Abstract
Introduction
Medication non-adherence is a serious barrier to treatment of schizophrenia. Understanding the impact of non-adherence on costs is essential to the assessment of the cost effectiveness of interventions in which adherence to treatment is a concern.
Objectives
We undertook a comprehensive review of the available literature on the impact on costs of non-adherence to antipsychotics in the treatment of schizophrenia.
Methods
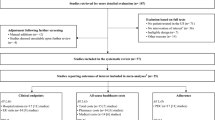
We performed a search on multiple databases (MEDLINE, Embase, PsycINFO and Health Management Information Consortium) for any study reporting the impact of adherence to antipsychotics on costs in patients with schizophrenia up to February 2018. We included trials of behavioural interventions but excluded comparisons of different pharmacological therapies. Studies were included if at least one-third of the study population had schizophrenia and costs were reported.
Results
Thirty-four publications on 28 studies met the inclusion criteria. Twenty studies reported analyses of administrative databases, primarily Medicaid. Findings on healthcare costs were mixed but suggested that lower pharmacy costs in non-adherent patients may outweigh increased hospitalisation costs where drug costs are relatively high. A few studies published analysis of prospective cohort data, or trials of behavioural interventions intended to influence adherence, mainly in a European setting. Findings were again mixed but indicate that increasing adherence does not reduce overall costs.
Conclusions
Inference from analysis of administrative data is limited by the risk of selection bias. Inference from trials is limited by small sample sizes. The literature does not consistently support an assumption that non-adherence increases healthcare costs.


Similar content being viewed by others
References
Jablensky A, Sartorius N, Ernberg G, Anker M, Korten A, Cooper JE, Day R, Bertelsen A. Schizophrenia: manifestations, incidence and course in different cultures. A World Health Organization Ten-Country Study. Psychol Med Monogr Suppl. 1992;20:1–97.
Hasan A, Falkai P, Wobrock T, Lieberman J, Glenthoj B, Gattaz WF, Thibaut F, Möller HJ. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, part 1: update 2012 on the acute treatment of schizophrenia and the management of treatment resistance. World J Biol Psychiatry. 2012;13(5):318–78.
Altar CA, Martin AR, Thurkauf A. Antipsychotic agents. Burger’s Medicinal Chemistry and Drug Discovery. Wiley; 2003. http://onlinelibrary.wiley.com/doi/book/10.1002/0471266949.
Svestka J, Bitter I. Nonadherence to antipsychotic treatment in patients with schizophrenic disorders. Neuro Endocrinol Lett. 2007;28:95–116.
Julius RJ, Novitsky MA Jr, Dubin WR. Medication adherence: a review of the literature and implications for clinical practice. J Psychiatr Prac. 2009;15(1):34–44.
Byerly MJ, Ann Thompson MB, Carmody T, Bugno R, Erwin T, Michael Kashner JD, John Rush A. Validity of electronically monitored medication adherence and conventional adherence measures in schizophrenia. Psychiat Serv. 2007;58:844–7.
Velligan DI, Wang M, Diamond P, Glahn DC, Castillo D, Scott Bendle M, Lam YF, Ereshefsky L, Miller AL. Relationships among subjective and objective measures of adherence to oral antipsychotic medications. Psychiatr Serv. 2007;58:1187–92.
Roberts DL, Velligan DI. Medication adherence in schizophrenia. Drug Discov Today Ther Strateg. 2011;8(1):11–5.
Andrade SE, Kahler KH, Frech F, Chan KA. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf. 2006;15(8):565–74.
Karve S, Cleves MA, Helm M, Hudson TJ, West DS, Martin BC. Prospective validation of eight different adherence measures for use with administrative claims data among patients with schizophrenia. Value Health. 2009;12(6):989–95.
Barkhof E, Meijer CJ, de Sonneville LM, Linszen DH, Haan L. Interventions to improve adherence to antipsychotic medication in patients with schizophrenia—a review of the past decade. Eur Psychiatr. 2012;27(1):9–18.
