Abstract
Objective
Major depressive disorder (MDD) and chronic non-cancer pain conditions (CNPC) often co-occur and exacerbate one another. Treatment-resistant depression (TRD) in adults with CNPC can amplify the economic burden. This study examined the impact of TRD on direct total and MDD-related healthcare resource utilization (HRU) and costs among commercially insured patients with CNPC and MDD in the US.
Methods
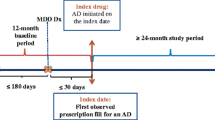
The retrospective longitudinal cohort study employed a claims-based algorithm to identify adults with TRD from a US claims database (January 2007 to June 2017). Costs (2018 US$) and HRU were compared between patients with and without TRD over a 12-month period after TRD/non-TRD index date. Counterfactual recycled predictions from generalized linear models were used to examine associations between TRD and annual HRU and costs. Post-regression linear decomposition identified differences in patient-level factors between TRD and non-TRD groups that contributed to the excess economic burden of TRD.
Results
Of the 21,180 adults with CNPC and MDD, 10.1% were identified as having TRD. TRD patients had significantly higher HRU, translating into higher average total costs (US$21,015TRD vs US$14,712No TRD) and MDD-related costs (US$1201TRD vs US$471No TRD) compared with non-TRD patients (all p < 0.001). Prescription drug costs accounted for 37.6% and inpatient services for 30.7% of the excess total healthcare costs among TRD patients. TRD patients had a significantly higher number of inpatient (incidence rate ratio [IRR] 1.30, 95% CI 1.14–1.47) and emergency room visits (IRR 1.21, 95% CI 1.10–1.34) than non-TRD patients. Overall, 46% of the excess total costs were explained by differences in patient-level characteristics such as polypharmacy, number of CNPC, anxiety, sleep, and substance use disorders between the TRD and non-TRD groups.
Conclusion
TRD poses a substantial direct economic burden for adults with CNPC and MDD. Excess healthcare costs may potentially be reduced by providing timely interventions for several modifiable risk factors.



Similar content being viewed by others

References
Friedrich M. Depression is the leading cause of disability around the world. JAMA. 2017;317(15):1517.
Greenberg PE, Fournier A-A, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76(2):155–62.
Katon WJ. Epidemiology and treatment of depression in patients with chronic medical illness. Dialogues Clin Neurosci. 2011;13(1):7.
Kapfhammer H-P. Somatic symptoms in depression. Dialogues Clin Neurosci. 2006;8(2):227–39.
Lindsay PG, Wyckoff M. The depression-pain syndrome and its response to antidepressants. Psychosomatics. 1981;22(7):571–3.
Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: a literature review. Arch Intern Med. 2003;163(20):2433–45.
Kroenke K, Wu J, Bair MJ, Krebs EE, Damush TM, Tu W. Reciprocal relationship between pain and depression: a 12-month longitudinal analysis in primary care. J Pain. 2011;12(9):964–73.
Welch CA, Czerwinski D, Ghimire B, Bertsimas D. Depression and costs of health care. Psychosomatics. 2009;50(4):392–401. https://doi.org/10.1176/appi.psy.50.4.392.
Rayner L, Hotopf M, Petkova H, Matcham F, Simpson A, McCracken LM. Depression in patients with chronic pain attending a specialised pain treatment centre: prevalence and impact on health care costs. Pain. 2016;157(7):1472.
Bao Y, Sturm R, Croghan TW. A national study of the effect of chronic pain on the use of health care by depressed persons. Psychiatr Serv. 2003;54(5):693–7.
Arnow BA, Hunkeler EM, Blasey CM, Lee J, Constantino MJ, Fireman B, et al. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med. 2006;68(2):262–8.
Bair MJ, Robinson RL, Eckert GJ, Stang PE, Croghan TW, Kroenke K. Impact of pain on depression treatment response in primary care. Psychosom Med. 2004;66(1):17–22.
Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR* D report. Am J Psychiatry. 2006;163(11):1905–17.
Nierenberg AA, DeCecco LM. Definitions of antidepressant treatment response, remission, nonresponse, partial response, and other relevant outcomes: a focus on treatment-resistant depression. J Clin Psychiatry. 2001;62:5–9.
Mrazek DA, Hornberger JC, Altar CA, Degtiar I. A review of the clinical, economic, and societal burden of treatment-resistant depression: 1996–2013. Psychiatr Serv. 2014;65(8):977–87. https://doi.org/10.1176/appi.ps.201300059.
Kubitz N, Mehra M, Potluri RC, Garg N, Cossrow N. Characterization of treatment resistant depression episodes in a cohort of patients from a US commercial claims database. PLoS ONE. 2013;8(10):e76882.
Cepeda MS, Reps J, Ryan P. Finding factors that predict treatment‐resistant depression: results of a cohort study. Depression and anxiety. 2018.
Rizvi SJ, Grima E, Tan M, Rotzinger S, Lin P, McIntyre RS, et al. Treatment-resistant depression in primary care across Canada. Can J Psychiatry Rev Can de Psychiatr. 2014;59(7):349–57.
