Abstract
Background
Osteoarthritis (OA) causes substantial pain and reduced health-related quality of life (HRQL). Although opioid analgesics are commonly used, the relative benefits of different opioids are poorly studied. Transdermal buprenorphine (TDB) offers an alternative to oral opioids for the treatment of moderate-to-severe chronic pain. This observational study of people with OA pain assessed satisfaction, HRQL and medication adherence.
Methods
Patients in the UK with self-reported knee and/or hip OA who had been receiving one or more of TDB, co-codamol (an oral paracetamol/codeine combination) and tramadol for at least 1 month completed an online or telephone questionnaire. Medication satisfaction scores, HRQL scores (Short-Form 36 [SF-36]), medication adherence (Morisky Medication Adherence Scale [MMAS™]), adverse events and treatment discontinuations were recorded. Linear and logistic regression models were used to compare the treatment effect of TDB with co-codamol or tramadol.
Results
Overall, 966 patients met the inclusion criteria; 701 were taking only one of the target medications (TDB: 85; co-codamol: 373; tramadol: 243). The largest age group was 50–59 years and 76.0 % of patients were female. The TDB group was younger, with more male patients, therefore the statistical models were adjusted for age and sex. Medication satisfaction scores were significantly higher in the TDB group than the other two groups (TDB vs. co-codamol: 3.56, 95 % confidence interval [CI] 1.90–6.68, p < 0.0001; TDB vs. tramadol: 3.22, 95 % CI 1.67–6.20, p = 0.0005). Physical Component Summary scores for HRQL and mean adherence were also higher in the TDB group, while Mental Component Summary HRQL scores were similar across the three groups.
Conclusions
Patients with knee and/or hip OA pain treated with TDB were more satisfied and more adherent with their medication, and reported higher Physical Component Summary HRQL scores than those treated with co-codamol or tramadol, although demographic differences were observed between groups.
Similar content being viewed by others
Low-dose transdermal buprenorphine (TDB) is an effective alternative to oral opioids such as co-codamol and tramadol for the treatment of moderate-to-severe osteoarthritis (OA) pain. |
This prospective, observational study showed that patients with OA whose pain was treated with TDB reported increased satisfaction with their medication, better adherence, and improved Physical Component Summary health-related quality of life scores compared with patients treated with co-codamol or tramadol. |
Physicians should consider patient satisfaction and quality of life when prescribing analgesics for chronic pain. |
1 Introduction
Osteoarthritis (OA) is a debilitating condition, characterised by pain, joint inflammation and joint stiffness, which causes a substantial degree of physical disability. OA commonly affects the knee or the hip, and in England it is estimated that 4.11 million people have knee OA (approximately 18 % of the population aged 45 years and over) and 2.46 million have hip OA (approximately 11 % of the population aged 45 years and over) [1]. Figures from the US suggest approximately 13 % of women and 10 % of men over 60 years of age have knee OA [2].
The pain caused by OA can have a substantial impact on patients’ quality of life. In a 2012 online survey of OA patients in the UK [3], 52 % of the 2001 respondents reported that OA had a large impact on their life, 71 % had persistent pain even after taking their prescribed pain medication, and 12 % said their pain was often unbearable.
Opioid analgesics are commonly used to treat chronic musculoskeletal pain, including OA pain. The National Institute for Health and Care Excellence (NICE) OA guidelines [4] recommend using opioids after other analgesics such as paracetamol and oral non-steroidal anti-inflammatory drugs (NSAIDs) have failed or are contraindicated. Similarly, the American College of Rheumatology guidelines [5] recommend opioids for the treatment of knee or hip OA pain in patients who have not responded to initial non-opioid treatment. Tramadol is considered separately to other opioids and is suggested as a first-line treatment. In their guidelines for the treatment of knee OA, The American Academy of Orthopaedic Surgeons [6] recommended the use of tramadol but were unable to recommend other opioids or pain patches due to a lack of published evidence that met their inclusion criteria.
At clinically prescribed doses, buprenorphine acts as a full μ-opioid agonist, and has a long duration of action [7–9]. It has been shown to have no analgesic ceiling effect, immunosuppressive activity or effect on gonadal hormones [7, 8, 10, 11]. In addition, the dose of buprenorphine does not need to be adjusted in elderly patients [12–15] or those with renal impairment [16].
Buprenorphine is available in the UK as transdermal patches (TDB), sublingual tablets, and as a solution for injection. This study focused on low-dose 7-day TDB, containing buprenorphine 5–20 mg with a nominal release rate of 5–20 μg/h. These patches are indicated for moderate chronic non-cancer pain, and have been shown to have comparable efficacy to oral opioids for the treatment of OA pain [17]. Two randomised controlled trials (RCTs) have demonstrated that 7-day TDB is non-inferior to co-codamol (an oral paracetamol/codeine combination) and tramadol for the treatment of OA pain [18, 19]. In addition, a retrospective database study into the use of 7-day TDB in primary care [20] found that significantly more patients persisted with their treatment after 6 and 12 months compared with codeine, dihydrocodeine and tramadol.
