Abstract
Background
Little is known about trends in statin use in United States (US) nursing homes.
Objectives
The aim of this study was to describe national trends in statin use in nursing homes and evaluate the impact of the introduction of generic statins, safety warnings, and guideline recommendations on statin use.
Methods
This study employed a repeated cross-sectional prevalence design to evaluate monthly statin use in long-stay US nursing home residents enrolled in Medicare fee-for-service using the Minimum Data Set 3.0 and Medicare Part D claims between April 2011 and December 2016. Stratified by age (65–75 years, ≥ 76 years), analyses estimated trends and level changes with 95% confidence intervals (CI) following statin-related events (the availability of generic statins, American Heart Association/American College of Cardiology guideline updates, and US FDA safety warnings) through segmented regression models corrected for autocorrelation.
Results
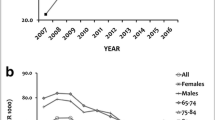
Statin use increased from April 2011 to December 2016 (65–75 years: 38.6–43.3%; ≥ 76 years: 26.5% to 30.0%), as did high-intensity statin use (65–75 years: 4.8–9.5%; ≥ 76 years: 2.3–4.5%). The introduction of generic statins yielded little impact on the prevalence of statins in nursing home residents. Positive trend changes in high-intensity statin use occurred following national guideline updates in December 2011 (65–75 years: β = 0.16, 95% CI 0.09–0.22; ≥ 76 years: β = 0.09, 95% CI 0.06–0.12) and November 2013 (65–75 years: β = 0.11, 95% CI 0.09–0.13; ≥ 76 years: β = 0.04, 95% CI 0.03–0.05). There were negative trend changes for any statin use concurrent with FDA statin safety warnings in March 2012 among both age groups (65–75 years: β trend change = − 0.06, 95% CI − 0.10 to − 0.02; ≥ 76 years: β trend change = − 0.05, 95% CI − 0.08 to − 0.01). The publication of the results of a statin deprescribing trial yielded a decrease in any statin use among the ≥ 76 years age group (β level change = − 0.25, 95% CI − 0.48 to − 0.09; β trend change = − 0.03, 95% CI − 0.04 to − 0.01), with both age groups observing a positive trend change with high-intensity statins (65–75 years: β = 0.11, 95% CI 0.02–0.21; ≥ 76 years: β = 0.05, 95% CI 0.01–0.09).
Conclusion
Overall, statin use in US nursing homes increased from 2011 to 2016. Guidelines and statin-related events appeared to impact use in the nursing home setting. As such, statin guidelines and messaging should provide special consideration for nursing home populations, who may have more risk than benefit from statin pharmacotherapy.



Similar content being viewed by others
References
Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999–2012. JAMA. 2015;314(17):1818–31. https://doi.org/10.1001/jama.2015.13766.
Todd A, Husband A, Andrew I, Pearson SA, Lindsey L, Holmes H. Inappropriate prescribing of preventative medication in patients with life-limiting illness: a systematic review. BMJ Support Palliat Care. 2017;7(2):113–21. https://doi.org/10.1136/bmjspcare-2015-000941.
Ngo-Metzger Q, Zuvekas SH, Bierman AS. Estimated impact of US preventive services task force recommendations on use and cost of statins for cardiovascular disease prevention. J Gen Intern Med. 2018;33(8):1317–23. https://doi.org/10.1007/s11606-018-4497-4.
Salami JA, Warraich H, Valero-Elizondo J, Spatz ES, Desai NR, Rana JS, et al. National trends in statin use and expenditures in the US adult population from 2002 to 2013: insights from the medical expenditure panel survey. JAMA Cardiol. 2017;2(1):56–65. https://doi.org/10.1001/jamacardio.2016.4700.
Tjia J, Cutrona SL, Peterson D, Reed G, Andrade SE, Mitchell SL. Statin discontinuation in nursing home residents with advanced dementia. J Am Geriatr Soc. 2014;62(11):2095–101. https://doi.org/10.1111/jgs.13105.
Campitelli MA, Maxwell CJ, Giannakeas V, Bell CM, Daneman N, Jeffs L, et al. The variation of statin use among nursing home residents and physicians: a cross-sectional analysis. J Am Geriatr Soc. 2017;65(9):2044–51. https://doi.org/10.1111/jgs.15013.
Zullo AR, Sharmin S, Lee Y, Daiello LA, Shah NR, John Boscardin W, et al. Secondary prevention medication use after myocardial infarction in US nursing home residents. J Am Geriatr Soc. 2017;65(11):2397–404. https://doi.org/10.1111/jgs.15144.
Mack DS, Tjia J, Hume AL, Lapane KL. Prevalent statin use in long-stay nursing home residents with life-limiting illness. J Am Geriatr Soc. 2020;68(4):708–16. https://doi.org/10.1111/jgs.16336.
US FDA. FDA Drug Safety Communication: New restrictions, contraindications, and dose limitations for Zocor (simvastatin) to reduce the risk of muscle injury. Center for Drug Evaluation and Research. 2011. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-new-restrictions-contraindications-and-dose-limitations-zocor#sa. Accessed 12 Feb 2019.
