Abstract
Background
The Disabilities of the Arm, Shoulder and Hand (DASH) Questionnaire is the most commonly applied patient-reported outcome measure used to assess disability and functioning in clinical research and practice for patients with injuries and diseases of the upper extremities. The objective of this study was to assess whether the DASH is a valid and reliable questionnaire to measure disability and functioning in patients with hand injuries and diseases using Rasch analysis.
Methods
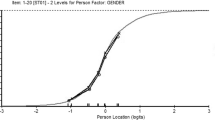
We performed a psychometric study using data derived from two multicentre studies carried out to develop the International Classification of Functioning, Disability and Health (ICF) Core Sets for Hand Conditions. We analysed the data of 417 patients recruited in a clinical setting and suffering from hand injuries (e.g. finger fracture, flexor tendon injury) or diseases (e.g. carpal tunnel syndrome, rhizarthrosis). We examined whether the DASH fulfilled the assumptions for its use as a measure by applying a partial credit model and testing for differential item functioning for sex and age.
Results
Bifactor analysis revealed problems with the underlying latent trait of functioning and disability. Rasch analysis raised further issues, including disordered thresholds for eight items and misfit in nine items. One item showed Differential Item Functioning for sex.
Conclusion
The study reveals that some DASH items do not fit the underlying trait that the DASH aims to measure. Further studies using Rasch analysis are needed to compare our findings with results of studies involving other target groups (e.g. patients with injuries of the upper arm and shoulder).



Similar content being viewed by others
References
Hobart JC, Cano SJ, Zajicek JP, Thompson AJ. Rating scales as outcome measures for clinical trials in neurology: problems, solutions, and recommendations. Lancet Neurol. 2007;6(12):1094–105.
Smith MV, Calfee RP, Baumgarten KM, Brophy RH, Wright RW. Upper extremity-specific measures of disability and outcomes in orthopaedic surgery. J Bone Joint Surg Am. 2012;94(3):277–85.
Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg Am. 1998;23(4):575–87.
Kirkley A, Alvarez C, Griffin S. The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: the Western Ontario Rotator Cuff Index. Clin J Sport Med. 2003;13(2):84–92.
Levine DW, Simmons BP, Koris MJ, Daltroy LH, Hohl GG, Fossel AH, et al. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993;75(11):1585–92.
Davis AM, Beaton DE, Hudak P, Amadio P, Bombardier C, Cole D, et al. Measuring disability of the upper extremity: a rationale supporting the use of a regional outcome measure. J Hand Ther. 1999;12(4):269–74.
Bialocerkowski AE. Difficulties associated with wrist disorders–a qualitative study. Clin Rehabil. 2002;16(4):429–40.
Wong JY. Time off work in hand injury patients. J Hand Surg Am. 2008;33(5):718–25.
Hill S, Dziedzic KS, Ong BN. The functional and psychological impact of hand osteoarthritis. Chronic Illn. 2010;6(2):101–10.
World Health Organization. International Classification Of Functioning, Disability and Health. Geneva: World Health Organization; 2001.
Coenen M, Kus S, Rudolf KD, Muller G, Berno S, Dereskewitz C, et al. Do patient-reported outcome measures capture functioning aspects and environmental factors important to individuals with injuries or disorders of the hand? J Hand Ther. 2013;26(4):332–42 (quiz 42).
Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (Disabilities Of The Arm, Shoulder and Hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29(6):602–8.
Kus S, van de Ven-Stevens LA, Coenen M, Berno S, Kollerits B, Cieza A. What is our knowledge of functioning and disability in hand conditions based on? Arch Phys Med Rehabil. 2011;92(8):1326–32.
Beaton DE, Davis AM, Hudak PL, McConnell S. The DASH (Disabilities of the Arm, Shoulder and Hand) outcome measure: what do we know about it now? Br J Hand Ther. 2001;6(4):109–18.
Beaton DE, Katz JN, Fossel AH, Wright JG, Tarasuk V, Bombardier C. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128–46.