Dilla T, Álvarez M. Systematic review of the economic aspects of nonadherence to antipsychotic medication in patients with schizophrenia. Patient Prefer Adher. 2013;7:275–84.
Higashi K, Medic G, Littlewood KJ, Diez T, Granström O, De Hert M. Medication adherence in schizophrenia: factors influencing adherence and consequences of nonadherence, a systematic literature review. Ther Adv Psychopharmacol. 2013;3(4):200–18.
Kane JM. Review of treatments that can ameliorate nonadherence in patients with schizophrenia. J Clin Psychiatry. 2006;67(suppl 5):1–478.
Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. J Clin Psychiatry. 2002;63(10):892–909.
Shuler KM. Approaches to improve adherence to pharmacotherapy in patients with schizophrenia. Patient Pref Adher. 2013;8:701–14.
Sun SX, Liu GG, Christensen DB, Fu AZ. Review and analysis of hospitalization costs associated with antipsychotic nonadherence in the treatment of schizophrenia in the United States. Curr Med Res Opin. 2007;23(10):2305–12.
Sendt KV, Tracy DK, Bhattacharyya S. A systematic review of factors influencing adherence to antipsychotic medication in schizophrenia-spectrum disorders. Psychiatry Res. 2015;225(1):14–30.
Thieda P, Beard S, Richter A, Kane J. An economic review of compliance with medication therapy in the treatment of schizophrenia. Psychiatr Serv. 2003;54(4):508–16.
Ascher-Svanum H, Nyhuis AW, Faries DE, Ball DE, Kinon BJ. Involvement in the US criminal justice system and cost implications for persons treated for schizophrenia. BMC Psychiatry. 2010;10(1):11.
Swartz MS, Swanson JW, Hiday VA, Borum R, Wagner HR, Burns BJ. Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. Am J Psychiatry. 1998;155:226–31.
Miller BJ, Bodenheimer C, Crittenden K. Second-generation antipsychotic discontinuation in first episode psychosis: an updated review. Clin Psychopharmacol Neurosci. 2011;9(2):45.
Gaebel W, Jänner M, Frommann N, Pietzcker A, Köpcke W, Linden M, Müller P, Müller-Spahn F, Tegeler J. First vs multiple episode schizophrenia: two-year outcome of intermittent and maintenance medication strategies. Schizophr Res. 2002;53(1):145–59.
Svarstad BL, Shireman TI, Sweeney JK. Using drug claims data to assess the relationship of medication adherence with hospitalization and costs. Psychiatr Serv. 2001;52(6):805–11.
Becker MA, Young MS, Ochshorn E, Diamond RJ. The relationship of antipsychotic medication class and adherence with treatment outcomes and costs for Florida Medicaid beneficiaries with schizophrenia. Adm Policy Ment Health Ment Health Serv Res. 2007;34(3):307–14.
Hansen RA, Maciejewski M, Yu-Isenberg K, Farley JF. Adherence to antipsychotics and cardiometabolic medication: association with health care utilization and costs. Psychiatr Serv. 2012;63(9):920–8.
Robertson AG, Swanson JW, Van Dorn RA, Swartz MS. Economic Grand Rounds: treatment participation and medication adherence: effects on criminal justice costs of persons with mental illness. Psychiatr Serv. 2014;65(10):1189–91.
McCombs JS, Luo M, Johnstone BM, Shi L. The use of conventional antipsychotic medications for patients with schizophrenia in a medicaid population: therapeutic and cost outcomes over 2 years. Value Health. 2000;3(3):222–31.
Pai J, McCombs J. PMH44 Impact of alternative definitions of medication compliance on first year treatment cost for Medi-Cal patients with schizophrenia. Value Health. 2010;13(3):A112.