Tramadol has a dual mode of action as a μ-opioid agonist and as a weak serotonin and noradrenaline reuptake inhibitor. It is available in the UK as immediate- or prolonged release oral tablets or capsules, as an oral solution, and as a solution for injection or infusion. The maximum recommended dose is 400 mg/day [21].
Co-codamol is a combination analgesic containing codeine and paracetamol, which is commonly used in the UK. Three different dose strengths are available: 8/500 (codeine 8 mg/paracetamol 500 mg), 15/500 and 30/500. Codeine is a μ-opioid agonist and co-codamol is available in the UK as oral tablets or capsules. The maximum recommended daily dose is codeine 240 mg and paracetamol 4 g [21]. Codeine is a prodrug that is metabolised to morphine via cytochrome P450 (CYP) 2D6 in the liver to exert its analgesic effect.
Clinical trial data are essential for robust comparisons of the efficacy of different treatments but rarely reflect the way medicines are used in practice. Real-world evidence, such as observational studies conducted without any healthcare professional involvement, can provide useful insights into how patients really use their medications, and may help to inform prescribing decisions.
Despite opioid analgesics being recommended for suitable patients with OA pain, few studies have compared the relative benefits of different opioids. Previous studies have compared TDB with co-codamol and tramadol in an RCT [18, 19] and general practice setting [20], but not from a patient perspective.
We conducted an observational study to assess TDB, co-codamol and tramadol in patients with OA pain in a real-world, non-interventional setting. Our primary objective was to establish whether there were any differences between the study medications in patient-reported outcomes, including medication satisfaction, health-related quality of life (HRQL) and adherence to treatment.
2 Method
2.1 Patients and Study Design
This was a UK-based observational study, conducted in people with OA of the knee and/or hip, without any intervention from a healthcare professional. Questionnaires were completed online by the participants or conducted by telephone interview. Recruitment was through social media, general practitioner (GP) surgeries and pharmacies, and advertisements in newspapers and on patient websites. Please refer to the electronic supplementary material (ESM) for further details of the questionnaire.
Participants were included in the study if they had a self-reported diagnosis of knee and/or hip OA, and had been prescribed one of the target analgesic medications (low-dose 7-day TDB, co-codamol or tramadol) for their OA pain for at least 1 month prior to study entry.
The study was conducted between September 2012 and March 2013. Responses were measured at baseline (the first questionnaire), and after 1, 2 and 3 months. Following completion of the baseline questionnaire, patients were sent reminders to complete the follow-up surveys. For each follow-up, participants had up to 14 days to complete the questionnaire after receiving a reminder, and each participant was contacted by email, SMS or telephone at least three times to complete each follow-up survey.
The study was performed in accordance with the regulations and guidelines governing medical practice and ethics in the UK. Study documents were reviewed and approved by the appointed Research Ethics Committee (East of Scotland Research Ethics Service [EoSRES]; ref: LR/12/ES/0093), and all patients were provided with information about the study and asked to consent either by telephone or online before completing the baseline questionnaire.
2.2 Outcomes and Assessments
2.2.1 Patient Satisfaction
Satisfaction with current pain medication was assessed at baseline using a 6-point Likert scale comprising ‘Very satisfied’, ‘Satisfied’, ‘Neither satisfied nor dissatisfied’, ‘Dissatisfied’, ’Very dissatisfied’ and ‘No opinion’.
2.2.2 Health-Related Quality of Life (HRQL)
HRQL during the previous 4 weeks was assessed at baseline and in each follow-up questionnaire using the Short-Form 36, version 2 (SF-36v2; standard form) health survey, which measures eight different areas of patients’ health: physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional and mental health. Scores were recorded for each of these areas, and aggregate physical and mental scores (the Physical Component Summary and Mental Component Summary) were calculated. Scores range from 0–100, with 0 corresponding to low HRQL and 100 corresponding to high HRQL.
2.2.3 Adherence
Adherence was measured at baseline and in each follow-up questionnaire using the Morisky Medication Adherence Scale (MMAS™), a set of eight questions designed to identify medication use behaviour that can indicate non-adherence. Scores from 0 to 8 are possible, with a score of <6 indicating low adherence, 6–7 indicating medium adherence, and 8 indicating high adherence.
2.2.4 Adverse Events (AEs)
AEs related to treatment were recorded at baseline. Reasons for discontinuation were also recorded at baseline and in each follow-up questionnaire, which included discontinuations because of side effects.
2.3 Statistical Methods
Participants who met the inclusion criteria and had partially or fully completed at least the baseline questionnaire were included in the statistical analysis.
The full analysis population refers to all patients and their actual treatment groups at the time of follow-up. Due to the number of patients who changed treatment or dropped out of the study, analysis for the follow-up questionnaires was carried out on two study populations:
-
Intention-to-treat (ITT) population: analysis of subjects as per their treatment groups at baseline, even if their treatment group later changed.
-
Per protocol (PP) population: analysis of subjects who remained on the same treatment from baseline.
Follow-up data have been reported in this study using the PP population.
Data were analysed descriptively; for categorical variables, the number and percentage falling into each category were reported. Percentages were calculated from total numbers excluding any missing observations. For continuous variables, the mean, standard deviation (SD), median, interquartile range (IQR) and range were reported.
