Abstract
Background
The rate of events such as recurrent heart failure (HF) hospitalization and death are known to dramatically increase directly after HF hospitalization. Furthermore, the number of HF hospitalizations is associated with irreversible long-term disease progression, which is in turn associated with increased event rates. However, cost-effectiveness models of HF treatments commonly fail to capture both the short- and long-term association between HF hospitalization and events.
Objective
The aim of this study was to provide a decision-analytic model that reflects the short- and long-term association between HF hospitalization and event rates. Furthermore, we assess the impact of omitting these associations.
Methods
We developed a life-time Markov cohort model to evaluate HF treatments, and modeled the short-term impact of HF hospitalization on event rates via a sequence of tunnel states, with transition probabilities following a parametric survival curve. The corresponding long-term impact was modeled via hazard ratios per HF hospitalization. We obtained baseline event rates and utilities from published literature. Subsequently, we assessed, for a hypothetical HF treatment, how omitting the modeled associations (through a simple two-state model) affects incremental quality-adjusted life-years (QALYs).
Results
We developed a model that incorporates both short- and long-term impacts of HF hospitalizations. Based on an assumed treatment effect of a 20% risk reduction for HF hospitalization (and associated reductions in all-cause mortality of 15%), omitting the short-term, the long-term, or both associations resulted in a 5%, 1%, and 22% decrease in QALYs gained, respectively.
Conclusion
For both modeling components, i.e., the short- and long-term implications of HF hospitalization, the impact on incremental outcomes associated with treatment was substantial. Considering these aspects as proposed within this modeling approach better reflects the natural course of this progressive condition and will enhance the evaluation of future HF treatments.






Similar content being viewed by others
References
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018; 392(10159):1789–858.
Ciapponi A, Alcaraz A, Calderon M, et al. Burden of heart failure in Latin America: a systematic review and meta-analysis. Rev Esp Cardiol (Engl Ed). 2016;69(11):1051–60.
Ponikowski P, Anker SD, AlHabib KF, et al. Heart failure: preventing disease and death worldwide. ESC Heart Fail. 2014;1(1):4–25.
Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017;3(1):7–11.
Parsons RW, Liew D, Neville AM, et al. The epidemiology of heart failure in the general Australian community—study of heart failure in the Australian primary carE setting (SHAPE): methods. BMC Public Health. 2020;20(1):648.
Hao G, Wang X, Chen Z, et al. Prevalence of heart failure and left ventricular dysfunction in China: the China Hypertension Survey, 2012–2015. Eur J Heart Fail. 2019;21(11):1329–37.
Lee H, Oh SH, Cho H, Cho HJ, Kang HY. Prevalence and socio-economic burden of heart failure in an aging society of South Korea. BMC Cardiovasc Disord. 2016;16(1):215.
Ambrosy AP, Fonarow GC, Butler J, et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014;63(12):1123–33.
Desai AS, Stevenson LW. Rehospitalization for heart failure: predict or prevent? Circulation. 2012;126(4):501–6.
Ambrosy AP, Hernandez AF, Armstrong PW, et al. The clinical course of health status and association with outcomes in patients hospitalized for heart failure: insights from ASCEND-HF. Eur J Heart Fail. 2016;18(3):306–13.
Jackson SL, Tong X, King RJ, Loustalot F, Hong Y, Ritchey MD. National burden of heart failure events in the United States, 2006 to 2014. Circ Heart Fail. 2018;11(12): e004873.
Levy D, Kenchaiah S, Larson MG, et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002;347(18):1397–402.
Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127(1):e6–245.
Roger VL. Epidemiology of heart failure. Circ Res. 2013;113(6):646–59.
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–200.
Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147-239.
Atherton JJ, Sindone A, De Pasquale CG, et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of heart failure 2018. Med J Aust. 2018;209(8):363–9.
Ezekowitz JA, O’Meara E, McDonald MA, et al. 2017 Comprehensive update of the Canadian Cardiovascular Society guidelines for the management of heart failure. Can J Cardiol. 2017;33(11):1342–433.
Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. J Am Coll Cardiol. 2017;70(6):776–803.
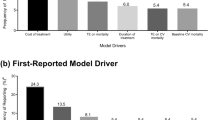
Di Tanna GL, Bychenkova A, O’Neill F, et al. Evaluating cost-effectiveness models for pharmacologic interventions in adults with heart failure: a systematic literature review. Pharmacoeconomics. 2019;37(3):359–89.