Ahn J, McCombs JS, Jung C, Croudace TJ, McDonnell D, Ascher-Svanum H, Edgell ET, Shi L. Classifying patients by antipsychotic adherence patterns using latent class analysis: characteristics of nonadherent groups in the California Medicaid (Medi-Cal) program. Value Health. 2008;11(1):48–56.
Gilmer TP, Dolder CR, Lacro JP, Folsom DP, Lindamer L, Garcia P, Jeste DV. Adherence to treatment with antipsychotic medication and health care costs among Medicaid beneficiaries with schizophrenia. Am J Psychiatry. 2004;161(4):692–9.
Eaddy M, Grogg A, Locklear J. Assessment of compliance with antipsychotic treatmentand resource utilization in a medicaid population. Clin Ther. 2005;27(2):263–72.
Farley JF. Medicaid prescription cost containment and schizophrenia: a retrospective examination. Med Care. 2010;48(5):440–7.
Jiang Y, Ni W. Estimating the impact of adherence to and persistence with atypical antipsychotic therapy on health care costs and risk of hospitalization. Pharmacotherapy. 2015;35(9):813–22.
Marcus SC, Olfson M. Outpatient antipsychotic treatment and inpatient costs of schizophrenia. Schizophr Bull. 2008;34(1):173–80.
Markowitz M, Karve S, Panish J, Candrilli SD, Alphs L. Antipsychotic adherence patterns and health care utilization and costs among patients discharged after a schizophrenia-related hospitalization. BMC Psychiatry. 2013;13(1):1.
Offord S, Lin J, Wong B, Mirski D, Baker RA. Impact of oral antipsychotic medication adherence on healthcare resource utilization among schizophrenia patients with medicare coverage. Commun Ment Health J. 2013;49(6):625–9.
Offord S, Lin J, Mirski D, Wong B. Impact of early nonadherence to oral antipsychotics on clinical and economic outcomes among patients with schizophrenia. Adv Ther. 2013;30(3):286–97.
Zeber JE, Grazier KL, Valenstein M, Blow FC, Lantz PM. Effect of a medication copayment increase in veterans with schizophrenia. Am J Managed Care. 2007;13(6):335–47.
Roberto P, Brandt N, Onukwugha E, Perfetto E, Powers C, Stuart B. Adherence to antipsychotic therapy: association with hospitalization and Medicare spending among Part D enrollees with schizophrenia. Psychiatr Serv. 2017;68(11):1185–8.
Joe S, Lee JS. Association between non-compliance with psychiatric treatment and non-psychiatric service utilization and costs in patients with schizophrenia and related disorders. BMC Psychiatry. 2016;16(1):444.
van der Lee A, de Haan L, Beekman A. Schizophrenia in the Netherlands: continuity of care with better quality of care for less medical costs. PLoS ONE. 2016;11(6):e0157150.
Dilokthornsakul P, Thoopputra T, Patanaprateep O, Kongsakon R, Chaiyakunapruk N. Effects of medication adherence on hospitalizations and healthcare costs in patients with schizophrenia in Thailand. SAGE Open Med. 2016;4:2050312116637026.
Zeber JE, Copeland LA, Miller AL, Valenstein M, Luci L. A cost-benefit analysis of higher medication copayments in veterans with schizophrenia. Schizophr Bull. 2009;35:130.
Knapp M, King D, Pugner K, Lapuerta P. Non-adherence to antipsychotic medication regimens: associations with resource use and costs. Br J Psychiatry. 2004;184(6):509–16.
Salize HJ, McCabe R, Bullenkamp J, Hansson L, Lauber C, Martinez-Leal R, Reinhard I, Rössler W, Svensson B, Torres-Gonzalez F, van den Brink R. Cost of treatment of schizophrenia in six European countries. Schizophr Res. 2009;111(1):70–7.
Hong J, Novick D, Haro JM, Knapp M. PW01-181-Economic consequences of medication nonadherence in the treatment of schizophrenia: 36-month results from the SOHO (schizophrenia outpatient health outcomes) study. Eur Psychiatry. 2010;25:1609.