Estimates for the treatment effect of single target medications (co-codamol and tramadol only) were obtained for continuous and binary outcomes (medication satisfaction, HRQL and treatment adherence) using linear and logistic regression models, respectively, compared with TDB. Each model included the treatment variable, with comparisons focusing on the treatment effect of TDB compared with the other two treatments. p-Values were provided for the differences across all three treatment groups and the comparisons between TDB and co-codamol, and TDB and tramadol. The estimates (or odds ratios where relevant) and a 95 % confidence interval for each treatment effect were also provided for the comparisons of TDB with co-codamol and with tramadol to show the likelihood of the outcome occurring in patients treated with TDB compared with patients treated with the other medication. Initial models were unadjusted, containing a covariate for treatment only. As subjects in the TDB group were more likely to be younger and/or male than those in the other groups, age- and sex-adjusted models were also investigated to remove potential bias in the results.
3 Results
3.1 Patient Characteristics
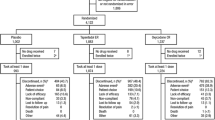
A total of 1011 patients completed the questionnaire, with 966 meeting the inclusion criteria (Fig. 1). Most of the patients (76.0 %) were female, and 91.3 % of the study population had been diagnosed with OA for 1 year or more. Some of the patients were taking more than one of the target medications; therefore, to enable more accurate comparisons between the target medications, subjects taking a single target medication were analysed separately, with patients categorised into the TDB-only, co-codamol-only and tramadol-only groups.
Patient selection process. Asterisk target medications: 7-day TDB, co-codamol or tramadol. These figures are taken from the full analysis population. The follow-up numbers include participants taking one target medication at the time of each follow-up questionnaire, although participants may have moved from another medication group or may not have completed all follow-up questionnaires. OA osteoarthritis, TDB transdermal buprenorphine
3.1.1 Age and Sex Distribution
The study population included a range of ages, with the largest proportion aged between 50 and 59 years (Table 1), which was similar in all groups except the TDB group, in which most patients were under 40 years of age. Similarly, the sex distribution of the TDB group was different to the other groups. The total analysis population was 76.0 % female, with similar proportions in the co-codamol (75.3 %) and tramadol (81.1 %) groups. In the TDB group, 45.8 % were female. Age- and sex-adjusted analysis was performed to take into account differences in age and sex distribution between the groups (see the ESM for analysis results).
3.1.2 Comorbidities
Many of the patients had comorbidities alongside their OA, with a mean of 1.4 concomitant conditions across all groups. The most common condition was depression, seen in just over 1 in 10 patients in the TDB-only group, compared with approximately one-third in the co-codamol- and tramadol-only groups. High blood pressure, high cholesterol and type II diabetes were the next most commonly reported conditions.
3.1.3 Target Medication Dose
In all groups, most patients had been taking their target medication for 6 months or more (89.4 % in the TDB group, 89.3 % in the co-codamol group and 91.8 % in the tramadol group).
The median strength of TDB used was 15 μg/h over 7 days. This strength was used by 32.9 % of patients in the TDB group. The lowest TDB strength was 5 µg/h, taken by 14.1 % of patients, and the highest strength was 30 µg/h (8.2 % of patients).
In the co-codamol group, the median dose was 180/3000 mg/day (six 30/500 mg tablets, taken by 55.8 % of patients). This was also the highest dose taken. The lowest dose was 48/3000 mg/day (six 8/500 mg tablets, taken by 23.6 % of patients).
The median dose in the tramadol group was 300 mg/day (taken by 58.4 % of patients), the lowest dose was 200 mg/day (6.6 % of patients), and the highest dose was 400 mg/day (35 % of patients).
3.1.4 Concomitant Medications
Many of the patients were taking concomitant non-target pain medications, either prescribed, purchased over-the-counter (OTC), or both prescribed and OTC. The use of these other pain medications was broadly similar across the three target medication groups (Table 2).
Nearly 30 % of patients taking one target medication also took prescribed paracetamol. Nearly one-fifth took OTC paracetamol, and 8.4 % took both prescribed and OTC paracetamol. Although co-codamol contains paracetamol, 21.4 % of patients in the co-codamol group were prescribed additional paracetamol, and 17.7 % bought paracetamol OTC. Nearly 1 in 12 patients taking co-codamol were taking prescribed and OTC paracetamol in addition to their co-codamol.
The total number of oral medications taken (for pain and other conditions), in addition to the target medication, are shown in Table A of the ESM. The proportions of patients were fairly similar across the groups, except the ‘10 or more’ oral medications category, which accounted for a considerably higher percentage of the tramadol group than the TDB or co-codamol groups.
3.2 Patient Satisfaction
At baseline, nearly 80 % of patients in the TDB group reported being either ‘very satisfied’ or ‘satisfied’ with their medication, compared with fewer than 40 % of patients in both the co-codamol and tramadol groups (Fig. 2); this difference was statistically significant. When adjusted for age and sex, the estimated treatment effect for TDB vs. co-codamol was 3.56 (95 % CI 1.90–6.68; p < 0.0001). For TDB vs. tramadol, the estimated treatment effect was 3.22 (95 % CI 1.67–6.20; p = 0.0005).
