Abstract
Background
Several studies have examined the effects of balance training in elderly individuals following total knee arthroplasty (TKA), although findings appear to be equivocal.
Objectives
This systematic review and meta-analysis examined the effects of balance training on walking capacity, balance-specific performance and other functional outcome measures in elderly individuals following TKA.
Methods
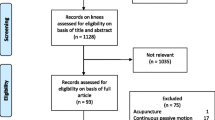
Data sources: Pubmed, PEDro, Cinahl, SportDiscus, Scopus. Eligibility criteria: Data were aggregated following the population-intervention-comparison-outcome (PICO) principles. Eligibility criteria included: (1) randomised controlled trials; (2) studies with comparative groups; (3) training interventions were incorporated post-TKA; and (4) outcome measures included walking capacity, balance-specific performance measures, subjective measures of physical function and pain and knee range-of-motion. Participants: Elderly individuals (65 + years) who underwent total knee arthroplasty. Interventions: Balance interventions that consisted of balance exercises, which were compared to control interventions that did not involve balance exercises, or to a lesser extent. Participants also undertook usual physiotherapy care in conjunction with either the balance and/or control intervention. The intervention duration ranged from 4 to 32 weeks with outcome measures reported immediately following the intervention. Of these, four studies also reported follow-up measures ranging from 6 to 12 months post-interventions. Study appraisal: PEDro scale.
Synthesis methods
Quantitative analysis was conducted by generating forest plots to report on standardised mean differences (SMD; i.e. effect size), test statistics for statistical significance (i.e. Z values) and inter-trial heterogeneity by inspecting I2. A meta-regression was also conducted to determine whether training duration predicted the magnitude of SMD.
Results
Balance training exhibited significantly greater improvement in walking capacity (SMD = 0.57; Z = 6.30; P < 0.001; I2 = 35%), balance-specific performance measures (SMD = 1.19; Z = 7.33; P < 0.001; I2 = 0%) and subjective measures of physical function (SMD = 0.46; Z = 4.19; P < 0.001; I2 = 0%) compared to conventional training immediately post-intervention. However, there were no differences in subjective measures of pain (SMD = 0.77; Z = 1.63; P > 0.05; I2 = 95%) and knee range-of-motion (SMD = 0.05; Z = 0.39; P > 0.05; I2 = 1%) between interventions. At the 6- to 12-month follow-up period, improvement in combined measures of walking capacity and balance performance (SMD = 041; Z = 3.55; P < 0.001; I2 = 0%) were significantly greater for balance training compared to conventional training, although no differences were observed for subjective measures of physical function and pain (SMD = 0.26; Z = 2.09; P > 0.05; I2 = 0%). Finally, the training duration significantly predicted subjective measures of pain and physical function (r2 = 0.85; standardised β = 0.92; P < 0.001), although this was not observed for walking capacity and balance-specific performance measures (r2 = 0.02; standardised β = 0.13; P = 0.48).
Limitations
A number of outcome measures indicated high inter-trial heterogeneity and only articles published in English were included.
Conclusion
Balance training improved walking capacity, balance-specific performance and functional outcome measures for elderly individuals following TKA. These findings may improve clinical decision-making for appropriate post-TKA exercise prescription to minimise falls risks and optimise physical function.






Similar content being viewed by others
References
Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185–99. https://doi.org/10.1093/bmb/lds038.
Mont MA, Banerjee S, Jauregui JJ, Cherian JJ, Kapadia BH. What outcome metrics do the various knee rating systems for assessment of outcomes following total kknee athroplasty measure? A systematic review of literature. Surg Tehnol Int. 2015;26:267–74.
Moutzouri M, Gleeson N, Billis E, Tsepis E, Panoutsopoulou I, Gliatis J. The effect of total knee arthroplasty on patients’ balance and incidence of falls: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25(11):3439–51. https://doi.org/10.1007/s00167-016-4355-z.
Tjon SS, Geurts AC, van’t Pad Bosch P, Laan RF, Mulder T. Postural control in rheumatoid arthritis patients scheduled for total knee arthroplasty. Arch Phys Med Rehabil. 2000;81(11):1489–93.