Di Tanna GL, Chen S, Bychenkova A, Wirtz HS, Burrows KL, Globe G. Economic evaluations of pharmacological treatments in heart failure patients: a methodological review with a focus on key model drivers. Pharmacoecon Open. 2020;4(3):397–401.
Levy AR, Briggs AH, Demers C, O’Brien BJ. Cost-effectiveness of beta-blocker therapy with metoprolol or with carvedilol for treatment of heart failure in Canada. Am Heart J. 2001;142(3):537–43.
King JB, Shah RU, Bress AP, Nelson RE, Bellows BK. Cost-effectiveness of sacubitril-valsartan combination therapy compared with enalapril for the treatment of heart failure with reduced ejection fraction. JACC Heart Fail. 2016;4(5):392–402.
Gandjour A, Ostwald DA. Sacubitril/valsartan (LCZ696): a novel treatment for heart failure and its estimated cost effectiveness, budget impact, and disease burden reduction in Germany. Pharmacoeconomics. 2018;36(10):1285–96.
McEwan P, Darlington O, McMurray JJV, Jhund PS, Docherty KF, Böhm M, Petrie MC, Bergenheim K, Qin L. Cost-effectiveness of dapagliflozin as a treatment for heart failure with reduced ejection fraction: a multinational health-economic analysis of DAPA-HF. Eur J Heart Fail. 2020;22(11):2147-56. https://doi.org/10.1002/ejhf.1978.
Caraballo C, Desai NR, Mulder H, et al. Clinical implications of the New York Heart Association classification. J Am Heart Assoc. 2019;8(23): e014240.
Thokala P, Dodd P, Baalbaki H, Brennan A, Dixon S, Lowrie K. Developing Markov models from real-world data: a case study of heart failure modeling using administrative data. Value Health. 2020;23(6):743–50.
Gaziano TA, Fonarow GC, Claggett B, et al. Cost-effectiveness analysis of sacubitril/valsartan vs enalapril in patients with heart failure and reduced ejection fraction. JAMA Cardiol. 2016;1(6):666–72.
Gaziano TA, Fonarow GC, Velazquez EJ, Morrow DA, Braunwald E, Solomon SD. Cost-effectiveness of sacubitril-valsartan in hospitalized patients who have heart failure with reduced ejection fraction. JAMA Cardiol. 2020;5(11):1236–44.
McMurray JJ, Packer M, Desai AS, et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014;371(11):993–1004.
Velazquez EJ, Morrow DA, DeVore AD, et al. Angiotensin-neprilysin inhibition in acute decompensated heart failure. N Engl J Med. 2019;380(6):539–48.
Teerlink JR, Diaz R, Felker GM, et al. Omecamtiv mecarbil in chronic heart failure with reduced ejection fraction: rationale and design of GALACTIC-HF. JACC Heart Fail. 2020;8(4):329–40.
Li S, Marcus P, Nunez J, Nunez E, Sanchis J, Levy WC. Validity of the Seattle Heart Failure Model after heart failure hospitalization. ESC Heart Fail. 2019;6(3):509–15.
Vaduganathan M, Claggett BL, Desai AS, et al. Prior heart failure hospitalization, clinical outcomes, and response to sacubitril/valsartan compared with valsartan in HFpEF. J Am Coll Cardiol. 2020;75(3):245–54.
Krumholz HM, Hsieh A, Dreyer RP, Welsh J, Desai NR, Dharmarajan K. Trajectories of risk for specific readmission diagnoses after hospitalization for heart failure, acute myocardial infarction, or pneumonia. PLoS ONE. 2016;11(10): e0160492.
Setoguchi S, Stevenson LW, Schneeweiss S. Repeated hospitalizations predict mortality in the community population with heart failure. Am Heart J. 2007;154(2):260–6.
Cowie MR, Anker SD, Cleland JGF, et al. Improving care for patients with acute heart failure: before, during and after hospitalization. ESC Heart Fail. 2014;1(2):110–45.
Dharmarajan K, Hsieh AF, Kulkarni VT, et al. Trajectories of risk after hospitalization for heart failure, acute myocardial infarction, or pneumonia: retrospective cohort study. BMJ. 2015;350: h411.
