Abstract
Background
Scale heterogeneity, or differences in the error variance of choices, may account for a significant amount of the observed variation in the results of discrete choice experiments (DCEs) when comparing preferences between different groups of respondents.
Objective
The aim of this study was to identify if, and how, scale heterogeneity has been addressed in healthcare DCEs that compare the preferences of different groups.
Methods
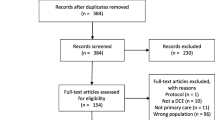
A systematic review identified all healthcare DCEs published between 1990 and February 2016. The full-text of each DCE was then screened to identify studies that compared preferences using data generated from multiple groups. Data were extracted and tabulated on year of publication, samples compared, tests for scale heterogeneity, and analytical methods to account for scale heterogeneity. Narrative analysis was used to describe if, and how, scale heterogeneity was accounted for when preferences were compared.
Results
A total of 626 healthcare DCEs were identified. Of these 199 (32%) aimed to compare the preferences of different groups specified at the design stage, while 79 (13%) compared the preferences of groups identified at the analysis stage. Of the 278 included papers, 49 (18%) discussed potential scale issues, 18 (7%) used a formal method of analysis to account for scale between groups, and 2 (1%) accounted for scale differences between preference groups at the analysis stage. Scale heterogeneity was present in 65% (n = 13) of studies that tested for it. Analytical methods to test for scale heterogeneity included coefficient plots (n = 5, 2%), heteroscedastic conditional logit models (n = 6, 2%), Swait and Louviere tests (n = 4, 1%), generalised multinomial logit models (n = 5, 2%), and scale-adjusted latent class analysis (n = 2, 1%).
Conclusions
Scale heterogeneity is a prevalent issue in healthcare DCEs. Despite this, few published DCEs have discussed such issues, and fewer still have used formal methods to identify and account for the impact of scale heterogeneity. The use of formal methods to test for scale heterogeneity should be used, otherwise the results of DCEs potentially risk producing biased and potentially misleading conclusions regarding preferences for aspects of healthcare.



Similar content being viewed by others
References
McFadden D. The choice theory approach to market research. Mark Sci. 1986;5:275–97.
Wright SJ, Ulph F, Dharni N, Payne K. Eliciting preferences for information provision in newborn bloodspot screening programs. Value Health. 2017;20:651–61.
Mirelman A, Mentzakis E, Kinter E, Paolucci F, Fordham R, Ozawa S, et al. Decision-making criteria among national policymakers in five countries: a discrete choice experiment eliciting relative preferences for equity and efficiency. Value Health. 2012;15:534–9.
Bansback N, Hole AR, Mulhern B, Tsuchiya A. Testing a discrete choice experiment including duration to value health states for large descriptive systems: addressing design and sampling issues. Soc Sci Med. 2014;114:38–48.
de Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ. 2012;21:145–72.
Clark M, Determann D, Petrou S, Moro D, de Bekker-Grob EW. Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics. 2014;32:883–902.
StataCorp. Stata Statistical Software: Release 12. College Station, TX: StataCorp LP; 2011.
Sawtooth. Sawtooth Software SSI Web 8.3.8. 2012.
Econometric Software Inc. NLOGIT. 2015. Available from: http://www.limdep.com/. Accessed 26 Feb 2018.
Hole AR. Modelling heterogeneity in patients’ preferences for the attributes of a general practitioner appointment. J Health Econ. 2008;27:1078–94.
Hensher D, Greene W. The mixed logit model: the state of practice. Transport. 2003;30:133–76.
Greene WH, Hensher D. A latent class model for discrete choice analysis: contrasts with mixed logit. Transp Res Part B Methodol. 2003;37:681–98.
Huber J, Train K. On the similarity of classical and bayesian estimates of individual mean partworths. Mark. Lett. 2001;123:259–69.
Vass CM, Wright S, Burton M, Payne K. Scale heterogeneity in healthcare discrete choice experiments: a primer. Patient. 2017. https://doi.org/10.1007/s40271-017-0282-4 (Epub 14 Oct 2017).
Innovations Statistical. Latent gold. Belmont: Statistical Innovations; 2013.
Hess S, Train K. Correlation and scale in mixed logit models. J Choice Model. 2017;23:1–8.