Matsumoto H, Okuno M, Nakamura T, Yamamoto K, Hagino H. Fall incidence and risk factors in patients after total knee arthroplasty. Arch Orthop Trauma Surg. 2012;132(4):555–63. https://doi.org/10.1007/s00402-011-1418-y.
Matsumoto T, Kubo S, Sasaki K, Kawakami Y, Oka S, Sasaki H, et al. Acceleration of tendon-bone healing of anterior cruciate ligament graft using autologous ruptured tissue. Am J Sports Med. 2012;40(6):1296–302. https://doi.org/10.1177/0363546512439026.
Takura T, Miki K. The future of medical reimbursement for orthopedic surgery in Japan from the viewpoint of the health economy. J Orthop Sci. 2016;21(3):273–81. https://doi.org/10.1016/j.jos.2016.02.007.
Kramer JF, Speechley M, Bourne R, Rorabeck C, Vaz M. Comparison of clinic- and home-based rehabilitation programs after total knee arthroplasty. Clin Orthop Relat Res. 2003;410:225–34. https://doi.org/10.1097/01.blo.0000063600.67412.11.
Shepperd S, Harwood D, Jenkinson C, Gray A, Vessey M, Morgan P. Randomised controlled trial comparing hospital at home care with inpatient hospital care. I: three month follow up of health outcomes. BMJ. 1998;316(7147):1786–91.
Walsh MB, Herbold J. Outcome after rehabilitation for total joint replacement at IRF and SNF: a case-controlled comparison. Am J Phys Med Rehabil. 2006;85(1):1–5.
Liao CD, Lin LF, Huang YC, Huang SW, Chou LC, Liou TH. Functional outcomes of outpatient balance training following total knee replacement in patients with knee osteoarthritis: a randomized controlled trial. Clin Rehabil. 2015;29(9):855–67. https://doi.org/10.1177/0269215514564086.
Bruun-Olsen V, Heiberg KE, Wahl AK, Mengshoel AM. The immediate and long-term effects of a walking-skill program compared to usual physiotherapy care in patients who have undergone total knee arthroplasty (TKA): a randomized controlled trial. Disabil Rehabil. 2013;35(23):2008–15. https://doi.org/10.3109/09638288.2013.770084.
Frost H, Lamb SE, Robertson S. A ranodmized controlled trial of exercise to improve mobility and function after elective knee arthroplasty. Feasibility, results and methodological difficulties. Clin Rehabil. 2002;16:200–9.
Johnson AW, Myrer JW, Hunter I, Feland JB, Hopkins JT, Draper DO, et al. Whole-body vibration strengthening compared to traditional strengthening during physical therapy in individuals with total knee arthroplasty. Physiother Theory Pract. 2010;26(4):215–25. https://doi.org/10.3109/09593980902967196.
Liao CD, Liou TH, Huang YY, Huang YC. Effects of balance training on functional outcome after total knee replacement in patients with knee osteoarthritis: a randomized controlled trial. Clin Rehabil. 2013;27(8):697–709. https://doi.org/10.1177/0269215513476722.
Piva SR, Gil AB, Almeida GJ, DiGioia AM 3rd, Levison TJ, Fitzgerald GK. A balance exercise program appears to improve function for patients with total knee arthroplasty: a randomized clinical trial. Phys Ther. 2010;90(6):880–94. https://doi.org/10.2522/ptj.20090150.
Fung V, Ho A, Shaffer J, Chung E, Gomez M. Use of Nintendo Wii FitTM in the rehabilitation of outpatients following total knee replacement: a preliminary randomised controlled trial. Physiotherapy. 2012;98(3):183–8.
Karaman A, Yuksel I, Kinikli GI, Caglar O. Do Pilates-based exercises following total knee arthroplasty improve postural control and quality of life? Physiother Theory Pract. 2017;33(4):289–95.
Roig-Casasus S, Maria Blasco J, Lopez-Bueno L, Blasco-Igual MC. Balance training with a dynamometric platform following total knee replacement: a randomized controlled trial. J Geriatr Phys Ther. 2017. https://doi.org/10.1519/JPT.0000000000000121.
