Abstract
Background
Low-dose acetylsalicylic acid (aspirin) prevents stroke and myocardial infarction in patients with cardiovascular disease (CVD), but whether it should be used for primary CVD prevention in older Chinese adults remains unclear.
Methods
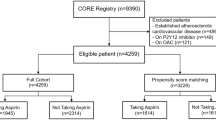
This prospective study investigated Chinese people aged > 70 years participating in the Kadoorie Study of Chronic Disease. The subjects were grouped as aspirin users and nonusers. Propensity score matching (PSM) was used to achieve balanced baseline characteristics. The primary outcome was major adverse cardiac and cerebrovascular events (MACCE). The secondary outcomes were all-cause mortality, cardiovascular and/or cerebrovascular disease (CCVD) mortality, and bleeding events. Survival curves were used to compare the outcomes between groups. Cox regression was used to identify the risk factors for the outcomes.
Results
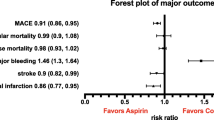
In total, 4791 participants were categorized as aspirin users (n = 257) or nonusers (n = 4534). PSM resulted in 252 and 951 participants in the aspirin user and nonuser groups, respectively. Median follow-up was 8.6 years. Aspirin did not influence MACCE, all-cause mortality, or bleeding events, but it did influence CCVD deaths (p = 0.019). Male sex (hazard ratio [HR] 1.652; 95% confidence interval [CI] 1.217–2.243; p = 0.001), body mass index (BMI) (HR 1.053; 95% CI 1.008–1.100; p = 0.021), and systolic blood pressure (HR 1.009; 95% CI 1.003–1.016; p = 0.004) were independent risk factors for MACCE. Survival analysis showed higher rates of CCVD mortality among aspirin users (HR 1.363; 95% CI 1.040–1.786; p = 0.025), but this was not significant in the regression analysis.
Conclusions
There were no significant benefits from using aspirin as primary prevention for MACCE in older Chinese adults.





Similar content being viewed by others
References
Francula-Zaninovic S, Nola IA. Management of measurable variable cardiovascular disease’ risk factors. Curr Cardiol Rev. 2018;14(3):153–63.
Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: current features and implications. Nat Rev Cardiol. 2019;16(4):203–12.
Antithrombotic Trialists’ (ATT) Collaboration, Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet (London, England). 2009;373(9678):1849–60.
Patscheke H, Hornberger W, Zehender H. Pathophysiological role of thromboxane A2 and pharmacological approaches to its inhibition. Z Kardiol. 1990;79(Suppl 3):151–4.
Catella-Lawson F, Reilly MP, Kapoor SC, Cucchiara AJ, DeMarco S, Tournier B, et al. Cyclooxygenase inhibitors and the antiplatelet effects of aspirin. N Engl J Med. 2001;345(25):1809–17.
Patrono C, Baigent C. Role of aspirin in primary prevention of cardiovascular disease. Nat Rev Cardiol. 2019;16(11):675–86.
Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ (Clin Res Ed). 2002;324(7329):71–86.
Campbell CL, Smyth S, Montalescot G, Steinhubl SR. Aspirin dose for the prevention of cardiovascular disease: a systematic review. JAMA. 2007;297(18):2018–24.
Guirguis-Blake JM, Evans CV, Senger CA, O’Connor EA, Whitlock EP. Aspirin for the primary prevention of cardiovascular events: a systematic evidence review for the U. S. Preventive Services Task Force. Ann Intern Med. 2016;164(12):804–13.
Steering Committee of the Physicians’ Health Study Research Group. Final report on the aspirin component of the ongoing Physicians’ Health Study. N Engl J Med. 1989;321(3):129–35.
Mora S, Manson JE. Aspirin for primary prevention of atherosclerotic cardiovascular disease: advances in diagnosis and treatment. JAMA Intern Med. 2016;176(8):1195–204.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention and Rehabilitation (EACPR). Eur Heart J. 2016;37(29):2315–81.
