Abstract
Background
Inaccurate estimates of diabetes-related healthcare costs can undermine the efficiency of resource allocation for diabetes care. The quantification of these costs using claims data may be affected by the method for defining diagnoses.
Objectives
The aims were to use panel data analysis to estimate diabetes-related healthcare costs and to comparatively evaluate the effects of diagnostic definitions on cost estimates.
Research design
Monthly panel data analysis of Japanese claims data.
Subjects
The study included a maximum of 141,673 patients with type 2 diabetes who received treatment between 2005 and 2013.
Measures
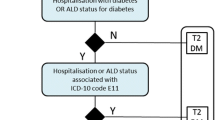
Additional healthcare costs associated with diabetes and diabetes-related complications were estimated for various diagnostic definition methods using fixed-effects panel data regression models.
Results
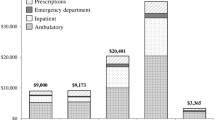
The average follow-up period per patient ranged from 49.4 to 52.3 months. The number of patients identified as having type 2 diabetes varied widely among the diagnostic definition methods, ranging from 14,743 patients to 141,673 patients. The fixed-effects models showed that the additional costs per patient per month associated with diabetes ranged from US$180 [95 % confidence interval (CI) 178–181] to US$223 (95 % CI 221–224). When the diagnostic definition excluded rule-out diagnoses, the diabetes-related complications associated with higher additional healthcare costs were ischemic heart disease with surgery (US$13,595; 95 % CI 13,568–13,622), neuropathy/extremity disease with surgery (US$4594; 95 % CI 3979–5208), and diabetic nephropathy with dialysis (US$3689; 95 % CI 3667–3711).
Conclusions
Diabetes-related healthcare costs are sensitive to diagnostic definition methods. Determining appropriate diagnostic definitions can further advance healthcare cost research for diabetes and its applications in healthcare policies.
Similar content being viewed by others
References
American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36:1033–46.
American Diabetes Association. Economic costs of diabetes in the U.S. In 2007. Diabetes Care. 2008;31:596–615.
Rice DP. Cost-of-illness studies: fact or fiction? Lancet. 1994;344:1519–20.
Ettaro L, Songer TJ, Zhang P, Engelgau MM. Cost-of-illness studies in diabetes mellitus. Pharmacoeconomics. 2004;22:149–64.
Seuring T, Archangelidi O, Suhrcke M. The economic costs of type 2 diabetes: a global systematic review. Pharmacoeconomics. 2015;33:811–31.
Ng CS, Lee JY, Toh MP, Ko Y. Cost-of-illness studies of diabetes mellitus: a systematic review. Diabetes Res Clin Pract. 2014;105:151–63.
Ringborg A, Yin DD, Martinell M, Stålhammar J, Lindgren P. The impact of acute myocardial infarction and stroke on health care costs in patients with type 2 diabetes in Sweden. Eur J Cardiovasc Prev Rehabil. 2009;16:576–82.
Clarke P, Leal J, Kelman C, Smith M, Colagiuri S. Estimating the cost of complications of diabetes in Australia using administrative health-care data. Value Health. 2008;11:199–206.
Oglesby AK, Secnik K, Barron J, Al-Zakwani I, Lage MJ. The association between diabetes related medical costs and glycemic control: a retrospective analysis. Cost Eff Resour Alloc. 2006;4:1.
Okamoto E. Declining accuracy in disease classification on health insurance claims: should we reconsider classification by principal diagnosis? J Epidemiol. 2010;20:166–75.
Tanihara S, Okamoto E, Une H. A statistical analysis of ‘rule-out’ diagnoses in outpatient health insurance claims in Japan. J Eval Clin Pract. 2011;17:1070–4.
American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care. 2013;36:S11–66.