Johnston KM, Powell LC, Anderson IM, Szabo S, Cline S. The burden of treatment-resistant depression: a systematic review of the economic and quality of life literature. J Affect Disord. 2019;242:195–210.
Kautzky A, Baldinger-Melich P, Kranz GS, Vanicek T, Souery D, Montgomery S, et al. A new prediction model for evaluating treatment-resistant depression. J Clin Psychiatry. 2017;78(2):215–22.
Corey-Lisle PK, Birnbaum HG, Greenberg PE, Marynchenko MB, Claxton AJ. Identification of a claims data" signature" and economic consequences for treatment-resistant depression. J Clin Psychiatry. 2002;63(8):717–26.
Greenberg P, Corey-Lisle PK, Marynchenko M, Claxton A. Economic implications of treatment-resistant depression among employees. Pharmacoeconomics. 2004;22(6):363–73.
Crown WH, Finkelstein S, Berndt ER, Ling D, Poret AW, Rush AJ, et al. The impact of treatment-resistant depression on health care utilization and costs. J Clin Psychiatry. 2002;63(11):963–71.
Amos TB, Tandon N, Lefebvre P, Pilon D, Kamstra RL, Pivneva I et al. Direct and indirect cost burden and change of employment status in treatment-resistant depression: a matched-cohort study using a US Commercial Claims Database. J Clin Psychiatry. 2018;79(2).
Ivanova JI, Birnbaum HG, Kidolezi Y, Subramanian G, Khan SA, Stensland MD. Direct and indirect costs of employees with treatment-resistant and non-treatment-resistant major depressive disorder. Curr Med Res Opin. 2010;26(10):2475–84. https://doi.org/10.1185/03007995.2010.517716.
Rice DP. Cost of illness studies: what is good about them? Inj Prev. 2000;6(3):177–9.
Balestri M, Calati R, Souery D, Kautzky A, Kasper S, Montgomery S, et al. Socio-demographic and clinical predictors of treatment resistant depression: a prospective European multicenter study. J Affect Disord. 2016;189:224–32.
Optum. Optum Clinformatics Data Mart[cited 2018 June 7]. 2018. https://www.optum.com/content/dam/optum/resources/productSheets/Clinformatics_for_Data_Mart.pdf.
Scherrer JF, Svrakic DM, Freedland KE, Chrusciel T, Balasubramanian S, Bucholz KK, et al. Prescription opioid analgesics increase the risk of depression. J Gen Intern Med. 2014;29(3):491–9.
Sullivan MD, Edlund MJ, Fan M-Y, DeVries A, Braden JB, Martin BC. Trends in use of opioids for non-cancer pain conditions 2000–2005 in commercial and Medicaid insurance plans: the TROUP study. Pain. 2008;138(2):440–9.
Shah A, Hayes CJ, Martin BC. Factors influencing long-term opioid use among opioid naive patients: An examination of initial prescription characteristics and pain etiologies. J Pain. 2017;18(11):1374–83.
Schultz J, Joish V. Costs associated with changes in antidepressant treatment in a managed care population with major depressive disorder. Psychiatr Serv. 2009;60(12):1604–11.
Johnson ES, Bartman BA, Briesacher BA, Fleming NS, Gerhard T, Kornegay CJ, et al. The incident user design in comparative effectiveness research. Pharmacoepidemiol Drug Saf. 2013;22(1):1–6.
Gibson TB, Jing Y, Smith CG, Kim E, Bagalman JE, Burton WN, et al. Cost burden of treatment resistance in patients with depression. Am J Manag Care. 2010;16(5):370–7.
Petersen T, Papakostas GI, Posternak MA, Kant A, Guyker WM, Iosifescu DV, et al. Empirical testing of two models for staging antidepressant treatment resistance. J Clin Psychopharmacol. 2005;25(4):336–41.
Marcus RN, McQuade RD, Carson WH, Hennicken D, Fava M, Simon JS, et al. The efficacy and safety of aripiprazole as adjunctive therapy in major depressive disorder: a second multicenter, randomized, double-blind, placebo-controlled study. J Clin Psychopharmacol. 2008;28(2):156–65.
Wong J, Motulsky A, Abrahamowicz M, Eguale T, Buckeridge DL, Tamblyn R. Off-label indications for antidepressants in primary care: descriptive study of prescriptions from an indication based electronic prescribing system. BMJ. 2017;356:j603. https://doi.org/10.1136/bmj.j603.
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995:1–10.
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230.
Deb P, Norton EC. Modeling health care expenditures and use. Annu Rev Public Health. 2018;39:489–505. https://doi.org/10.1146/annurev-publhealth-040617-013517.
Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic evaluation in clinical trials. Oxford: OUP Oxford; 2014.
Basu A, Rathouz PJ. Estimating marginal and incremental effects on health outcomes using flexible link and variance function models. Biostatistics. 2005;6(1):93–109. https://doi.org/10.1093/biostatistics/kxh020.
