, unknown which moderators affect the treatment outcome.
Objective
To quantify the immediate effects of FR on ROM in healthy adults.
Methods
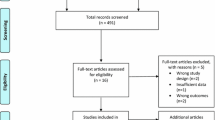
A multilevel meta-analysis with a robust random effects meta-regression model was used to pool the standardized mean differences (SMD) between FR and no-exercise (NEX) as well as FR and stretching. The influence of the possible effect modifiers treatment duration, speed, targeted muscle, testing mode (active/passive ROM), sex, BMI, and study design was examined in a moderator analysis.
Results
Twenty-six trials with high methodological quality (PEDro scale) were identified. Compared to NEX, FR had a large positive effect on ROM (SMD: 0.74, 95% CI 0.42–1.01, p = 0.0002), but was not superior to stretching (SMD: − 0.02, 95% CI − 0.73 to 0.69, p = 0.95). Although the few individual study findings suggest that FR with vibration may be more effective than NEX or FR without vibration, the pooled results did not reveal significant differences (SMD: 6.75, 95% CI − 76.4 to 89.9, p = 0.49 and SMD: 0.66, 95% CI − 1.5 to 2.8, p = 0.32). According to the moderator analysis, most potential effect modifiers (e.g., BMI, speed or duration) do not have a significant impact (p > 0.05) but FR may be less effective in men (p < 0.05).
Conclusion
FR represents an effective method to induce acute improvements in joint ROM. The impact of moderators should be further elucidated in future research.





Similar content being viewed by others
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Simenz CJ, Dugan CA, Ebben WP. Strength and conditioning practices of national basketball association strength and conditioning coaches. J Strength Cond Res. 2005;19:495–504.
Van Baar ME, Dekker J, Bosveld W. A survey of physical therapy goals and interventions for patients with back and knee pain. Phys Ther. 1998;78:33–42.
Roebroeck ME, Dekker J, Oostendorp RA, Bosveld W. Physiotherapy for patients with lateral ankle sprains: a prospective survey of practice patterns in Dutch primary health care. Physiotheraphy. 1998;84:421–32.
Wilke J, Niederer D, Vogt L, Banzer W. Head coaches’ attitudes towards injury prevention and use of related methods in basketball: a survey. Phys Ther Sport. 2018;32:133–9.
Harvey L, Herbert R, Crosbie J. Does stretching induce lasting increases in joint ROM? A systematic review. Physiother Res Int. 2002;7:1–13.
Decoster LC, Cleland J, Altieri C, et al. The effects of hamstring stretching on range of motion: a systematic literature review. Orthop Sports Phys Ther. 2005;35:377–87.
Radford JA, Burns J, Buchbinder R, et al. Does stretching increase ankle dorsiflexion range of motion? A systematic review. Br J Sports Med. 2006;40:870–5.
Medeiros DM, Cini A, Sbruzzi G, et al. Influence of static stretching on hamstring flexibility in healthy young adults: systematic review and meta-analysis. Physiother Theory Pract. 2016;32:438–45.
Behm DG, Blazevich AJ, Kay AD, McHugh M. Systematic review: acute effects of muscle stretching on physical performance, range of motion and injury incidence in healthy active individuals. Appl Physiol Nutr Metab. 2016;40(1):1–11.
Simic L, Sarabon N, Markovic G. Does pre-exercise stretching inhibit maximal muscular performance? A meta-analytical review. Scand J Med Sci Sports. 2013;23:131–48.
Cheatham SW. Roller massage: a descriptive survey of allied health professionals. J Sport Rehabil. 2018. https://doi.org/10.1123/jsr.2017-0366.
Kalichman L, Ben David C. Effect of self-myofascial release on myofascial pain, muscle flexibility, and strength: a narrative review. J Bodyw Mov Ther. 2017;21:446–51.
Cheatham SW, Kolber MJ, Cain M, et al. The effects of self-myofascial release using a foam roll or roller massager on joint range of motion, muscle recovery, and performance: a systematic review. Int J Sports Phys Ther. 2015;10:827–38.
Schoeder AN, Best TM. Is self myofascial release an effective preexercise and recovery strategy? A literature review. Curr Sports Med Rep. 2015;14:200–8.
Beardley C, Skarabot J. Effects of self-myofascial release: a systematic review. J Bodyw Mov Ther. 2015;19:747–58.
