Abstract
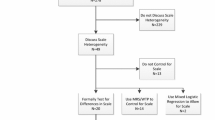
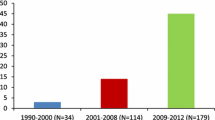
Discrete choice experiments (DCEs) are used to quantify the preferences of specified sample populations for different aspects of a good or service and are increasingly used to value interventions and services related to healthcare. Systematic reviews of healthcare DCEs have focussed on the trends over time of specific design issues and changes in the approach to analysis, with a more recent move towards consideration of a specific type of variation in preferences within the sample population, called taste heterogeneity, noting rises in the popularity of mixed logit and latent class models. Another type of variation, called scale heterogeneity, which relates to differences in the randomness of choice behaviour, may also account for some of the observed ‘differences’ in preference weights. The issue of scale heterogeneity becomes particularly important when comparing preferences across subgroups of the sample population as apparent differences in preferences could be due to taste and/or choice consistency. This primer aims to define and describe the relevance of scale heterogeneity in a healthcare context, and illustrate key points, with a simulated data set provided to readers in the Online appendix.

Similar content being viewed by others
Notes
In some studies, preferences are allowed to vary by individual, introducing the subscript, n: \(\beta_{n,k}\). This primer focuses on scale heterogeneity and not preference heterogeneity. For this reason, issues relating to the joint identification of preference and scale heterogeneity are not addressed in this primer. We refer readers to Hess and Train [36] for a description unsuitable for this primer.
The MNL is often used interchangeably with ‘conditional logit’. In this case, we use the term ‘multinomial logit’ or ‘MNL’ as this is commonly used in the literature cited, but acknowledge estimations in Stata for this definition will use the clogit command.
Comparisons of coefficients estimated with different models can also be problematic. For example, estimating a probit model with a standard normal distribution (with a variance of 1), and a logit model with a standard logistic distribution with a variance of \(\frac{{\pi^{2} }}{3}\), will result in a difference of estimated coefficients of \(\sqrt {\frac{{\pi^{2} }}{3}}\) or 1.8. For a worked example, see Part D of the Technical Appendix, and, for more details, see Chapters 2 and 3 of Train [37].
For simplicity, alternative specific constants are not included in this model. It is noted in some literature that alternative specific constants should also not be included on these coefficient plots [19].
Part E of the Technical Appendix generates data with different scale and preference parameters in the two samples, and example estimation where the equivalence of the preference parameters is rejected, even once one has controlled for scale.
References
De Bekker-Grob EW, Ryan M, Gerard K. Discrete choice experiments in health economics: a review of the literature. Health Econ. 2012;21(2):145–72.
Clark M, Determann D, Petrou S, Moro D, de Bekker-Grob EW. Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics. 2014;32(9):883–902.
Vass C, Rigby D, Payne K. The role of qualitative research methods in discrete choice experiments: a systematic review and survey of authors. Med. Decis. Mak. 2017;37(3):298–313.
Lancaster KJ. A new approach to consumer theory. J Polit Econ. 1966;74(2):132–57.
Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–77.
McFadden D. The choice theory approach to market research. Mark Sci. 1986;5(4):275–97.
Lancsar E, Fiebig DG, Hole AR. Discrete choice experiments: a guide to model specification, estimation and software. Pharmacoeconomics. 2017;35(7):697–716.
Wright SJ, Vass CM, Sim G, Burton M, Fiebig DG, Payne K. Accounting for scale heterogeneity in health-related discrete choice experiments: the current state of play. Patient. 2017. (In Review).
Hauber AB, González JM, Groothuis-Oudshoorn CGM, Prior T, Marshall DA, Cunningham C, et al. Statistical methods for the analysis of discrete choice experiments: a report of the ispor conjoint analysis good research practices task force. Value Health. 2016;19(4):300–15.
Viney R, Lancsar E, Louviere J. Discrete choice experiments to measure consumer preferences for health and healthcare. Expert Rev Pharmacoecon Outcomes Res. 2002;2(4):319–26.
Thurstone L. A law of comparative judgment. Psychol Rev. 1927;34(4):273–86.
Marschak J. Binary-choice constraints and random utility indicators. Math. Methods Soc. Sci. Dordrecht: Springer Netherlands;1960:312–29.
Louviere J, Hensher D, Swait J. Stated choice methods: analysis and application. Cambrdige: Cambridge University Press; 2000.
Payne K, Fargher EA, Roberts SA, Tricker K, Elliott RA, Ratcliffe J, et al. Valuing pharmacogenetic testing services: a comparison of patients’ and health care professionals’ preferences. Value Health. 2011;14(1):121–34.