Oaxaca R. Male-female wage differentials in urban labor markets. Int Econ Rev. 1973:693–709.
Blinder AS. Wage discrimination: reduced form and structural estimates. J Human Resour. 1973:436–55.
Mitra S, Findley PA, Sambamoorthi U. Health care expenditures of living with a disability: total expenditures, out-of-pocket expenses, and Burden, 1996 to 2004. Arch Phys Med Rehabil. 2009;90(9):1532–40. https://doi.org/10.1016/j.apmr.2009.02.020.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424. https://doi.org/10.1080/00273171.2011.568786.
Vergunst FK, Fekadu A, Wooderson SC, Tunnard CS, Rane LJ, Markopoulou K, et al. Longitudinal course of symptom severity and fluctuation in patients with treatment-resistant unipolar and bipolar depression. Psychiatry Res. 2013;207(3):143–9.
Johansson T, Abuzahra ME, Keller S, Mann E, Faller B, Sommerauer C, et al. Impact of strategies to reduce polypharmacy on clinically relevant endpoints: a systematic review and meta-analysis. Br J Clin Pharmacol. 2016;82(2):532–48.
Kojima G, Bell C, Tamura B, Inaba M, Lubimir K, Blanchette PL et al. Reducing cost by reducing polypharmacy: the polypharmacy outcomes project. J Am Med Dir Assoc. 2012;13(9):818.e11–e8.18E15. https://doi.org/10.1016/j.jamda.2012.07.019.
Bergfeld IO, Mantione M, Figee M, Schuurman PR, Lok A, Denys D. Treatment-resistant depression and suicidality. J Affect Disord. 2018;235:362–7. https://doi.org/10.1016/j.jad.2018.04.016.
Pfeiffer PN, Kim HM, Ganoczy D, Zivin K, Valenstein M. Treatment-resistant depression and risk of suicide. Suicide Life Threat Behav. 2013;43(4):356–65. https://doi.org/10.1111/sltb.12022.
Davydow DS, Fenger-Grøn M, Ribe AR, Pedersen HS, Prior A, Vedsted P, et al. Depression and risk of hospitalisations and rehospitalisations for ambulatory care-sensitive conditions in Denmark: a population-based cohort study. BMJ Open. 2015;5(12):e009878.
Citrome L, Jain R, Tung A, Landsman-Blumberg PB, Kramer K, Ali S. Prevalence, treatment patterns, and stay characteristics associated with hospitalizations for major depressive disorder. J Affect Disord. 2019;249:378–84. https://doi.org/10.1016/j.jad.2019.01.044.
Sambamoorthi U, Tan X, Deb A. Multiple chronic conditions and healthcare costs among adults. Expert Rev Pharmacoecon Outcomes Res. 2015;15(5):823–32.
Arnow BA, Blasey CM, Lee J, Fireman B, Hunkeler EM, Dea R, et al. Relationships among depression, chronic pain, chronic disabling pain, and medical costs. Psychiatr Serv. 2009;60(3):344–50. https://doi.org/10.1176/appi.ps.60.3.34410.1176/ps.2009.60.3.344.
Lin EH, Katon W, Von Korff M, Tang L, Williams JW Jr, Kroenke K, et al. Effect of improving depression care on pain and functional outcomes among older adults with arthritis: a randomized controlled trial. JAMA. 2003;290(18):2428–9.
Pietruszewski P. A new direction in depression treatment in Minnesota: DIAMOND program. Inst Clin Syst Improv Bloomington Minnesota Psychiatr Serv. 2010;61(10):1042–4.
Katon WJ, Lin EH, Von Korff M, Ciechanowski P, Ludman EJ, Young B, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363(27):2611–20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the study. The authors have disclosed that they have no significant relationships with or financial interests in any commercial companies related to this study or article.
Conflict of Interest
Drishti Shah and Suresh Madhavan were employees at West Virginia University at the time of the study. Wenhui Wei is an employee at Regeneron Pharmaceuticals. The authors report no conflict of interest.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Availability of Data and Material
This retrospective database study used commercial claims data from the Optum Clinformatics® Data Mart (Eden Prairie, MN, USA). The claims data that support the findings of this study are from a proprietary administrative claims database and are not publicly available. However, summary data tables are available from the authors upon reasonable request.
Code Availability
Not applicable.
Author Contributions
DS was responsible for developing the initial concept and study design. All authors contributed to the subsequent conception, and design of the final study. WZ provided clinical insights, reviewed and approved the clinical algorithms and diagnosis codes used in the current study. DS and US conducted the statistical analyses. The first draft of the manuscript was written by DS. All authors worked on successive iterations, read and approved the final manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Shah, D., Allen, L., Zheng, W. et al. Economic Burden of Treatment-Resistant Depression among Adults with Chronic Non-Cancer Pain Conditions and Major Depressive Disorder in the US. PharmacoEconomics 39, 639–651 (2021). https://doi.org/10.1007/s40273-021-01029-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-021-01029-2