Hensher D, Louviere J, Swait J. Combining sources of preference data. J Econ. 1998;89:197–221.
Swait J, Louviere J. The role of the scale parameter in the estimation and comparison of multinomial logit models. J Mark Res. 1993;30:305–14.
Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Vass C, Gray E, Payne K. Discrete choice experiments of pharmacy services: a systematic review. Int J Clin Pharm. 2016;38(3):620–30.
Vass C, Rigby D, Payne K. The role of qualitative research methods in discrete choice experiments. Med Decis Mak. 2017;37:298–313.
Ryan M, Gerard K. Using discrete choice experiments to value health care programmes: current practice and future research reflections. Appl Health Econ Health Policy. 2003;2:55–64.
Barnes AJ, Hanoch Y, Rice T. Determinants of coverage decisions in health insurance marketplaces: consumers’ decision-making abilities and the amount of information in their choice environment. Health Serv Res. 2015;50:58–80.
Koopmanschap MA, Stolk EA, Koolman XHE. Dear policy maker: have you made up your mind? A discrete choice experiment among policy makers and other health professionals. Int J Technol Assess Health Care. 2010;26:198–204.
Ostermann J, Njau B, Mtuy T, Brown DS, Muhlbacher A, Thielman N. One size does not fit all: HIV testing preferences differ among high-risk groups in Northern Tanzania. AIDS Care. 2015;27:595–603.
Araña JE, León CJ, Quevedo JL. The effect of medical experience on the economic evaluation of health policies. A discrete choice experiment. Soc Sci Med. 2006;63:512–24.
Bech M, Kjaer T, Lauridsen J. Does the number of choice sets matter? Results from a web survey applying a discrete choice experiment. Health Econ. 2011;20:273–86.
Hall J, Fiebig DG, King MT, Hossain I, Louviere JJ. What influences participation in genetic carrier testing? Results from a discrete choice experiment. J Health Econ. 2006;25:520–37.
Van Helvoort-Postulart D, Dellaert BGC, Van Der Weijden T, Von Meyenfeldt MF, Dirksen CD. Discrete choice experiments for complex health-care decisions: does hierarchical information integration offer a solution ? Health Econ. 2009;920:903–20.
Holte JH, Kjaer T, Abelsen B, Olsen JA. The impact of pecuniary and non-pecuniary incentives for attracting young doctors to rural general practice. Soc Sci Med. 2015;128:1–9.
Kinter ET, Prior TJ, Carswell CI, Bridges JFP. A comparison of two experimental design approaches in applying conjoint analysis in patient-centered outcomes research: a randomized trial. Patient. 2012;5:279–94.
Knox SA, Viney RC, Gu Y, Hole AR, Fiebig DG, Street DJ, et al. The effect of adverse information and positive promotion on women’s preferences for prescribed contraceptive products. Soc Sci Med. 2013;83:70–80.
Meghani SH, Chittams J, Hanlon AL, Curry J. Measuring preferences for analgesic treatment for cancer pain: how do African-Americans and Whites perform on choice-based conjoint (CBC) analysis experiments? BMC Med Inform Decis Mak. 2013;13:118.
Milte R, Ratcliffe J, Chen G, Lancsar E, Miller M, Crotty M. Cognitive overload? An exploration of the potential impact of cognitive functioning in discrete choice experiments with older people in health care. Value Health. 2014;17:655–9.
Owen K, Pettman T, Haas M, Viney R, Misan G. Individual preferences for diet and exercise programmes: changes over a lifestyle intervention and their link with outcomes. Public Health Nutr. 2010;13:245–52.
Payne K, Fargher EA, Roberts SA, Tricker K, Elliott RA, Ratcliffe J, et al. Valuing pharmacogenetic testing services: a comparison of patients’ and health care professionals’ preferences. Value Health. 2011;14:121–34.
Pedersen LB, Kjær T, Kragstrup J, Gyrd-Hansen D. Do general practitioners know patients’ preferences? an empirical study on the agency relationship at an aggregate level using a discrete choice experiment. Value Health. 2012;15:514–23.
Salampessy BH, Veldwijk J, Jantine Schuit A, van den Brekel-Dijkstra K, Neslo REJ, Ardine de Wit G, et al. The predictive value of discrete choice experiments in public health: an exploratory application. Patient. 2015;8:521–9.