Moutzouri M, Gleeson N, Billis E, Panoutsopoulou I, Gliatis J. What is the effect of sensori-motor training on functional outcome and balance performance of patients’ undergoing TKR? A systematic review. Physiotherapy. 2016;102(2):136–44.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65–94.
Taube W, Gruber M, Beck S, Faist M, Gollhofer A, Schubert M. Cortical and spinal adaptations induced by balance training: correlation between stance stability and corticospinal activation. Acta Physiol (Oxf). 2007;189(4):347–58. https://doi.org/10.1111/j.1365-201X.2007.01665.x.
Kuo AD. An optimal state estimation model of sensory integration in human postural balance. J Neural Eng. 2005;2(3):S235–49. https://doi.org/10.1088/1741-2560/2/3/S07.
Lusardi MM, Fritz S, Middleton A, Allison L, Wingood M, Phillips E, et al. Determining risk of falls in community dwelling older adults: a systematic review and meta-analysis using posttest probability. J Geriatr Phys Ther. 2017;40(1):1–36. https://doi.org/10.1519/JPT.0000000000000099.
Runge M, Hunter G. Determinants of musculoskeletal frailty and the risk of falls in old age. J Musculoskelet Neuronal Interact. 2006;6(2):167–73.
Reider N, Gaul C. Fall risk screening in the elderly: a comparison of the minimal chair height standing ability test and 5-repetition sit-to-stand test. Arch Gerontol Geriatr. 2016;65:133–9. https://doi.org/10.1016/j.archger.2016.03.004.
Komatsu T, Kim KJ, Kaminai T, Okuizumi H, Kamioka H, Okada S, et al. Clinical factors as predictors of the risk of falls and subsequent bone fractures due to osteoporosis in postmenopausal women. J Bone Miner Metab. 2006;24(5):419–24. https://doi.org/10.1007/s00774-006-0704-1.
Alenazi AM, Alshehri MM, Alothman S, Rucker J, Dunning K, D’Silva L, et al. Functional reach, depression scores, and number of medications are associated with number of falls in people with chronic stroke. PM R. 2017. https://doi.org/10.1016/j.pmrj.2017.12.005.
Bello AI, Ababio E, Antwi-Baffoe S, Seidu MA, Adjei DN. Pain, range of motion and activity level as correlates of dynamic balance among elderly people with musculoskeletal disorder. Ghana Med J. 2014;48(4):214–8.
Miner AL, Lingard EA, Wright EA, Sledge CB, Katz JN, Kinemax Outcomes G. Knee range of motion after total knee arthroplasty: how important is this as an outcome measure? J Arthroplasty. 2003;18(3):286–94. https://doi.org/10.1054/arth.2003.50046.
Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6:284–90.
de Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Aust J Physiother. 2009;55(2):129–33.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Deeks J, Higgins JPT. Cochrane handbook for systematic reviews of interventions. Analysing data and undertaking meta-analyses. New Jersey: Wiley-Blackwell; 2008.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: Erlbaum; 1988.
Moffet H, Collet JP, Shapiro SH, Paradis G, Marquis F, Roy L. Effectiveness of intensive rehabilitation on functional ability and quality of life after first total knee arthroplasty: a single-blind randomized controlled trial. Arch Phys Med Rehabil. 2004;85(4):546–56.
Monticone M, Ferrante S, Rocca B, Salvaderi S, Fiorentini R, Restelli M, et al. Home-based functional exercises aimed at managing kinesiophobia contribute to improving disability and quality of life of patients undergoing total knee arthroplasty: a randomized controlled trial. Arch Phys Med Rehabil. 2013;94(2):231–9. https://doi.org/10.1016/j.apmr.2012.10.003.
Piva SR, Almeida GJ, Gil AB, DiGioia AM, Helsel DL, Sowa GA. A comprehensive behavioral and exercise intervention improves physical function and activity participation after total knee replacement—a pilot randomized study. Arthritis Care Res (Hoboken). 2017. https://doi.org/10.1002/acr.23227.