Gummesson C, Atroshi I, Ekdahl C. The Disabilities of the Arm, Shoulder and Hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11–6.
Offenbaecher M, Ewert T, Sangha O, Stucki G. Validation of a German version of the Disabilities of Arm, Shoulder, and Hand Questionnaire (DASH-G). J Rheumatol. 2002;29(2):401–2.
SooHoo NF, McDonald AP, Seiler JG 3rd, McGillivary GR. Evaluation of the construct validity of the DASH questionnaire by correlation to the SF-36. J Hand Surg Am. 2002;27(3):537–41.
Germann G, Harth A, Wind G, Demir E. Standardisation and validation of the German version 2.0 of the Disability of Arm, Shoulder, Hand (DASH) Questionnaire. Unfallchirurg. 2003;106(1):13–9.
Lehman LA, Woodbury M, Velozo CA. Examination of the factor structure of the Disabilities of the Arm, Shoulder, and Hand Questionnaire. Am J Occup Ther. 2011;65(2):169–78.
Franchignoni F, Giordano A, Sartorio F, Vercelli S, Pascariello B, Ferriero G. Suggestions for refinement of the Disabilities of the Arm, Shoulder and Hand outcome measure (DASH): a factor analysis and Rasch validation study. Arch Phys Med Rehabil. 2010;91(9):1370–7.
Cheng HM, Sampaio RF, Mancini MC, Fonseca ST, Cotta RM. Disabilities of the Arm, Shoulder and Hand (DASH): factor analysis of the version adapted to Portuguese/Brazil. Disabil Rehabil. 2008;30(25):1901–9.
Mousavi SJ, Parnianpour M, Abedi M, Askary-Ashtiani A, Karimi A, Khorsandi A, et al. Cultural adaptation and validation of the Persian version of the Disabilities of the Arm, Shoulder and Hand (DASH) outcome measure. Clin Rehabil. 2008;22(8):749–57.
Beaton DE, Wright JG, Katz JN, Upper ExtremityCollaborative G. Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am. 2005;87(5):1038–46.
Cano SJ, Barrett LE, Zajicek JP, Hobart JC. Beyond the reach of traditional analyses: using Rasch to evaluate the DASH in people with multiple sclerosis. Mult Scler. 2011;17(2):214–22.
Rudolf KD, Kus S, Chung KC, Johnston M, LeBlanc M, Cieza A. Development of the international classification of functioning, disability and health core sets for hand conditions—results of the World Health Organization International Consensus process. Disabil Rehabil. 2012;34(8):681–93.
Kus S, Oberhauser C, Cieza A. Validation of the brief international classification of functioning, disability, and health (ICF) core set for hand conditions. J Hand Ther. 2012;25(3):274–86 (quiz 87).
Kus S, Dereskewitz C, Wickert M, Schwab M, Eisenschenk A, Steen M, et al. Validation of the comprehensive international classification of functioning, disability and health (ICF) core set for hand conditions. Hand Therapy. 2011;16(3):58–66.
Cronbach L. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334.
Revelle W, Zinbarg R. Coefficients alpha, beta, omega, and the glb: comments on Sijtsma. Psychometrika. 2009;74(1):145–54.
Roscino A, Pollice A. A generalization of the polychoric correlation coefficient. In: Zani S, Cerioli A, Riani M, Vichi M, editors. Data analysis, classification and the forward search. Berlin, Heidelberg: Springer; 2006. p. 135–42.
Trochim W. The research methods knowledge base, 2nd edition. Internet WWW page (version current as of October 20, 2006) 2016 [updated October 20, 2006; cited 2016 March 22, 2016]. http://www.socialresearchmethods.net/kb/.
Jennrich RI, Bentler PM. Exploratory bifactor analysis. Psychometrika. 2011;76(4):537–49.
Reise SP. The rediscovery of bifactor measurement models. Multivar Behav Res. 2012;47(5):667–96.