Veldwijk J, Lambooij MS, van Til JA, Groothuis-Oudshoorn CGM, Smit HA, de Wit GA. Words or graphics to present a discrete choice experiment: does it matter? Patient Educ Couns. 2015;98:1376–84.
Finkelstein EA, Bilger M, Flynn TN, Malhotra C. Preferences for end-of-life care among community-dwelling older adults and patients with advanced cancer: a discrete choice experiment. Health Policy. 2015;119:1482–9.
Miller F, Hayeems RZ, Bombard Y, Cressman C, Barg CJ, Carroll JC, et al. Public perceptions of the benefits and risks of newborn screening. Pediatrics. 2015;136:e413–23.
Carroll FE, Al-Janabi H, Flynn T, Montgomery AA. Women and their partners’ preferences for Down’s syndrome screening tests: a discrete choice experiment. Prenat Diagn. 2013;33:449–56.
Erdem S, Thompson C. Prioritising health service innovation investments using public preferences: a discrete choice experiment. BMC Health Serv Res. 2014;14:360.
Fiebig DG, Haas M, Hossain I, Street DJ, Viney R. Decisions about pap tests: what influences women and providers? Soc Sci Med. 2009;68:1766–74.
Arbiol J, Yabe M, Nomura H, Borja M, Gloriani N, Yoshida SI. Using discrete choice modeling to evaluate the preferences and willingness to pay for leptospirosis vaccine. Hum Vaccines Immunother. 2015;11:1046–56.
de Bekker-Grob EW, Bliemer MCJ, Donkers B, Essink-Bot M-L, Korfage IJ, Roobol MJ, et al. Patients’ and urologists’ preferences for prostate cancer treatment: a discrete choice experiment. Br J Cancer. 2013;109:633–40.
Essers BAB, Van Helvoort-Postulart D, Prins MH, Neumann M, Dirksen CD. Does the inclusion of a cost attribute result in different preferences for the surgical treatment of primary basal cell carcinoma? A comparison of two discrete-choice experiments. Pharmacoeconomics. 2010;28:507–20.
Gerard K, Salisbury C, Street D, Pope C, Baxter H. Is fast access to general practice all that should matter? A discrete choice experiment of patients’ preferences. J Health Serv Res Policy. 2008;13(Suppl 2):3–10.
Gidman W, Elliott R, Payne K, Meakin GH, Moore J. A comparison of parents and pediatric anesthesiologists’ preferences for attributes of child daycase surgery: a discrete choice experiment. Paediatr Anaesth. 2007;17:1043–52.
Reed Johnson F, Ozdemir S, Phillips KA. Effects of simplifying choice tasks on estimates of taste heterogeneity in stated-choice surveys. Soc Sci Med. 2010;70:183–90.
Özdemir S, Johnson FR, Hauber AB. Hypothetical bias, cheap talk, and stated willingness to pay for health care. J Health Econ. 2009;28:894–901.
Rockers PC, Jaskiewicz W, Wurts L, Kruk ME, Mgomella GS, Ntalazi F, et al. Preferences for working in rural clinics among trainee health professionals in Uganda: a discrete choice experiment. BMC Health Serv Res. 2012;12:212.
Scott A, Witt J, Duffield C, Kalb G. What do nurses and midwives value about their jobs? Results from a discrete choice experiment. J Health Serv Res Policy. 2014;20:31–8.
Song K, Scott A, Sivey P, Meng Q. Improving Chinese primary care providers’ recruitment and retention: a discrete choice experiment. Health Policy Plan. 2015;30:68–77.
Tinelli M, Nikoloski Z, Kumpunen S, Knai C, Brinovec RP, Warren E, et al. Decision-making criteria among European patients: exploring patient preferences for primary care services. Eur J Public Health. 2015;25:3–9.
Hole AR. Small-sample properties of tests for heteroscedasticity in the conditional logit model. Health, Econometrics and Data Group, University of York. HEDG Working Paper 06/04. May 2006. Available at: https://www.york.ac.uk/media/economics/documents/herc/wp/06_04.pdf,
Fiebig D, Keane M, Louviere J, Wasi N. The generalized multinomial logit model: accounting for scale and coefficient heterogeneity. Mark Sci. 2010;29:393–421.