Gaziano JM, Brotons C, Coppolecchia R, Cricelli C, Darius H, Gorelick PB, et al. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet (London, England). 2018;392(10152):1036–46.
ASCEND Study Collaborative Group, Bowman L, Mafham M, Wallendszus K, Stevens W, Buck G, et al. Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med. 2018;379(16):1529–39.
McNeil JJ, Wolfe R, Woods RL, Tonkin AM, Donnan GA, Nelson MR, et al. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med. 2018;379(16):1509–18.
McNeil JJ, Nelson MR, Woods RL, Lockery JE, Wolfe R, Reid CM, et al. Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med. 2018;379(16):1519–28.
McNeil JJ, Woods RL, Nelson MR, Reid CM, Kirpach B, Wolfe R, et al. Effect of aspirin on disability-free survival in the healthy elderly. N Engl J Med. 2018;379(16):1499–508.
Zhang XF, Attia J, D’Este C, Yu XH, Wu XG. A risk score predicted coronary heart disease and stroke in a Chinese cohort. J Clin Epidemiol. 2005;58(9):951–8.
Frank AT, Zhao B, Jose PO, Azar KM, Fortmann SP, Palaniappan LP. Racial/ethnic differences in dyslipidemia patterns. Circulation. 2014;129(5):570–9.
Fei K, Rodriguez-Lopez JS, Ramos M, Islam N, Trinh-Shevrin C, Yi SS, et al. Racial and ethnic subgroup disparities in hypertension prevalence, New York City Health and Nutrition Examination Survey, 2013–2014. Prev Chronic Dis. 2017;20(14):E33.
Yang X, Li J, Hu D, Chen J, Li Y, Huang J, et al. Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population: The China-PAR Project (Prediction for ASCVD Risk in China). Circulation. 2016;134(19):1430–40.
Li XY, Shi ZW, Zhao D, Yin DW. 2019 Chinese expert consensus statement on aspirin application in primary prevention of cardiovascular disease. Chin Med J. 2020.
Chen Z, Lee L, Chen J, Collins R, Wu F, Guo Y, et al. Cohort profile: the Kadoorie Study of Chronic Disease in China (KSCDC). Int J Epidemiol. 2005;34(6):1243–9.
Li LM, Lv J, Guo Y, Collins R, Chen JS, Peto R, et al. The China Kadoorie Biobank: related methodology and baseline characteristics of the participants. Zhonghua liu xing bing xue za zhi Zhonghua liuxingbingxue zazhi. 2012;33(3):249–55.
Chen Z, Chen J, Collins R, Guo Y, Peto R, Wu F, et al. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int J Epidemiol. 2011;40(6):1652–66.
Lacey B, Lewington S, Clarke R, Kong XL, Chen Y, Guo Y, et al. Age-specific association between blood pressure and vascular and non-vascular chronic diseases in 0.5 million adults in China: a prospective cohort study. Lancet Glob Health. 2018;6(6):e641–9.
Chinese Society of Cardiology of Chinese Medical Association, Cardiovascular Disease Prevention and Rehabilitation Committee of Chinese Association of Rehabilitation Medicine, Cardiovascular Disease Committee of Chinese Association of Gerontology and Geriatrics, Thrombosis Prevention and Treatment Committee of Chinese Medical Doctor Association. Chinese guideline on the primary prevention of cardiovascular diseases. Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48(12):1000–38.
Fan M, Yu C, Guo Y, Bian Z, Li X, Yang L, et al. Effect of total, domain-specific, and intensity-specific physical activity on all-cause and cardiovascular mortality among hypertensive adults in China. J Hypertens. 2018;36(4):793–800.
Stevens W, Peneva D, Li JZ, Liu LZ, Liu G, Gao R, et al. Estimating the future burden of cardiovascular disease and the value of lipid and blood pressure control therapies in China. BMC Health Serv Res. 2016;10(16):175.