Patient satisfaction with their current pain medication. Measured at baseline in patients taking one target medication (TDB, n = 85; co-codamol, n = 373; tramadol, n = 243). ‘Other’ includes ‘Neither satisfied nor dissatisfied’, ‘Dissatisfied’, ‘Very dissatisfied’ and ‘No opinion’. TDB transdermal buprenorphine
3.3 HRQL
The SF-36 Physical Component Summary and Mental Component Summary scores for each group at baseline are shown in Table 3. The mean Physical Component Summary score was higher in the TDB group (38.39) than in both the co-codamol (30.99) and tramadol (27.83) groups. In the age- and sex-adjusted analysis, this difference was statistically significant for the TDB group when compared with the tramadol group (p < 0.0001), but not when compared with the co-codamol group (p = 0.0910). No significant differences in the Mental Component Summary scores were observed between the groups. The scores from the follow-up questionnaires from months 1, 2 and 3 are shown in Table 4. The Physical Component Summary results were broadly similar to baseline after 1 month, but after 2 and 3 months the treatment differences were smaller. For the Mental Component Summary scores, all of the follow-up results showed that mean scores were numerically higher in patients taking co-codamol and tramadol than those taking TDB, but that these differences were not significant.
3.4 Adherence
The mean MMAS score in the TDB group at baseline was 6.01, which corresponds to ‘medium adherence’. Mean results for the co-codamol and tramadol groups were 5.24 and 5.73, respectively, putting both groups in the ‘low adherence’ category. The mean MMAS score in the TDB group was significantly higher than the mean scores for both the co-codamol and tramadol groups. The adjusted analysis showed that the estimated treatment effect for TDB vs. co-codamol was 1.07 (95 % CI 0.57–1.56; p < 0.0001), and 0.54 (95 % CI 0.02–1.07; p = 0.0435) for TDB vs. tramadol.
Looking at the trends in individual scores at baseline, there were more patients in the TDB group with high and medium adherence, and fewer patients with low adherence, compared with the co-codamol and tramadol groups (Fig. 3). Results for each question are shown in Table B of the ESM.
Patient adherence with their pain medication. Percentages of patients in each target medication group with high, medium and low adherence, according to the Morisky Medication Adherence Scale. N = 701 patients taking one target medication: TDB, n = 85; co-codamol, n = 373; tramadol, n = 243. TDB transdermal buprenorphine
After 1 month, adherence results were broadly similar to those recorded at baseline, with mean MMAS total scores of 6.33 for TDB, 5.45 for co-codamol, and 5.61 for tramadol. More patients in the TDB group were classed as having high and medium adherence, and fewer patients had low adherence, than in the co-codamol and tramadol groups. However, at months 2 and 3, there were very few differences between the groups.
3.5 Reasons for Discontinuation
Reasons for discontinuation at months 1, 2 and 3 for the full analysis population are shown in Table C of the ESM. Although the numbers of patients who recorded reasons for discontinuation were small, discontinuations due to side effects were more common in the co-codamol and tramadol groups than in the TDB group.
3.6 Adverse Events
AEs were reported by 30.6 % of patients in the TDB group, compared with 53.4 % in the co-codamol group and 55.1 % in the tramadol group (Table D of the ESM). The incidence of constipation was much higher in the co-codamol group (23.9 %) than in the TDB group (9.4 %) or tramadol group (10.3 %); dizziness occurred in more patients in the tramadol group (10.7 %) than the TDB group (5.9 %) or co-codamol group (6.7 %); somnolence was reported in only 1.2 % of patients in the TDB group compared with 11.3 % in the co-codamol group and 14.8 % in the tramadol group; and psychiatric disorders were reported in more patients in the tramadol group (11.1 %) than the TDB group (1.2 %) or the co-codamol group (4.6 %).
4 Discussion
We believe this is the first study comparing patient-reported outcomes for medication satisfaction, HRQL and treatment adherence between different opioid analgesics in the treatment of OA pain. Previous studies have demonstrated comparable analgesia between TDB and co-codamol and tramadol [18, 19]. The intention was to highlight the other potential benefits of using a patch besides pain relief that may be important to patients, such as satisfaction with their medication or improvements in HRQL. TDB has the convenience of once-weekly administration and reduces the overall pill burden [18], which may be particularly important for patients with concomitant conditions who are taking multiple medications. Patients in the current study with additional medical conditions may have already been taking a number of non-analgesic medicines every day. The additional conditions most commonly reported in this study were depression, high blood pressure, high cholesterol and type II diabetes, which are all likely to require long-term medication use. Analgesic patches provide continuous pain relief without the risk of peaks and troughs of dosing that might be seen when taking regular oral analgesics. The patches may be useful for patients who are unable to take oral medications or have difficulty swallowing.
