Abstract
Background/Objective
While several psychotropic and cardiovascular drugs have been identified as fall-risk-increasing drugs (FRIDs) in older adults, the intervening mechanisms linking FRIDs and falls are unclear. It is plausible that gait performance is an intermediate variable on the causal pathway between FRIDs and falls. The current evidence on the relationship between medication use and gait performance in older adults is scarce. We aimed to assess the association between FRIDs and gait performance in community-dwelling older adults.
Methods
This was a cross-sectional analysis using data from the Gait and Brain Study, a study of community-dwelling older adults aged 65 years old and over (N = 345). The following drug classes were assessed: antidepressants, benzodiazepines, alpha-blockers, beta-blockers, vasodilators, diuretics, statins and aspirin. Medication use was ascertained through validated questionnaires and electronic medical records. Multiple linear regression models were used to assess the association between each of the drug classes and gait speed and gait variability. Gait variability was expressed as the coefficient of variation (CV = mean/standard deviation) of stride time. Models were adjusted for age, sex, education, body mass index (BMI), mini-mental status exam (MMSE) score, Geriatric Depression Scale (GDS) score, general activity level, use of other FRIDs and comorbidity propensity score.
Results
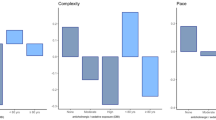
Diuretic use was associated with significantly reduced gait speed (B = −7.97 cm/s, 95% CI: −13.94, −2.00, P = 0.009). Statin use was associated with significantly increased stride time CV (B = 0.13, 95% CI: 0.02, 0.24, P = 0.026). Other drugs did not have a statistically significant relationship with gait speed or variability.
Conclusion
The association between diuretic use and reduced gait speed is consistent with existing evidence on diuretic use and increased fall risk. The association between statins and increased stride time variability is notable given inconclusive evidence in previous studies. Our results provide initial estimates of the association between FRIDs and gait performance in older adults for future longitudinal studies.
Similar content being viewed by others
References
World Health Organization, 2018. Fact sheet on falls. https://www.who.int/news-room/fact-sheets/detail/falls. Updated 16 Jan 2018. Accessed 27 Jan 2020.
Public Health Agency of Canada, 2014. Seniors’ falls in Canada: second report. https://www.phac-aspc.gc.ca/seniors-aines/publications/public/injury-blessure/seniors_falls-chutes_aines/assets/pdf/seniors_falls-chutes_aines-eng.pdf. Accessed 27 Jan 2020.
Somadder M, Mondal S, Kersh R, Abdelhafiz AH. Are recurrent fallers depressed? J Am Geriatr Soc (United States). 2007. https://doi.org/10.1111/j.1532-5415.2007.01449.x.
Painter JA, Allison L, Dhingra P, Daughtery J, Cogdill K, Trujillo LG. Fear of falling and its relationship with anxiety, depression, and activity engagement among community-dwelling older adults. Am J Occup Ther. 2012;66:169–76. https://doi.org/10.5014/ajot.2012.002535.
Bloch F, Blandin M, Ranerison R, Claessens YE, Rigaud AS, Kemoun G. Anxiety after a fall in elderly subjects and subsequent risk of developing post traumatic stress disorder at two months. A pilot study. J Nutr Health Aging. 2014;18:303–6. https://doi.org/10.1007/s12603-013-0415-y.
Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 2009;169:1952–60. https://doi.org/10.1001/archinternmed.2009.357.
Seppala LJ, Wermelink AMAT, de Vries M, Ploegmakers KJ, van de Glind EMM, Daams JG, et al. Fall-risk-increasing drugs: a systematic review and meta-analysis: II. Psychotropics. J Am Med Dir Assoc. 2018;19:371.e11-371.e17. https://doi.org/10.1016/j.jamda.2017.12.098.
de Vries M, Seppala LJ, Daams JG, van de Glind EMM, Masud T, van der Velde N, et al. Fall-risk-increasing drugs: a systematic review and meta-analysis: I. Cardiovascular drugs. J Am Med Dir Assoc. 2018;19:371.e1–371.e9. https://doi.org/10.1016/j.jamda.2017.12.013.