Wiewelhove T, Döweling A, Schneider C, et al. A meta-analysis of the effects of foam rolling on performance and recovery. Front Physiol. 2019. https://doi.org/10.3389/fphys.2019.00376.
Madoni SN, Costa PB, Coburn JW, et al. Effects of foam rolling on range of motion, peak torque, muscle activation, and the hamstrings-to-quadriceps strength ratios. J Strength Cond Res. 2018;32:1821–30.
Smith JC, Pridgeon B, Hall MG. Acute effect of foam rolling and dynamic stretching on flexibility and jump height. J Strength Cond Res. 2018;32:2209–15.
Lee CL, Chu IH, Chang WD, et al. Comparison of vibration rolling, nonvibration rolling, and static stretching as a warm-up exercise on flexibility, joint proprioception, muscle strength, and balance in young adults. J Sport Sci. 2018;36:2575–82.
García-Gutiérrez MT, Guillén-Rogel P, Cochrane DJ, et al. Cross transfer acute effects of foam rolling with vibration on ankle dorsiflexion range of motion. J Musculoskel Neuron Interact. 2018;18:262–7.
MacGregor LJ, Fairweather MM, Bennett RM, et al. The effect of foam rolling for three consecutive days on muscular efficiency and range of motion. Sports Med Open. 2018;4:26.
Hall MG, Smith JC. The effects of an acute bout of foam rolling on hip range of motion on different tissues. Int J Sports Phys Ther. 2018;13:652–60.
Young JD, Spence AJ, Power G, et al. The addition of transcutaneous electrical nerve stimulation with roller massage alone or in combination did not increase pain tolerance or range of motion. J Sport Sci Med. 2018;17:525–32.
Wilke J, Niemeyer P, Niederer D, et al. Influence of foam rolling velocity on knee range of motion and tissue stiffness: a randomized controlled crossover trial. J Sport Rehabil. 2019. https://doi.org/10.1123/jsr.2018-0041.
Laudner K. Acute effects of pectoralis minor self mobilization on shoulder motion and posture: a blinded and randomized placebo-controlled study in asymptomatic individuals. J Sport Rehabil. 2019. https://doi.org/10.1123/jsr.2018-0220.
Smith JC, Washell BR, Aini MF, et al. Effects of static stretching and foam rolling on ankle dorsiflexion range of motion. Med Sci Sports Exerc. 2019. https://doi.org/10.1249/MSS.0000000000001964.
Somers K, Aune D, Horten A, et al. Acute effects of gastrocnemius/soleus self-myofascial release vs. dynamic stretching on closed chain dorsiflexion. J Sport Rehabil. 2019. https://doi.org/10.1123/jsr.2018-0199.
Cheatham SW, Stull KR, Kolber MJ. Comparison of a vibration roller and a nonvibration roller intervention on knee range of motion and pressure pain threshold: a randomized controlled trial. J Sport Rehabil. 2019;28:39–45.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Wager E, Wiffen PJ. Ethical issues in preparing and publishing systematic reviews. J Evid Based Med. 2011;4:130–4.
Wilke J, Krause F, Vogt L, et al. What is evidence-based about myofascial chains: a systematic review. Arch Phys Med Rehabil. 2016;97:454–61.
Krause F, Wilke J, Vogt L, et al. Intermuscular force transmission along myofascial chains: a systematic review. J Anat. 2016;228:910–8.
Wilke J, Giesche F, Klier K, et al. Acute effects of resistance exercise on cognitive function in healthy adults: a systematic review with multilevel meta-analysis. Sports Med. 2019. https://doi.org/10.1007/s40279-019-01085-x.
Horsley T, Dingwall O, Sampson M. Checking reference lists to find additional studies for systematic reviews. Cochrane Database Syst Rev. 2011;73:505.
Rosenthal R. Meta-analytic procedures for social research. Newbury Park: Sage Publications; 1993.
Curtin F, Altman DG, Elbourne D. Meta-analysis combining parallel and cross-over clinical trials I: continuous outcomes. Stat Med. 2002;21:2131–44.
Eiling E, Bryant AL, Petersen W, Murphy A, Hohmann E. Effects of menstrual-cycle hormone fluctuations on musculotendinous stiffness and knee joint laxity. Knee Surg Sports Traumatol Arthrosc. 2007;15:126–32.
Hedges LV, Tipton E, Johnson MC. Robust variance estimation in meta-regression with dependent effect size estimates. Res Synth Methods. 2010;1:39–65.