This study indicates that patients prescribed TDB for self-reported OA pain are more satisfied with their medication compared with patients taking co-codamol or tramadol. It would seem logical that increased patient satisfaction with pain medication might improve treatment adherence, and consequently patient outcomes, but there have been few studies looking at this for pain. Hirsh et al. [22] suggested a link between patient satisfaction and compliance with treatment in patients with chronic pain. However, a recent study showed that adherence and treatment satisfaction were not linked to quality-of-life outcomes in patients with chronic pain [23]. In our study, patients in the TDB group reported both greater treatment satisfaction and higher Physical Component Summary SF-36 scores compared with the co-codamol and tramadol groups. At baseline, the difference in Physical Component Summary SF-36 scores in the TDB group was statistically significant compared with tramadol, and scores were numerically higher compared with co-codamol.
Quality of life is an important consideration in the treatment of chronic pain patients. All aspects of quality of life are compromised when pain is inadequately treated, and effective pain relief has been shown to improve HRQL [24]. When patients with chronic pain were asked to rank aspects of quality of life impacted by their condition, they highlighted enjoyment of life, fatigue, emotional wellbeing and physical activities as the most important areas they would consider when evaluating the success of their pain treatment [25]. Our study indicates that SF-36 Physical Component Summary HRQL scores are higher for patients prescribed TDB compared with co-codamol or tramadol. After adjusting for age and sex, the treatment difference in SF-36 Physical Component Summary score between the TDB and co-codamol groups was 1.75, which was not statistically significant (p .0910); however, the difference between the TDB and tramadol groups was 4.29. As well as being statistically significant (p < 0.0001), this is also likely to be clinically relevant. For patients with OA of the lower extremities, the minimal clinically important difference (MCID) for SF-36 scores has been reported as ranging from 2.0 to 7.8 depending on the subscale used; for the Physical Component Summary, 2.0 was suggested as the MCID to show improvement [26]. In the current study, after 1 month the SF-36 Physical Component Summary scores were broadly similar to baseline, with smaller treatment differences after 2 and 3 months. However, the number of patients in the TDB group completing questionnaires at months 2 and 3 was too low for any conclusions to be drawn from these data. In all three of the follow-up questionnaires, SF-36 Mental Component Summary scores were better for patients taking co-codamol or tramadol than for patients taking TDB; however, these differences were not significant. Over one-third of patients in the study reported depression as a comorbidity. This was not unexpected as depression is very common in people with chronic pain, and it is therefore important for pain to be treated using a biopsychosocial model [27]. It is possible that the high level of depression reported in the study population affected the SF-36 Mental Component Summary scores and may have contributed to the lack of differences seen in these scores between the groups.
Adherence is difficult to measure in clinical studies because of increased monitoring, and possibly increased awareness, by patients that their adherence is being measured. Real-world studies may be more useful for measuring adherence but often (as in this study) rely on patients accurately recalling and reporting their medication use behaviour. The results of this study suggest that patients in the TDB group show medium adherence to their medicine compared with low adherence in the co-codamol and tramadol groups. To qualify for high adherence, a patient would need a perfect score on the MMAS questionnaire. For example, this means they must never forget a dose or forget to take their medicine with them when travelling. When considering patch medications, some of the questions may be misleading; for example, asking if there were any days in the last week when the medication was not taken, or if the medication was taken yesterday. Patients could misinterpret these questions as asking whether they had applied a patch on the days in question, when in reality they would be ‘taking’ their medication on any of the 7 days after patch application. Many patients with OA are likely to be prescribed a number of different medications, both for pain and other comorbid conditions; however, increasing numbers of concomitant medications have been linked with a decrease in medication adherence [28]. This is an increasing problem, particularly in older people. A recent review of Scottish medical records found that in 2010, 17.2 % of people over 65 years of age were prescribed 10 medications in an 84-day period [29]. In our study, most of the patients (just over one-third) were taking between three and five additional oral medications, with 8.7 % of the overall study population and 21.0 % of patients in the tramadol group taking over 10 additional oral medications. Once-weekly transdermal patches are likely to be easier for patients to remember to use than oral medications, which could help to explain the improved adherence seen with TDB compared with co-codamol and tramadol in this study. Importantly, patients in the TDB group were younger than those in the co-codamol and tramadol groups, which may also have contributed to the improved compliance. The convenience of a medicine is likely to be important for people who are working, and oral medication may be less convenient than a transdermal patch. For example, a patient who has been prescribed tablets may forget to take their medicine to work with them, it could be inconvenient to stop work to administer their dose, or the patient might forget to take their tablets at the right time while working. In this study, the patient population in the TDB group was predominantly of working age, and the potential convenience benefits of a patch formulation could account for the increased adherence seen in the TDB group. Although the follow-up results were similar after 1 month, there were few differences between the groups after 2 and 3 months. Again, the number of TDB patients completing questionnaires at months 2 and 3 was too low for any conclusions to be drawn.