Najafzadeh M, Johnston KM, Peacock SJ, Connors JM, Marra MA, Lynd LD, et al. Genomic testing to determine drug response: measuring preferences of the public and patients using discrete choice experiment (dce). BMC Health Serv Res. 2013;13(1):454.
Morillas C, Feliciano R, Catalina PF, Ponte C, Botella M, Rodrigues J, et al. Patients’ and physicians’ preferences for type 2 diabetes mellitus treatments in spain and portugal: a discrete choice experiment. Patient Prefer Adherence. 2015;9:1443–58.
Wooldridge J. Introductory econometrics. 4th ed. Chula Vista: South Western College; 2008.
Burton M, Davis KJ, Kragt ME. Interpretation issues in heteroscedastic conditional logit models. Working paper 1603. Crawley: School of Agriculture and Resource Economics, University of Western Australia; 2016.
Swait J, Louviere J. The role of the scale parameter in the estimation and comparison of multinomial logit models. J Mark Res. 1993;30(3):305–14.
Hensher D, Louviere J, Swait J. Combining sources of preference data. J Econ. 1998;89(1–2):197–221.
Hole AR. Small-sample properties of tests for heteroscedasticity in the conditional logit model. Econ Bull. 2006;3:1–14.
StataCorp. Stata statistical software: release 12. College Station: StataCorp LP. 2011.
Hole AR. Clogithet: stata module to estimate heteroscedastic conditional logit model. Stat. Softw. Components. 2006;(S456737).
LIMDEP; Nlogit. Econometric Software, Inc.; 2015.
Bech M, Kjaer T, Lauridsen J. Does the number of choice sets matter? results from a web survey applying a discrete choice experiment. Health Econ. 2011;20(3):273–86.
Flynn T, Louviere J, Peters T, Coast J. Using discrete choice experiments to understand preferences for quality of life. variance-scale heterogeneity matters. Soc Sci Med. 2010;70(12):1957–65.
DeShazo JR, Fermo G. Designing choice sets for stated preference methods: the effects of complexity on choice consistency. J Environ Econ Manage. 2002;44(1):123–43.
Pedersen LB, Kjaer T, Kragstrup J, Gyrd-Hansen D. Do general practitioners know patients’ preferences? an empirical study on the agency relationship at an aggregate level using a discrete choice experiment. Value Health. 2012;15(3):514–23.
Vass CM, Rigby D, Payne K. Investigating the heterogeneity in women’s preferences for breast screening: does the communication of risk matter? Value Health. doi:10.1016/j.jval.2017.07.010.
Hensher D, Greene W. The mixed logit model: the state of practice. Transport. 2003;30:133–76.
Greene WH, Hensher D. A latent class model for discrete choice analysis: contrasts with mixed logit. Transp Res Part B Methodol. 2003;37(8):681–98.
Fiebig D, Keane M, Louviere J, Wasi N. The generalized multinomial logit model: accounting for scale and coefficient heterogeneity. Mark Sci. 2010;29(3):393–421.
Gu Y, Hole AR, Knox S. Fitting the generalized multinomial logit model in stata. Stata J. 2013;13(2):382–97.
Latent Gold. Belmont: Statistical Innovations; 2013.
Hess S, Rose JM. Can scale and coefficient heterogeneity be separated in random coefficients models? Transportation. 2012;39(6):1225–39.
Hess S, Train K. Correlation and scale in mixed logit models. J. Choice Model. 2017;23:1–8.
Train K. Discrete choice methods with simulation. 2nd ed. Cambridge: Cambridge University Press; 2009.
Acknowledgements
The authors wish to thank Dr Arne Hole from the University of Sheffield for reading and commenting on a draft of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors were involved in the drafting and editing of the manuscript, and Michael Burton was also involved in the simulation of choice data.
Corresponding author
Ethics declarations
Ethical approval
No ethical approval was required for this study.
Conflict of interest
Caroline M. Vass and Katherine Payne were supported in the preparation and submission of this paper by Mind the Risk, from The Swedish Foundation for Humanities and Social Sciences. The views and opinions expressed are those of the authors and are not necessarily those of other Mind the Risk members or The Swedish Foundation for Humanities and Social Sciences. Stuart Wright and Michael Burton declare that they have no conflicts of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vass, C.M., Wright, S., Burton, M. et al. Scale Heterogeneity in Healthcare Discrete Choice Experiments: A Primer. Patient 11, 167–173 (2018). https://doi.org/10.1007/s40271-017-0282-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-017-0282-4