Ziaeian B, Fonarow GC. The prevention of hospital readmissions in heart failure. Prog Cardiovasc Dis. 2016;58(4):379–85.
Cheng RK, Cox M, Neely ML, et al. Outcomes in patients with heart failure with preserved, borderline, and reduced ejection fraction in the Medicare population. Am Heart J. 2014;168(5):721–30.
Butt JH, Fosbol EL, Gerds TA, et al. Readmission and death in patients admitted with new-onset versus worsening of chronic heart failure: insights from a nationwide cohort. Eur J Heart Fail. 2020;22(10):1777–85.
McMurray JJV, Trueman D, Hancock E, et al. Cost-effectiveness of sacubitril/valsartan in the treatment of heart failure with reduced ejection fraction. Heart. 2018;104(12):1006–13.
Di Tanna GL, Urbich M, Wirtz HS, et al. Health state utilities of patients with heart failure: a systematic literature review. Pharmacoeconomics. 2021;39(2):211–29.
Teerlink JR, Diaz R, Felker GM, et al. Cardiac myosin activation with omecamtiv mecarbil in systolic heart failure. N Engl J Med. 2021;384(2):105–16.
Shah KS, Xu H, Matsouaka RA, et al. Heart failure with preserved, borderline, and reduced ejection fraction: 5-year outcomes. J Am Coll Cardiol. 2017;70(20):2476–86.
Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):e56–528.
Andersson L, Eriksson I, Nordgren L. Living with heart failure without realising: a qualitative patient study. Br J Community Nurs 2012; 17(12): 630, 632-7.
Jones J, McDermott CM, Nowels CT, Matlock DD, Bekelman DB. The experience of fatigue as a distressing symptom of heart failure. Heart Lung. 2012;41(5):484–91.
MacInnes J. An exploration of illness representations and treatment beliefs in heart failure. J Clin Nurs. 2014;23(9–10):1249–56.
Thornhill K, Lyons AC, Nouwen A, Lip GY. Experiences of living with congestive heart failure: a qualitative study. Br J Health Psychol. 2008;13(Pt 1):155–75.
Ryan M, Farrelly M. Living with an unfixable heart: a qualitative study exploring the experience of living with advanced heart failure. Eur J Cardiovasc Nurs. 2009;8(3):223–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Financial support for this study was provided entirely by Amgen Inc. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, and writing and publishing the report.
Author contributions
GLDT planned and originally implemented the model proposal and wrote the paper. BA assisted with the analyses and gave writing support. MU and BS implemented the model in Microsoft Excel and gave writing support. PL, TG and GG gave expert opinion support and writing contributions. All authors participated in the critical review of the manuscript and approved the final version submitted for publication
Conflicts of interest
Björn Stollenwerk is an Amgen employee and Amgen corporate stockholder. Peter Lindgren and Thomas A. Gaziano received Amgen funds and/or honoraria. Gian Luca Di Tanna and Michael Urbich are former Amgen employees. Gian Luca Di Tanna received Amgen honoraria paid to his employer. Gary Globe is a former Amgen employee and remains an Amgen corporate stockholder. Blake Angell is supported by an National Health and Medical Research Council Emerging Leadership Grant (GNT2010055) and declares no other funding or conflicts of interests related to this work.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Code availability
Not applicable.
Availability of data and material
The four models that we have discussed in this manuscript are available at the following Open Science Framework companion repository: https://osf.io/6wx39/ (Di Tanna, G. L. [2022, July 2]; A Proposal of Cost-effectiveness Modeling Approach for Heart Failure Treatment Assessment: Considering the Short- and Long-Term Impact of Hospitalization on Event Rates). These have been developed using the widely available Microsoft Excel suite (Microsoft Corporation, Redmond, WA, USA) but they can be programmed taking advantage of the increasingly available R packages such as heemod, hesim and mstate (The R Foundation for Statistical Computing, Vienna, Austria), among others.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Di Tanna, G.L., Angell, B., Urbich, M. et al. A Proposal of a Cost-Effectiveness Modeling Approach for Heart Failure Treatment Assessment: Considering the Short- and Long-Term Impact of Hospitalization on Event Rates. PharmacoEconomics 40, 1095–1105 (2022). https://doi.org/10.1007/s40273-022-01174-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-022-01174-2