People with OA pain often take a combination of different analgesic medications [4]. In the current study, patients were divided into groups depending on the target medication they were taking (TDB, co-codamol or tramadol), but 265 patients were taking two or more of the target medications and were removed from the medication-specific analyses. Many patients were also taking concomitant non-target pain medications. However, use of these other pain medications was broadly similar across the three target medication groups, allowing comparisons to be made between the groups. A substantial proportion of patients were taking prescribed and/or OTC paracetamol in addition to the target medication, even for patients already receiving paracetamol from co-codamol. It is important to consider the risk of toxicity in these patients taking high doses of paracetamol. A recent review has suggested that paracetamol may be linked to cardiovascular, gastrointestinal and renal side effects, even at standard therapeutic doses [30]. In addition, high use of paracetamol may indicate that the intensity of patients’ pain and recommended treatment guidelines are not being taken into account in the management of OA pain [31]. Higher proportions of patients in the TDB group were using concomitant analgesics (including prescribed, OTC, and prescribed/OTC) compared with the co-codamol and tramadol groups. It is possible this could have contributed to the improved satisfaction, SF-36 Physical Component Summary HRQL, and adherence scores in the TDB group. It is likely that many patients in this study were self-administering their OTC pain medications without notifying their GP. Physicians should consider this and ask about OTC medication use at each consultation to ensure prescribed analgesia is suitable for the patient’s level of pain, and to reduce the need for the patient to make unnecessary pharmacy visits. Regular pain assessments would also be beneficial, ensuring pain is being treated appropriately in each patient.
AEs reported in this study were typical of those seen with opioid medications. The proportion of patients experiencing AEs was smaller in the TDB group than in the co-codamol or tramadol groups. Constipation was more common in the co-codamol group than the TDB and tramadol groups, and is a well-known side effect of codeine, which has been described as “too constipating for long-term use” [21]. Constipation can have a large impact on patients’ quality of life. In a survey of patients taking opioids and laxatives, it was shown that constipation was the ‘most bothersome’ gastrointestinal side effect of opioids [32] and does not decrease over time as with other opioid side effects. Nervous system disorders and psychiatric disorders occurred more often in the tramadol group than the TDB or co-codamol groups. This included dizziness, which can be a particular problem in the elderly, and is present in some form in 30 % of people over 65 years of age, and 50 % of people aged 85 years and over. Almost 60 % of older primary care patients with dizziness experience a moderate or severe impact on their daily life as a result [33]. Dizziness has been linked to anxiety and avoidance behaviour, such as avoiding crowds and being away from home, and can also cause occupational problems in people of working age [34].
The high dropout rate over the study period was mostly due to patients not completing the follow-up questionnaires, rather than discontinuation of treatment. This highlights the difficulties in carrying out this type of research in patients without healthcare professional input. Because of the drop in patient numbers, the main statistics in this study have been taken from the baseline population. However, the results are still a valid measure of patients’ opinions and treatment outcomes as most of the patients had been stabilised on their medication for 6 months or more, and were not new patients. We did not expect so many long-term patients when we designed the study, and thought that the follow-up questionnaires would show differences, for example as patients changed treatments due to side effects or lack of efficacy. In reality, even if patient numbers had been higher at follow-up, we would have been unlikely to see much difference from baseline in a population largely well-established on their target medication.
As this study had no healthcare professional involvement, some of the information collected may not be as accurate as in a controlled clinical trial, where source data are verified. For example, the self-reported diagnosis of OA was not medically confirmed. However, self-reported OA has recently been shown to have high specificity when compared with a radiographic diagnosis of OA [35]. Patients’ recall of information such as current and recent medications and concomitant conditions may be unreliable. In addition, as this was a non-randomised, non-blinded study, factors that may have influenced the type of analgesic each patient was prescribed may have had an effect on their responses to questions. The treatment groups in the study were unequal, with the co-codamol group over four times larger than the TDB group, although this may reflect the proportion of OA patients taking each medication in the wider population. The TDB group was noticeably younger than the other groups analysed in this study, and younger than the average ages in most OA studies. This could be due to the use of social media and online advertising for patient recruitment, which may have led to selection bias, favouring younger and more IT-literate patients; however, this would have affected all groups equally. It is also possible that healthcare professionals prefer to prescribe TDB for younger patients of working age because it is less intrusive on their daily schedule as it does not require regular administration throughout the day. The TDB group was quite different to the other groups in terms of gender balance, with a much higher proportion of male subjects. It is not clear why there was this gender recruitment difference, as, for example, IT literacy would not be expected to be different by gender. It is possible that GPs were more cautious about using oral opioids in younger males [36], although we have no supporting data. Although an age- and sex-adjusted analysis was performed, the differences in patient numbers and demographics between the groups should be taken into account when interpreting the results of this study. In addition, due to the drop in patient numbers after the baseline questionnaire, it is difficult to interpret the significance of any trends seen in the follow-up results.
5 Conclusions
Although there were between-group differences in patient demographics, this observational study showed that patients prescribed TDB for their hip and/or knee OA pain had higher scores for medication satisfaction, SF-36 Physical Component Summary HRQL measures, and medication adherence than those taking co-codamol or tramadol, two commonly-used oral opioids.
References
Arthritis Research UK. Data and statistics on osteoarthritis. http://www.arthritisresearchuk.org/arthritis-information/data-and-statistics/data-by-condition/osteoarthritis.aspx. Accessed 18 Dec 2015.
Zhang Y, Jordan JM. Epidemiology of osteoarthritis. Clin Geriatr Med. 2010;26:355–69.