Mistry JB, Elmallah RD, Bhave A, Chughtai M, Cherian JJ, McGinn T, et al. Rehabilitative guidelines after total knee arthroplasty: a review. J Knee Surg. 2016;29(3):201–17. https://doi.org/10.1055/s-0036-1579670.
Bunton EE, Pitney WA, Cappaert TA, Kane AW. The role of limb torque, muscle action and proprioception during closed kinetic chain rehabilitation of the lower extremity. J Athl Train. 1993;28(1):10–20.
Nadeau S, Arsenault AB, Gravel D, Bourbonnais D. Analysis of the clinical factors determining natural and maximal gait speeds in adults with a stroke. Am J Phys Med Rehabil. 1999;78(2):123–30.
Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80(9):896–903.
Judge JO, Schechtman K, Cress E. The relationship between physical performance measures and independence in instrumental activities of daily living. The FICSIT Group. Frailty and Injury: cooperative studies of intervention trials. J Am Geriatr Soc. 1996;44(11):1332–41.
Hagovska M, Olekszyova Z. Relationships between balance control and cognitive functions, gait speed, and activities of daily living. Z Gerontol Geriatr. 2016;49(5):379–85. https://doi.org/10.1007/s00391-015-0955-3.
Swinkels A, Allain TJ. Physical performance tests, self-reported outcomes, and accidental falls before and after total knee arthroplasty: an exploratory study. Physiother Theory Pract. 2013;29(6):432–42. https://doi.org/10.3109/09593985.2012.755590.
Lesinski M, Hortobagyi T, Muehlbauer T, Gollhofer A, Granacher U. Effects of balance training on balance performance in healthy older adults: a systematic review and meta-analysis. Sports Med. 2015;45(12):1721–38. https://doi.org/10.1007/s40279-015-0375-y.
Rahman M, Sakamoto J, Fukui T. Japan’s share of articles in orthopedics. J Orthop Sci. 2002;7(6):607–9. https://doi.org/10.1007/s007760200109.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Data Availability Statement
The mean and standard deviation measures for each effect point is presented in the forest plot. Thus, to avoid repetition, the data set for this review has not been included as a separate file.
Conflict of Interest
Kenji Doma, Jodie Morris and Andrea Grant declare that they have no conflicts of interest.
Study Funding
No financial support was received for the conduct of this study or preparation of this manuscript.
Electronic supplementary material
Below is the link to the electronic supplementary material.
40279_2018_964_MOESM1_ESM.pdf
Online resource 1. Funnel plot of the walk capacity measures. 2MWT – two minute walk test; 6MWT – six minute walk test (PDF 142 kb)
40279_2018_964_MOESM2_ESM.pdf
Online resource 2. Funnel plot of the walking capacity and balance measures during the 6-12 month follow-up period. 6MWT – six minute walk test (PDF 140 kb)
40279_2018_964_MOESM3_ESM.pdf
Online resource 3. Funnel plot of the subjective measures of function and pain during the 6-12 month follow-up period (PDF 186 kb)
40279_2018_964_MOESM4_ESM.pdf
Online resource 4. Funnel plot of the balance measures. BBS – Berg balance scale; SLS TKR EC – single leg stance time for the total knee replacement limb with eyes closed; SLS Non-TKR EC – single leg stance time for the limb without total knee replacement with eyes closed; CSTS – chair sit-to-stand; SLS TKR EO – single leg stance time for the total knee replacement limb with eyes open; SLS Non-TKR EO – single leg stance time for the limb without total knee replacement with eyes opened (PDF 192 kb)
40279_2018_964_MOESM5_ESM.pdf
Online resource 5. Funnel plot of the subjective measures of function and pain and range-of-motion measures (PDF 194 kb)
Rights and permissions
About this article
Cite this article
Doma, K., Grant, A. & Morris, J. The Effects of Balance Training on Balance Performance and Functional Outcome Measures Following Total Knee Arthroplasty: A Systematic Review and Meta-Analysis. Sports Med 48, 2367–2385 (2018). https://doi.org/10.1007/s40279-018-0964-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40279-018-0964-7