Buja A, Eyuboglu N. Remarks on parallel analysis. Multivar Behav Res. 1992;27(4):509–40.
Reeve BB, Fayers P. Applying item response theory modeling for evaluating questionnaire item and scale properties. In: Fayers P, Hays RD, editors. Assessing quality of life in clinical trials: methods of practice. 2nd ed. Oxford: Oxford University Press; 2005. p. 55–73.
Elhan AH, Küçükdeveci AA, Tennant A. The Rasch measurement model. In: Franchignoni F, editor. Research issues in physical and rehabilitation medicine. Pavia: Maugeri Foundation Books; 2010. p. 89–102.
Tesio L. Measuring behaviours and perceptions: Rasch analysis as a tool for rehabilitation research. J Rehabil Med. 2003;35(3):105–15.
Tennant A, Conaghan PG. The Rasch measurement model in rheumatology: what is it and why use it? When should it be applied, and what should one look for in a Rasch paper? Arthritis Rheum. 2007;57(8):1358–62.
Pallant JF, Tennant A. An introduction to the Rasch measurement model: an example using the Hospital Anxiety and Depression Scale (HADS). Br J Clin Psychol. 2007;46(Pt 1):1–18.
Smith AB, Rush R, Fallowfield LJ, Velikova G, Sharpe M. Rasch fit statistics and sample size considerations for polytomous data. BMC Med Res Methodol. 2008;8(1):33.
Bond TG, Fox CM. Applying the Rasch model: fundamental measurement in the human sciences. 2nd ed. Mahwah: Lawrence Erlbaum Associates, Inc.; 2007.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statisctical Computing; 2013.
Mair P, Hatzinger R, Maier MJ. eRm: Extended Rasch Modeling. 0.15-7. 2016. http://erm.r-forge.rproject.org/. Accessed 20 Dec 2016.
Choi SW, Gibbons LE, Crane PK. lordif: an R package for detecting differential item functioning using iterative hybrid ordinal logistic regression/item response theory and Monte Carlo simulations. J Stat Softw. 2011;39(8):1–30.
Acknowledgements
We would like to thank all persons involved in the data collection at (1) the Department of Hand Surgery, Plastic and Microsurgery at the BG Klinikum Hamburg, (2) the Department of Plastic and Hand Surgery, Burns Unit at the BG Klinikum Bergmannstrost Halle, (3) the Department of Hand Surgery, Plastic and Microsurgery at the Unfallkrankenhaus Berlin and (4) the Department of Hand, Plastic, Reconstructive and Burns Surgery at the BG Klinik Tübingen.
Author contributions
Michaela Coenen initiated and supervised the study, contributed to the design of the study and revised the draft version of the manuscript. Kathrin Braitmayer performed the data analysis, interpreted the results and drafted the manuscript. Cornelia Oberhauser supervised the data analysis and contributed to the writing and revising of the manuscript. Caroline Dereskewitz and Klaus-Dieter Rudolf contributed to the design of the study, managed and supervised the data collection of the two former studies and contributed to the writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The two former studies that provided the data used in this study were funded by the German Social Accident Insurance, DGUV. The authors of this publication are responsible for its content.
Disclosure of potential conflicts of interest
K Braitmayer, C. Dereskewitz, C. Oberhauser, K.-D. Rudolf and M. Coenen declare that they have no competing interests.
Statement on human rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Statement on the welfare of animals
This article does not include any animal studies performed by any of the authors.
Informed consent
For this psychometric study, we used data from two former studies. Both studies were approved by the Ethics Committee of the Medical Association, Hamburg, and the Ethics Committee of the Ludwig-Maximilians-Universität (LMU), Munich. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Braitmayer, K., Dereskewitz, C., Oberhauser, C. et al. Examination of the Applicability of the Disabilities of the Arm, Shoulder and Hand (DASH) Questionnaire to Patients with Hand Injuries and Diseases Using Rasch Analysis. Patient 10, 367–376 (2017). https://doi.org/10.1007/s40271-016-0212-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-016-0212-x