Conaghan PG, Porcheret M, Kingsbury SR, Gammon A, Soni A, Hurley M, et al. Impact and therapy of osteoarthritis: the Arthritis Care OA Nation 2012 survey. Clin Rheumatol. 2015;34:1581–8.
National Institute for Health and Care Excellence (NICE). Osteoarthritis. Care and management in adults. February 2014. NICE clinical guideline 177. https://www.nice.org.uk/guidance/cg177. Accessed 18 Dec 2015.
Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012;64:465–74.
American Academy of Orthopaedic Surgeons (AAOS). Treatment of osteoarthritis of the knee. Evidence-based guideline. 2nd ed. May 2013. http://www.aaos.org/Research/guidelines/TreatmentofOsteoarthritisoftheKneeGuideline.pdf. Accessed 18 Dec 2015.
Kress HG. Clinical update on the pharmacology, efficacy and safety of transdermal buprenorphine. Eur J Pain. 2009;13:219–30.
Pergolizzi J, Aloisi AM, Dahan A, Filitz J, Langford R, Likar R, et al. Current knowledge of buprenorphine and its unique pharmacological profile. Pain Pract. 2010;10:428–50.
Guetti C, Angeletti C, Marinangeli F, Ciccozzi A, Baldaschin G, Paladini A, et al. Transdermal buprenorphine for central neuropathic pain: clinical reports. Pain Pract. 2011;11:446–52.
Plosker GL, Lyseng-Williamson KA. Buprenorphine 5, 10 and 20 µg/h transdermal patch: a guide to its use in chronic non-malignant pain. CNS Drugs. 2012;26:367–73.
Aurilio C, Ceccarelli I, Pota V, Sansone P, Massafra C, Barbarisi M, et al. Endocrine and behavioural effects of transdermal buprenorphine in pain-suffering women of different reproductive ages. Endocr J. 2011;58:1071–8.
Al-Tawil N, Odar-Cederlöf I, Berggren AC, Johnson HE, Persson J. Pharmacokinetics of transdermal buprenorphine patch in the elderly. Eur J Clin Pharmacol. 2013;69:143–9.
Karlsson J, Söderström A, Augustini BG, Berggren AC. Is buprenorphine transdermal patch equally safe and effective in younger and elderly patients with osteoarthritis-related pain? Results of an age-group controlled study. Curr Med Res Opin. 2014;30:575–87.
Gianni W, Madaio AR, Ceci M, Benincasa E, Conati G, Franchi F, et al. Transdermal buprenorphine for the treatment of chronic noncancer pain in the oldest old. J Pain Symptom Manage. 2011;41:707–14.
Likar R, Vadlau EM, Breschan C, Kager I, Korak-Leiter M, Ziervogel G. Comparable analgesic efficacy of transdermal buprenorphine in patients over and under 65 years of age. Clin J Pain. 2008;24:536–43.
Niscola P, Scaramucci L, Vischini G, Giovannini M, Ferrannini M, Massa P, et al. The use of major analgesics in patients with renal dysfunction. Curr Drug Targets. 2010;11:752–8.
James IG, O’Brien CM, McDonald CJ. A randomized, double-blind, double-dummy comparison of the efficacy and tolerability of low-dose transdermal buprenorphine (BuTrans seven-day patches) with buprenorphine sublingual tablets (Temgesic) in patients with osteoarthritis pain. J Pain Symptom Manage. 2010;40:266–78.
Conaghan PG, O’Brien CM, Wilson M, Schofield JP. Transdermal buprenorphine plus oral paracetamol vs an oral codeine-paracetamol combination for osteoarthritis of hip and/or knee: a randomised trial. Osteoarthritis Cartil. 2011;19:930–8.
Karlsson M, Berggren A-C. Efficacy and safety of low-dose transdermal buprenorphine patches (5, 10, and 20 microg/h) versus prolonged-release tramadol tablets (75, 100, 150, and 200 mg) in patients with chronic osteoarthritis pain: a 12-week, randomized, open-label, controlled, parallel-group noninferiority study. Clin Ther. 2009;31:503–13.
Gallagher AM, Leighton-Scott J, van Staa TP. Utilization characteristics and treatment persistence in patients prescribed low-dose buprenorphine patches in primary care in the United Kingdom: a retrospective cohort study. Clin Ther. 2009;31:1707–15.
British Medical Association and Royal Pharmaceutical Society of Great Britain. British National Formulary. Vol. 69. BNF Publications; Mar 2015.
Hirsh AT, Atchison JW, Berger JJ, Waxenberg LB, Lafayette-Lucey A, Bulcourf BB, et al. Patient satisfaction with treatment for chronic pain: predictors and relationship to compliance. Clin J Pain. 2005;21:302–10.
Wong WS, Chow YF, Chen PP, Wong S, Fielding R. A longitudinal analysis on pain treatment satisfaction among Chinese patients with chronic pain: predictors and association with medical adherence, disability, and quality of life. Qual Life Res. 2015;24:2087–97.
Katz N. The impact of pain management on quality of life. J Pain Symptom Manage. 2002;24:S38–47.