American Geriatrics Society 2019 Updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67:674–94. https://doi.org/10.1111/jgs.15767.
Verghese J, Holtzer R, Lipton RB, Wang C. Quantitative gait markers and incident fall risk in older adults. J Gerontol A Biol Sci Med Sci. 2009;64:896–901.
Middleton A, Fritz SL, Lusardi M. Walking speed: the functional vital sign. J Aging Phys Act. 2015;23:314–22.
Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil. 2001;82:1050–6. https://doi.org/10.1053/apmr.2001.24893.
Montero-Odasso M, Muir SW, Hall M, Doherty TJ, Kloseck M, Beauchet O, et al. Gait variability is associated with frailty in community-dwelling older adults. J Gerontol Ser A. 2011;66A:568–76. https://doi.org/10.1093/gerona/glr007.
Hilmer SN, Mager DE, Simonsick EM, Ling SM, Windham BG, Harris TB, et al. Drug burden index score and functional decline in older people. Am J Med. 2009;122:1142–9.
Taipale HT, Bell JS, Gnjidic D, Sulkava R, Hartikainen S. Sedative load among community-dwelling people aged 75 years or older: association with balance and mobility. J Clin Psychopharmacol. 2012;32:218–24. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed13&NEWS=N&AN=364384488.
Lim R, Kalisch Ellett LM, Widagdo IS, Pratt NL, Roughead EE. Analysis of anticholinergic and sedative medicine effects on physical function, cognitive function, appetite and frailty: a cross-sectional study in Australia. BMJ Open. 2019;9:e029221. http://bmjopen.bmj.com/content/early/by/section.
National Library of Medicine. Gait as predictor of dementia and falls. The gait and brain cohort study. In: ClinicalTrials.gov. National Library of Medicine. 2023. https://clinicaltrials.gov/ct2/show/NCT03020381. Accessed 09 May 2023.
Montero-Odasso M, Bergman H, Phillips NA, Wong CH, Sourial N, Chertkow H. Dual-tasking and gait in people with mild cognitive impairment, the effect of working memory. BMC Geriatr. 2009;9:1–8.
Bilney B, Morris M, Webster K. Concurrent related validity of the GAITRite® walkway system for quantification of the spatial and temporal parameters of gait. Gait Posture 2003;17:68–74. https://www.sciencedirect.com/science/article/pii/S096663620200053X.
Osman A, Kamkar N, Speechley M, Ali S, Montero-Odasso M. Fall risk-increasing drugs and gait performance in community-dwelling older adults: a systematic review. Ageing Res Rev. 2022;77:101599. https://www.sciencedirect.com/science/article/pii/S1568163722000411.
Aronson JK, Bankhead C, Mahtani KR, Nunan D. Catalogue of bias collaboration, confounding by indication. In: Catalogue of biases. 2018. https://catalogofbias.org/biases/confounding-by-indication.
Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127:757–63. https://doi.org/10.7326/0003-4819-127-8_Part_2-199710151-00064.
Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Stürmer T. Variable selection for propensity score models. Am J Epidemiol. 2006;163:1149–56. https://pubmed.ncbi.nlm.nih.gov/16624967.
Tachi T, Yokoi T, Goto C, Umeda M, Noguchi Y, Yasuda M, et al. Hyponatremia and hypokalemia as risk factors for falls. Eur J Clin Nutr. 2015;69:205–10.
Gray SL, Aragaki AK, LaMonte MJ, Cochrane BB, Kooperberg C, Robinson JG, et al. Statins, angiotensin-converting enzyme inhibitors, and physical performance in older women. J Am Geriatr Soc. 2012;60:2206–14. https://doi.org/10.1111/jgs.12029.
Lo-Ciganic W-H, Perera S, Gray SL, Boudreau RM, Zgibor JC, Strotmeyer ES, et al. Statin use and decline in gait speed in community-dwelling older adults. J Am Geriatr Soc. 2015;63:124–9. https://doi.org/10.1111/jgs.13134.