Northey JM, Cherbuin, Pumpa NL, et al. Exercise interventions for cognitive function in adults older than 50: a systematic review with meta-analysis. Br J Sports Med. 2018;52:154–60.
Faraone SV. Interpreting estimates of treatment effects. P&T. 2008;33:700–3.
Fisher Z, Tipton E. Robumeta. An r package for robust variance estimation in meta-analysis. https://arxiv.org/abs/1503.02220.
Maher CG, Sherrington C, Herbert RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–21.
Foley CF, Bhogal SK, Teasell RW, et al. Estimates of quality and reliability with the physiotherapy evidence-based database scale to assess the methodology of randomized controlled trials of pharmacological and nonpharmacological interventions. Phys Ther. 2006;86(6):817–24.
de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55:129–33.
MacDonald GZ, Penney MD, Mullaley ME, et al. An acute bout of self-myofascial release increases range of motion without a subsequent decrease in muscle activation or force. J Strength Cond Res. 2013;27:812–21.
Sullivan KM, Silvey DB, Button DC, et al. Roller-massager application to the hamstrings increases sit-and-reach range of motion within five to ten seconds without performance impairments. Int J Sports Phys Ther. 2013;8:228–36.
Halperin I, Aboodarda SJ, Button DC, et al. Roller massager improves range of motion of plantar flexor muscles without subsequent decreases in force parameters. Int J Sports Phys Ther. 2014;9:92–102.
Mohr AR, Long BC, Goad CL. Effect of foam rolling and static stretching on passive hip-flexion range of motion. J Sport Rehabil. 2014;23:296–9.
Bushell JE, Dawson SM, Webster MM. Clinical relevance of foam rolling on hip extension angle in a functional lunge position. J Strength Cond Res. 2015;29:2397–403.
Skarabot J, Beardsley C, Stirn I. Comparing the effects of self-myofascial release with static stretching on ankle range of motion in adolescent athletes. Int J Sports Phys Ther. 2015;10:203–11.
Bradbury-Squires DJ, Notfall JC, Sullivan K, et al. Roller massager application to the quadriceps and knee-joint range of motion and neuromuscular efficiciency during a lunge. J Athl Train. 2015;50:133–40.
Murray AM, Jones TW, Horobeanu C, et al. Sixty seconds of foam rolling does not affect functional flexibility or change muscle termperature in adolescent athletes. Int J Phys Ther. 2016;11:765–75.
Kelly S, Beardsley C. Specific and cross-over effects of foam rolling on ankle dorsiflexion range of motion. Int J Sports Phys Ther. 2016;11:544–51.
Su H, Chang NJ, Wu WL, et al. Acute effects of foam rolling, static stretching, and dynamic stretching during warm-ups on muscular flexibility and strength in young adults. J Sport Rehabil. 2017;26:469–77.
Behara B, Jacobson BH. Acute effects of deep tissue foam rolling and dynamic stretching on muscular strength, power, and flexibility in division I linemen. J Strength Cond Res. 2017;31:888–92.
Morales-Artacho AJ, Lacourpaille L, Guilhem G. Effects of warm-up on hamstring muscle stiffness: cycling vs foam rolling. Scand J Med Sci Sports. 2017;1:1–11.
Phillips J, Diggin D, King DL, et al. Effect of varying self-myofascial release duration on subsequent athletic performance. J Strength Cond Res. 2018;10:1–8.
Fairall RR, Cabell L, Boergers RJ, et al. Acute effects of SMR and static stretching in overhead athletes with GIRD. J Strength Cond Res. 2017;21(648):652.
Behm DG, Wilke J. Do self-myofascial release devices release myofascia? Rolling mechanisms: a narrative review. Sports Med. 2019 (under review).
Hotfiel T, Swoboda B, Krinner S, Grim C, Engelhardt M, Uder M, et al. Acute effects of lateral thigh foam rolling on arterial tissue perfusion determined by spectral doppler and power doppler ultrasound. J Strength Cond Res. 2017;31(4):893–900.
Okamoto T, Masuhara M, Ikuta K. Acute effects of self-myofascial release using a foam roller on arterial function. J Strength Cond Res. 2014;28(1):69–73.