Turk DC, Dworkin RH, Revicki D, Harding G, Burke LB, Cella D, et al. Identifying important outcome domains for chronic pain clinical trials: an IMMPACT survey of people with pain. Pain. 2008;137:276–85.
Angst F, Aeschlimann A, Steiner W, Stucki G. Responsiveness of the WOMAC osteoarthritis index as compared with the SF-36 in patients with osteoarthritis of the legs undergoing a comprehensive rehabilitation intervention. Ann Rheum Dis. 2001;60:834–40.
Manchikanti L, Fellows B, Singh V. Understanding psychological aspects of chronic pain in interventional pain management. Pain Physician. 2002;5:57–82.
Markotic F, Cerni Obrdalj E, Zalihic A, Pehar R, Hadziosmanovic Z, Pivic G, et al. Adherence to pharmacological treatment of chronic nonmalignant pain in individuals aged 65 and older. Pain Med. 2013;14:247–56.
Guthrie B, Makubate B, Hernandez-Santiago V, Dreischulte T. The rising tide of polypharmacy and drug–drug interactions: population database analysis 1995–2010. BMC Med. 2015;13:74.
Roberts E, Delgado Nunes V, Buckner S, Latchem S, Constanti M, Miller P, et al. Paracetamol: not as safe as we thought? A systematic literature review of observational studies. Ann Rheum Dis. 2016;75(3):552–9.
Conaghan PG, Peloso PM, Everett SV, Rajagopalan S, Black CM, Mavros P, et al. Inadequate pain relief and large functional loss among patients with knee osteoarthritis: evidence from a prospective multinational longitudinal study of osteoarthritis real-world therapies. Rheumatology (Oxford). 2015;54:270–7.
Bell TJ, Panchal SJ, Miaskowski C, Bolge SC, Milanova T, Williamson R. The prevalence, severity, and impact of opioid-induced bowel dysfunction: results of a US and European Patient Survey (PROBE 1). Pain Med. 2009;10:35–42.
Dros J, Maarsingh OR, Beem L, van der Horst HE, ter Riet G, Schellevis FG, et al. Impact of dizziness on everyday life in older primary care patients: a cross-sectional study. Health Qual Life Outcomes. 2011;9:44.
Yardley L, Owen N, Nazareth I, Luxon L. Prevalence and presentation of dizziness in a general practice community sample of working age people. Br J Gen Pract. 1998;48:1131–5.
Parsons C, Clynes M, Syddall H, Jagannath D, Litwic A, van der Pas S, et al. How well do radiographic, clinical and self-reported diagnoses of knee osteoarthritis agree? Findings from the Hertfordshire cohort study. SpringerPlus. 2015;4:177.
Stanos SP, Bruckenthal P, Barkin RL. Strategies to reduce the tampering and subsequent abuse of long-acting opioids: potential risks and benefits of formulations with physical or pharmacologic deterrents to tampering. Mayo Clin Proc. 2012;87:683–94.
Acknowledgments
The authors would like to thank all of the study participants. Statistical assistance was provided by Suzanne Lloyd, Robertson Centre for Biostatistics, University of Glasgow, UK. Medical writing assistance was provided by Fiona Millard, Vivid Iris Limited, Cambridge, UK.
Author contributions
Philip G. Conaghan, Michael Serpell, Rod Junor and Sara Dickerson were involved in study design, analysis and interpretation of data; Paula McSkimming provided statistical analysis and interpretation of data. All authors provided critical revision of the manuscript for important intellectual content, and approved the submitted manuscript and subsequent revisions. As corresponding author, Sara Dickerson acts as the overall guarantor of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Study documents were reviewed and approved by the EoSRES, and all patients participating in the study were asked to provide informed consent by telephone or online. All procedures performed in studies involving human participants were in accordance with the ethical standards of the appointed Research Ethics Committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding
This study, including medical writing support and open access, was funded by NAPP Pharmaceuticals Limited.
Potential conflict of interest
Philip G. Conaghan declares no conflicts of interest. Michael Serpell has received research support, consulting fees or honoraria in the past 3 years from Astellas, Grünenthal, Lilly, Napp and Pfizer. Paula McSkimming is an employee of The Robertson Centre for Biostatistics, which received funding for the analysis and reporting of this study. Rod Junor and Sara Dickerson were employees of Napp Pharmaceuticals Limited at the time of the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
40271_2016_181_MOESM2_ESM.pdf
Model Results. Model results from the age- and sex-adjusted analyses for medication satisfaction scores, aggregate physical scores and aggregate mental scores for SF-36, and MMAS scores
40271_2016_181_MOESM3_ESM.pdf
Additional Tables. Table A: Number of oral medications taken in addition to the target medication. Table B: Adherence results for each question of the Morisky Medication Adherence Scale. Table C: Reasons for discontinuation. Table D: Adverse events reported
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Conaghan, P.G., Serpell, M., McSkimming, P. et al. Satisfaction, Adherence and Health-Related Quality of Life with Transdermal Buprenorphine Compared with Oral Opioid Medications in the Usual Care of Osteoarthritis Pain. Patient 9, 359–371 (2016). https://doi.org/10.1007/s40271-016-0181-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40271-016-0181-0