Kawai H, Ihara K, Kera T, Hirano H, Fujiwara Y, Tanaka M, et al. Association between statin use and physical function among community-dwelling older Japanese adults. Geriatr Gerontol Int. 2018;18:623–30. https://doi.org/10.1111/ggi.13228.
Dumurgier J, Singh-Manoux A, Tavernier B, Tzourio C, Elbaz A. Lipid-lowering drugs associated with slower motor decline in the elderly adults. J Gerontol Ser A. 2014;69A:199–206. https://doi.org/10.1093/gerona/glt140.
Haerer W, Delbaere K, Bartlett H, Lord SR, Rowland J. Relationships between HMG-CoA reductase inhibitors (statin) use and strength, balance and falls in older people. Intern Med J. 2012;42:1329–34. https://doi.org/10.1111/j.1445-5994.2011.02622.x.
Parker BA, Thompson PD. Effect of statins on skeletal muscle: exercise, myopathy, and muscle outcomes. Exerc Sport Sci Rev. 2012;40. https://journals.lww.com/acsm-essr/Fulltext/2012/10000/Effect_of_Statins_on_Skeletal_Muscle__Exercise,.2.aspx.
Figgins E, Pieruccini-Faria F, Speechley M, Montero-Odasso M. Potentially modifiable risk factors for slow gait in community-dwelling older adults: a systematic review. Ageing Res Rev. 2021;66:101253. https://www.sciencedirect.com/science/article/pii/S1568163720303883.
Cullen S, Montero-Odasso M, Bherer L, Almeida Q, Fraser S, Muir-Hunter S, et al. Guidelines for gait assessments in the Canadian Consortium on Neurodegeneration in Aging (CCNA). Can Geriatr J. 2018;21:157–65.
Cesari M, Pedone C, Incalzi RA, Pahor M. ACE-inhibition and physical function: results from the trial of angiotensin-converting enzyme inhibition and novel cardiovascular risk factors (TRAIN) study. J Am Med Dir Assoc. 2010;11:26–32. https://pubmed.ncbi.nlm.nih.gov/20129212.
George CJ, Verghese J. Gait performance in hypertensive patients on angiotensin-converting enzyme inhibitors. J Am Med Dir Assoc. 2016;17:737–40. https://doi.org/10.1016/j.jamda.2016.03.022.
Deguchi M, Ooi K, Nishida K, Enokiya T. Risk factor analysis of the decrease in gait speed among Japanese older outpatients with polypharmacy. J Pharm Heal Care Sci. 2019;5:23. http://www.jphcs.net/.
Hausdorff JM, Herman T, Baltadjieva R, Gurevich T, Giladi N. Balance and gait in older adults with systemic hypertension. Am J Cardiol. 2003;91:643–5. https://doi.org/10.1016/S0002-9149(02)03332-5.
Rosano C, Longstreth Jr WT, Boudreau R, Taylor CA, Du Y, Kuller LH, et al. High blood pressure accelerates gait slowing in well-functioning older adults over 18-years of follow-up. J Am Geriatr Soc. 2011;59:390–7. https://doi.org/10.1111/j.1532-5415.2010.03282.x.
Aisen PS, Deluca T, Lawlor BA. Falls among geropsychiatry inpatients are associated with PRN medications for agitation. Int J Geriatr Psychiatry. 1992;7:709–12.
Bulat T, Castle SC, Rutledge M, Quigley P. Clinical practice algorithms: medication management to reduce fall risk in the elderly – part 3, benzodiazepines, cardiovascular agents, and antidepressants. J Am Acad Nurse Pract. 2008;20:55–62. https://doi.org/10.1111/j.1745-7599.2007.00285.x.
Poujol L, Annweiler C, Allali G, Fantino B, Beauchet O. Effect of psychoactive medication on gait variability in community-dwelling older adults: a cross-sectional study. J Am Geriatr Soc. 2010;58:1207–8. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med8&NEWS=N&AN=20722862.
Donoghue OA, O’Hare C, King-Kallimanis B, Kenny RA. Antidepressants are independently associated with gait deficits in single and dual task conditions. Am J Geriatr Psychiatry. 2015;23:189–99. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=med12&NEWS=N&AN=24933587.