Heiss RM, Huettel M, Lutter C, Forst R, Hoppe M, Freiwald J, Roemer FW, Hotfiel T. Evaluation of tissue stiffness in athletes with different experience in foam rolling assessed by acoustic radiation force impulse elastography. Semin Musculoskelet Radiol. 2019;23:S1–6.
Young JD, Spence AJ, Behm DG. Roller massage decreases spinal excitability to the soleus. J Appl Physiol (1985). 2018;124(4):950–9. https://doi.org/10.1152/japplphysiol.00732.2017.
Aboodarda SJ, Spence AJ, Button DC. Pain pressure threshold of a muscle tender spot increases following local and non-local rolling massage. BMC Musculoskelet Disord. 2015;16:265. https://doi.org/10.1186/s12891-015-0729-5.
Cavanaugh MT, Doweling A, Young JD, Quigley PJ, Hodgson DD, Whitten JH, et al. An acute session of roller massage prolongs voluntary torque development and diminishes evoked pain. Eur J Appl Physiol. 2016. https://doi.org/10.1007/s00421-016-3503-y.
Schleip R. Fascial plasticity—a new neurobiological explanation: part 2. J Bodyw Mov Ther. 2003;7:104–16.
Schleip R. Fascial plasticity—a new neurobiological explanation: part I. J Bodyw Mov Ther. 2003;7:11–9.
Wu G, Ekedahl R, Stark B, Carlstedt T, Nilsson B, Hallin RG. Clustering of Pacinian corpuscle afferent fibres in the human median nerve. Experim Brain Res. 1999;126:399–409.
Weerapong P, Hume PA, Kolt GS. The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med. 2005;35:235–56.
Lastova K, Nordvall M, Walter-Edwards M, Allnutt, Wong A. Cardiac autonomic and blood pressure responses to an acute foam rolling session. J Strength Cond Res. 2018;32(10):2825–30.
Mitchell JH, Schmidt RF. Cardiovascular reflex control by afferent fibers from skeletal muscle receptors. Bethesda: American Physiological Society; 1977.
Kostopoulos DN, Arthur J, Ingber RS, Larkin RW. Reduction of spontaneous electrical activity and pain perception of trigger points in the upper trapezius muscle through trigger point compression and passive stretching. J Musculoskelet Pain. 2008;16:266–78.
Pearcey GE, Bradbury-Squires DJ, Kawamoto JE, Drinkwater EJ, Behm DG, Button DC. Foam rolling for delayed-onset muscle soreness and recovery of dynamic performance measures. J Athl Train. 2015;50:5–13.
Cabido CE, Bergamini JC, Andrade AG, Lima FV, Menzel HJ, Chagas MH. Acute effect of constant torque and angle stretching on range of motion, muscle passive properties, and stretch discomfort perception. J Strength Cond Res. 2014;28(4):1050–7.
Hoge KM, Ryan ED, Costa PB, Herda TJ, Walter AA, Stout JR, Cramer JT. Gender differences in musculotendinous stiffness and range of motion after an acute bout of stretching. J Strength Cond Res. 2010;24(10):2618–26.
Etnyre BR, Lee EJ. Chronic and acute flexibility of men and women using three different stretching techniques. Res Q Exerc Sport. 1988;59(3):222–8.
Cipriani DJ, Terry ME, Haines MA, Tabibnia AP, Lyssanova O. Effect of stretch frequency and sex on the rate of gain and rate of loss in muscle flexibility during a hamstring–stretching program: a randomized single-blind longitudinal study. J Strength Cond Res. 2012;26(8):2119–29.
Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, Carpenter J, Rücker G, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002.
Zwetsloot PP, van der Naald M, Sena ES, Howells DW, IntHout J, De Groot JA, Chamuleau SA, MacLeod MR, Wever KE. Standardized mean differences cause funnel plot distortion in publication bias assessments. Elife. 2017. https://doi.org/10.7554/eLife.24260.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No sources of funding were used to assist in the preparation of this article.
Conflict of Interest
Jan Wilke, Anna-Lena Müller, Florian Giesche, Gerard Powers, Hamid Ahmedi and David Behm declare that they have no conflicts of interest relevant to the content of this review.
Rights and permissions
About this article
Cite this article
Wilke, J., Müller, AL., Giesche, F. et al. Acute Effects of Foam Rolling on Range of Motion in Healthy Adults: A Systematic Review with Multilevel Meta-analysis. Sports Med 50, 387–402 (2020). https://doi.org/10.1007/s40279-019-01205-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-019-01205-7