Kitazato H, Ikeda S, Izumi K, et al. A method to investigate medical expenditure in Japan in relationship of stage progression of type 2 diabetes mellitus complications and macroangiopathy. Obesity Diabetes. 2010;9:S48–64 [in Japanese].
Honeycutt AA, Segel JE, Hoerger TJ, et al. Comparing cost-of-illness estimates from alternative approaches: an application to diabetes. Health Serv Res. 2009;44:303–20.
Shrestha SS, Zhang P, Albright A, Finkelstein EA. Medical expenditures associated with diabetes among privately insured U.S. youth in 2007. Diabetes Care. 2011;34:1097–101.
Trogdon JG, Hylands T. Nationally representative medical costs of diabetes by time since diagnosis. Diabetes Care. 2008;31:2307–11.
Tunceli O, Wade R, Gu T, Bouchard JR, Aagren M, Luo W. Cost of diabetes: comparison of disease-attributable and matched cohort cost estimation methods. Curr Med Res Opin. 2010;26:1827–34.
Pagano E, Bo S, Petrinco M, Rosato R, Merletti F, Gregori D. Factors affecting hospitalization costs in type 2 diabetic patients. J Diabetes Complicat. 2009;23:1–6.
Lee LJ, Yu AP, Cahill KE, et al. Direct and indirect costs among employees with diabetic retinopathy in the United States. Curr Med Res Opin. 2008;24:1549–59.
Fu AZ, Qiu Y, Radican L, Wells BJ. Health care and productivity costs associated with diabetic patients with macrovascular comorbid conditions. Diabetes Care. 2009;32:2187–92.
Durden ED, Alemayehu B, Bouchard JR, Chu BC, Aagren M. Direct health care costs of patients with type 2 diabetes within a privately insured employed population, 2000 and 2005. J Occup Environ Med. 2009;51:1460–5.
Currie CJ, Poole CD, Woehl A, et al. The financial costs of healthcare treatment for people with type 1 or type 2 diabetes in the UK with particular reference to differing severity of peripheral neuropathy. Diabet Med. 2007;24:187–94.
Alva ML, Gray A, Mihaylova B, Leal J, Holman RR. The impact of diabetes-related complications on healthcare costs: new results from the UKPDS (UKPDS 84). Diabet Med. 2015;32:459–66.
Clarke PM, Glasziou P, Patel A, et al. Event rates, hospital utilization, and costs associated with major complications of diabetes: a multicountry comparative analysis. PLoS Med. 2010;7:e1000236.
Gerdtham UG, Clarke P, Hayes A, Gudbjornsdottir S. Estimating the cost of diabetes mellitus-related events from inpatient admissions in Sweden using administrative hospitalization data. Pharmacoeconomics. 2009;27:81–90.
Japan’s Health Service Bureau. National Health and Nutrition Survey 2007. http://www.mhlw.go.jp/bunya/kenkou/eiyou09/dl/01-kekka.pdf. Accessed 25 Jan 2016.
Author contributions
HF contributed to the study concept, design, data analysis and interpretation, and drafting of the manuscript. SI, TS, and TF contributed to the study concept and data interpretation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This research was supported in part by a Grant-in-Aid for Young Scientists (A) by the Japan Society for the Promotion of Science (JSPS) KAKENHI (Grant Number 25713029) and a Grant-in-Aid for Health Sciences Research by the Ministry of Health, Labour and Welfare of Japan (Grant Number H25-Seisaku-Shitei-011).
Conflict of interest
No conflicts of interest exist for Haruhisa Fukuda, Shunya Ikeda, Takeru Shiroiwa and Takashi Fukuda.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fukuda, H., Ikeda, S., Shiroiwa, T. et al. The Effects of Diagnostic Definitions in Claims Data on Healthcare Cost Estimates: Evidence from a Large-Scale Panel Data Analysis of Diabetes Care in Japan. PharmacoEconomics 34, 1005–1014 (2016). https://doi.org/10.1007/s40273-016-0402-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-016-0402-3