Peretti S, Judge R, Hindmarch I. Safety and tolerability considerations: tricyclic antidepressants vs. selective serotonin reuptake inhibitors. Acta Psychiatr Scand Suppl. 2000;403:17–25.
Glynn RJ, Schneeweiss S, Stürmer T. Indications for propensity scores and review of their use in pharmacoepidemiology. Basic Clin Pharmacol Toxicol. 2006;98:253–9.
Elze MC, Gregson J, Baber U, Williamson E, Sartori S, Mehran R, et al. Comparison of propensity score methods and covariate adjustment: evaluation in 4 cardiovascular studies. J Am Coll Cardiol. 2017;69:345–57.
Huang AR Mallet L. Medication use and falls in people with cognitive impairment. Assessment and management strategies. In: Montero-Odasso M, Camicioli R, editors. Falls and cognition in older persons: fundamentals, assessment and therapeutic options. Cham: Springer; 2020. pp. 151–164. https://doi.org/10.1007/978-3-030-24233-6_9.
Bourin M, Briley M. Sedation, an unpleasant, undesirable and potentially dangerous side-effect of many psychotropic drugs. Hum Psychopharmacol Clin Exp. 2004;19:135–9. https://doi.org/10.1002/hup.561.
Seppala LJ, Petrovic M, Ryg J, Bahat G, Topinkova E, Szczerbińska K, et al. STOPPFall (Screening Tool of Older Persons Prescriptions in older adults with high fall risk): a Delphi study by the EuGMS Task and Finish Group on Fall-Risk-Increasing Drugs. Age Ageing. 2021;50:1189–99. https://doi.org/10.1093/ageing/afaa249.
Hilmer SN, Mager DE, Simonsick EM, Cao Y, Ling SM, Windham BG, et al. A drug burden index to define the functional burden of medications in older people. Arch Intern Med. 2007;167:781–7. https://doi.org/10.1001/archinte.167.8.781.
Acknowledgements
We would like to acknowledge all the participants who provided data to the Gait and Brain Study. We also would like to acknowledge all the staff and trainees of the Gait and Brain Lab for their work on data collection and data entry. This work first presented in the form of an abstract at the 40th Annual Scientific Meeting of the Canadian Geriatrics in 2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Abdelhady Osman is a recipient of an Ontario Graduate Scholarship (OGS) for the year 2020–2021. Dr. Montero-Odasso’s research program in Gait and Brain Health is supported by grants from the Canadian Institutes of Health Research (CIHR; MOP 211220, PJT 153100), the Ontario Ministry of Research and Innovation (ER11–08–101), the Ontario Neurodegenerative Diseases Research Initiative (OBI 34739), and the Department of Medicine Program of Experimental Medicine Research Award (POEM 768915), the University of Western Ontario. He is the first recipient of the Schulich Clinician-Scientist Award.
Conflicts of interest
The authors declare no conflicts of interest.
Ethics approval
Ethics approval was obtained from the University of Western Ontario Health Sciences Research Ethics Board (REB).
Consent to participate
Written informed consent was obtained from all participants prior to their enrolment in the Gait and Brain Study.
Consent for publication
Not applicable.
Availability of data and material
The datasets generated during and/or analysed in this study cannot be shared, since data sharing was not specified in our REB submission or our letter of consent to participants.
Code availability
The statistical codes used in this analysis are available on reasonable request from the corresponding author and with the permission of all authors.
Author contributions
Conceptualization: AO, MS and MMO. Data acquisition: MMO. Methodology: AO, MS and SA. Formal analysis: AO. Interpretation: All authors. Writing-original draft: AO. Writing-reviewing and editing: All authors. All authors reviewed and approved the final version of the manuscript.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Osman, A., Speechley, M., Ali, S. et al. Fall-Risk-Increasing Drugs and Gait Performance in Community-Dwelling Older Adults: Exploratory Results from the Gait and Brain Study. Drugs Aging 40, 721–730 (2023). https://doi.org/10.1007/s40266-023-01045-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-023-01045-1