King D, Knapp M, Patel A, Amaddeo F, Tansella M, Schene A, Koeter M, Angermeyer M, Becker T. The impact of non-adherence to medication in patients with schizophrenia on health, social care and societal costs Analysis of the QUATRO study. Epidemiol Psychiatr Sci. 2014;23(01):61–70.
Novick D, Haro JM, Suarez D, Perez V, Dittmann RW, Haddad PM. Predictors and clinical consequences of non-adherence with antipsychotic medication in the outpatient treatment of schizophrenia. Psychiatry Res. 2010;176(2):109–13.
King, D. (2010). Non-adherence to medication in schizophrenia: The impact on service use and costs. Thesis submitted to London School of Economics and Political Science for the degree of Doctor of Philosophy, London. http://etheses.lse.ac.uk/295/1/King_Non-adherence%20to%20medication%20in%20schizophrenia.pdf. Accessed 16 Apr 2018.
Healey A, Knapp M, Astin J, Beecham J, Kemp R, Kirov G, David A. Cost-effectiveness evaluation of compliance therapy for people with psychosis. Br J Psychiatry. 1998;172(5):420–4.
Kemp R, Kirov G, Everitt B, Hayward P, David A. Randomised controlled trial of compliance therapy. 18-month follow-up. Br J Psychiatry. 1998;172(5):413–9.
Stant AD, TenVergert EM, Wunderink L, Nienhuis FJ, Wiersma D. Economic consequences of alternative medication strategies in first episode non-affective psychosis. Eur Psychiatry. 2007;22(6):347–53.
Wunderink L, Nienhuis FJ, Sytema S, Slooff CJ, Knegtering R, Wiersma D. Guided discontinuation versus maintenance treatment in remitted first-episode psychosis: relapse rates and functional outcome. J Clin Psychiatry. 2007;68(5):654–61.
Gilden J, Staring AB, Van der Gaag M, Mulder CL. Does treatment adherence therapy reduce expense of healthcare use in patients with psychotic disorders? Cost-minimization analysis in a randomized controlled trial. Schizophr Res. 2011;133(1):47–53.
Staring AB, Van der Gaag M, Koopmans GT, Selten JP, Van Beveren JM, Hengeveld MW, Loonen AJ, Mulder CL. Treatment adherence therapy in people with psychotic disorders: randomised controlled trial. Br J Psychiatry. 2010;197(6):448–55.
Henderson C, Knapp M, Yeeles K, Bremner S, Eldridge S, David AS, O’Connell N, Burns T, Priebe S. Cost-effectiveness of financial incentives to promote adherence to depot antipsychotic medication: economic evaluation of a cluster-randomised controlled trial. PLoS ONE. 2015;10(10):e0138816.
Priebe S, Bremner SA, Lauber C, Henderson C, Burns T. Financial incentives to improve adherence to antipsychotic maintenance medication in non-adherent patients: a cluster randomised controlled trial. Health Technol Assess. 2016;20(70):1–22.
O’Malley AJ, Frank RG, Normand SL. Estimating cost-offsets of new medications: use of new antipsychotics and mental health costs for schizophrenia. Stat Med. 2011;30(16):1971–88.
Funding
This study was funded by Janssen-Cilag Ltd. It was not part of a specific programme. Representatives from Janssen have commented on a draft but the authors retained sole control over the design, implementation and reporting of the results.
Author information
Authors and Affiliations
Contributions
PM is responsible for the conception of the project and editing of the manuscript. MP undertook the literature searching, extraction of data and drafting of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
MP reports no conflicts of interest. PM reports no conflicts of interest.
Data availability
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Rights and permissions
About this article
Cite this article
Pennington, M., McCrone, P. Does Non-Adherence Increase Treatment Costs in Schizophrenia?. PharmacoEconomics 36, 941–955 (2018). https://doi.org/10.1007/s40273-018-0652-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-018-0652-3