Hess S, Rose JM. Can scale and coefficient heterogeneity be separated in random coefficients models? Transportation. 2012;39:1225–39.
Magidson J, Vermunt J. Removing the scale factor confound in multinomial logit choice models to obtain better estimates of preference. Sawtooth Software; 2007. p. 1–18.
Swait J, Louviere J. The role of the scale parameter in the estimation and comparison of multinomial logit choice models. J Mark Res. 1993;30:305–14.
Chow GC. Tests of equality between sets of coefficients in two linear regressions. Econometrica. 1960;28:591–605.
Louviere J, Hensher D, Swait J. Stated choice methods: analysis and application. Cambridge: Cambridge University Press; 2000.
DeShazo JR, Fermo G. Designing choice sets for stated preference methods: the effects of complexity on choice consistency. J Environ Econ Manag. 2002;44:123–43.
Hole AR. Stata modules. 2017. Available at: https://www.sheffield.ac.uk/economics/people/hole/stata.
Van Helvoort-Postulart D, Dellaert BGC, Van Der Weijden T, Von Meyenfeldt MF, Dirksen CD. Discrete choice experiments for complex health-care decisions: does hierarchical information integration offer a solution? Health Econ. 2008;18:903–20.
Blaauw D, Erasmus E, Pagaiya N, Tangcharoensathein V, Mullei K, Mudhune S, et al. Policy interventions that attract nurses to rural areas: a multicountry discrete choice experiment. Bull World Health Organ. 2010;88:350–6.
Zhou M, Thayer WM, Bridges JFP. Using latent class analysis to model preference heterogeneity in health: a systematic review. Pharmacoeconomics. 2018;36(2):175–87.
Rigby D, Burton M, Pluske J. Preference stability and choice consistency in discrete choice experiments. Environ Resour Econ. 2016;65:441–61.
Burton M, Davis KJ, Kragt ME. Interpretation issues in heteroscedastic conditional logit models. School of Agricultural and Resource Economics, The University of Western Australia. Working Paper 1603. 15 May 2016. Crawley.
Louviere JJ, Meyer RJ, Bunch DS, Carson R, Hanemann WM, Hensher D, et al. Combining sources of preference data for modeling complex decision processes. Mark Lett. 1999;103:205–17.
Louviere J, Eagle T. Confound it! That pesky little scale constant messes up our convenient assumptions. Sequem, WA: Sawtooth Software; 2006. Available at: https://www.statisticalinnovations.com/wp-content/uploads/Louviere.Eagle_.2006.pdf.
Acknowledgements
The researchers would like to thank Dr. Ewan Gray (The University of Edinburgh) and Logan Trenaman (The University of British Columbia) who screened abstracts as part of the initial creation of a database of discrete choice experiments in healthcare.
Funding
Caroline M. Vass and Katherine Payne were supported in the preparation and submission of this article by Mind the Risk, from The Swedish Foundation for Humanities and Social Sciences. The views and opinions expressed are those of the authors, and not necessarily those of other Mind the Risk members or The Swedish Foundation for Humanities and Social Sciences.
Author information
Authors and Affiliations
Contributions
SJW conceptualised the project, screened abstracts in the systematic review, conducted data extraction, contributed to writing the paper and approved the final manuscript. CMV conceptualised the project, updated the existing systematic review, screened abstracts in the systematic review, contributed to writing the paper and approved the final manuscript. GS conceptualised the project, screened abstracts in the systematic review, contributed to writing the paper and approved the final manuscript. MB conceptualised the project, contributed to writing the paper and approved the final manuscript. DGF conceptualised the project, contributed to writing the paper and approved the final manuscript. KP conceptualised the project, updated the existing systematic review, contributed to writing the paper and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Stuart Wright, Caroline Vass, Gene Sim, Michael Burton, Denzil Fiebig and Katherine Payne declare that they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wright, S.J., Vass, C.M., Sim, G. et al. Accounting for Scale Heterogeneity in Healthcare-Related Discrete Choice Experiments when Comparing Stated Preferences: A Systematic Review. Patient 11, 475–488 (2018). https://doi.org/10.1007/s40271-018-0304-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-018-0304-x