Wong ND. Epidemiological studies of CHD and the evolution of preventive cardiology. Nat Rev Cardiol. 2014;11(5):276–89.
Zheng SL, Roddick AJ. Association of aspirin use for primary prevention with cardiovascular events and bleeding events: a systematic review and meta-analysis. JAMA. 2019;321(3):277–87.
Jung M, Lee S. Efficacy of aspirin in the primary prevention of cardiovascular diseases and cancer in the elderly: a population-based cohort study in Korea. Drugs Aging. 2020;37(1):43–55.
Ikeda Y, Shimada K, Teramoto T, Uchiyama S, Yamazaki T, Oikawa S, et al. Low-dose aspirin for primary prevention of cardiovascular events in Japanese patients 60 years or older with atherosclerotic risk factors: a randomized clinical trial. JAMA. 2014;312(23):2510–20.
Sugawara M, Goto Y, Yamazaki T, Teramoto T, Oikawa S, Shimada K, et al. Low-dose aspirin for primary prevention of cardiovascular events in elderly Japanese patients with atherosclerotic risk factors: subanalysis of a randomized clinical trial (JPPP-70). Am J Cardiovasc Drugs. 2019;19(3):299–311.
Stewart RA, Wallentin L, Benatar J, Danchin N, Hagström E, Held C, et al. Dietary patterns and the risk of major adverse cardiovascular events in a global study of high-risk patients with stable coronary heart disease. Eur Heart J. 2016;37(25):1993–2001.
Crowe FL, Roddam AW, Key TJ, Appleby PN, Overvad K, Jakobsen MU, et al. Fruit and vegetable intake and mortality from ischaemic heart disease: results from the European Prospective Investigation into Cancer and Nutrition (EPIC)-Heart study. Eur Heart J. 2011;32(10):1235–43.
Acknowledgements
The authors thank the staff of the Chinese Center for Disease Control and Prevention, the Chinese Ministry of Health, the National Health and Family Planning Commission of China, and ten regional Health Administrative Departments. Most importantly, we are grateful to the study subjects for their participation and the project development and management teams based in Beijing, Oxford, and the ten regional research centers.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the National Key Research and Development Program of China (Grant numbers 2016YFC0900500, 2016YFC0900501, 2016YFC0900504), the Kadoorie Charitable Foundation in Hong Kong, and the Wellcome Trust in the UK (Grant numbers 202922/Z/16/Z, 088158/Z/09/Z, 104085/Z/14/Z).
Conflicts of Interest
Xiaojia Sun, Ruihong Sun, and Liming Zhang have no conflicts of interest that are directly relevant to the content of this article.
Availability of data and material
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Code availability
Not applicable.
Author Contributions
Xiaojia Sun and Ruihong Sun contributed to the conception. Liming Zhang contributed to the design of the work. Xiaojia Sun contributed to the acquisition, analysis, and interpretation of data for the work. Ruihong Sun contributed to interpretation. Liming Zhang contributed to the acquisition. Xiaojia Sun drafted the manuscript. Ruihong Sun and Liming Zhang critically revised the manuscript. All authors read and approved the final manuscript. All authors gave final approval and agreed to be accountable for all aspects of the work, ensuring integrity and accuracy.
Ethics approval
This study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. It was approved by the Chinese Center for Disease Control and Prevention Ethical Review Committee (No. 005/2004). Written informed consent was obtained from all participants from CKB.
Consent to participate
Written informed consent was obtained from the patients to publish this paper.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sun, X., Sun, R. & Zhang, L. The Effect of Aspirin on the Primary Prevention of Major Adverse Cardiac and Cerebrovascular Events in Chinese Older Adults: A Registration Study. Drugs Aging 39, 97–106 (2022). https://doi.org/10.1007/s40266-021-00906-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-021-00906-x