Rosenson RS, Farkouh ME, Mefford M, Bittner V, Brown TM, Taylor B, et al. Trends in use of high-intensity statin therapy after myocardial infarction, 2011 to 2014. J Am Coll Cardiol. 2017;69(22):2696–706. https://doi.org/10.1016/j.jacc.2017.03.585.
Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation endorsed by the World Heart Federation and the Preventive Cardiovascular Nurses Association. J Am Coll Cardiol. 2011;58(23):2432–46. https://doi.org/10.1016/j.jacc.2011.10.824.
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–934. https://doi.org/10.1016/j.jacc.2013.11.002.
Kutner JS, Blatchford PJ, Taylor DH Jr, Ritchie CS, Bull JH, Fairclough DL, et al. Safety and benefit of discontinuing statin therapy in the setting of advanced, life-limiting illness: a randomized clinical trial. JAMA Intern Med. 2015;175(5):691–700. https://doi.org/10.1001/jamainternmed.2015.0289.
Final Update Summary: Statin Use for the Primary Prevention of Cardiovascular Disease in Adults: Preventive Medication. US Preventive Services Task Force. 2016. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/statin-use-in-adults-preventive-medication. Accessed 10 Dec 2018.
Saliba B, Buchannan J. Making the investment count: revision of the Minimum Data Set for nursing homes, MDS 3.0. J Am Med Dir Assoc. 2012;13:602–10.
Thomas KS, Dosa D, Wysocki A, Mor V. The minimum data set 3.0 cognitive function scale. Med Care. 2017;55(9):e68–72.
Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999;54(11):M546–53.
Tibrewala A, Jivan A, Oetgen WJ, Stone NJ. A comparative analysis of current lipid treatment guidelines: nothing stands still. J Am Coll Cardiol. 2018;71(7):794–9.
Tran JN, Caglar T, Stockl KM, et al. Impact of the new ACC/AHA guidelines on the treatment of high blood cholesterol in a managed care setting. Am Health Drug Benefits. 2014;7(8):430–43.
Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. https://doi.org/10.1046/j.1365-2710.2002.00430.x.
Zhang F, Wagner AK, Ross-Degnan D. Simulation-based power calculation for designing interrupted time series analyses of health policy interventions. J Clin Epidemiol. 2011;64(11):1252–61. https://doi.org/10.1016/j.jclinepi.2011.02.007.
Mack DS, Baek J, Tjia J, Lapane KL. Statin discontinuation and life-limiting illness in non-skilled stay nursing homes at admission. J Am Geriatr Soc. 2020;68(12):2787–96. https://doi.org/10.1111/jgs.16777.
Mefford MT, Rosenson RS, Deng L, Tanner RM, Bittner V, Safford MM, et al. Trends in statin use among US adults with chronic kidney disease, 1999–2014. J Am Heart Assoc. 2019;8(2):e010640. https://doi.org/10.1161/JAHA.118.010640.
Mann D, Reynolds K, Smith D, Muntner P. Trends in statin use and low-density lipoprotein cholesterol levels among US adults: impact of the 2001 National Cholesterol Education Program guidelines. Ann Pharmacother. 2008;42(9):1208–15. https://doi.org/10.1345/aph.1L181.
Centers for Medicare and Medicaid Services. Surveys and Certification Guidance to Laws and Regulations for Nursing Homes. Guidance for Laws and Regulations. http://www.cms.gov/GuidanceforLawsAndRegulations/12_NHs.asp. Accessed 18 Oct 2020.
Dusetzina SB, Higashi AS, Dorsey ER, Conti R, Huskamp HA, Zhu S, et al. Impact of FDA drug risk communications on health care utilization and health behaviors: a systematic review. Med Care. 2012;50(6):466–78. https://doi.org/10.1097/MLR.0b013e318245a160.
Jacobson TA. NLA task force on statin safety—2014 update. J Clin Lipidol. 2014;8(3 Suppl):S1-4. https://doi.org/10.1016/j.jacl.2014.03.003.
Miller SC, Mor VN. The role of hospice care in the nursing home setting. J Palliat Med. 2002;5(2):271–7. https://doi.org/10.1089/109662102753641269.
Vossius C, Selbæk G, Šaltytė Benth J, Bergh S. Mortality in nursing home residents: a longitudinal study over three years. PLoS ONE. 2018;13(9):e0203480. https://doi.org/10.1371/journal.pone.0203480.
Gu A, Kamat S, Argulian E. Trends and disparities in statin use and low-density lipoprotein cholesterol levels among US patients with diabetes, 1999–2014. Diabetes Res Clin Pract. 2018;139:1–10. https://doi.org/10.1016/j.diabres.2018.02.019.
Chou R, Dana T, Blazina I, Daeges M, Jeanne TL. Statins for prevention of cardiovascular disease in adults: evidence report and systematic review for the US preventive services task force. JAMA. 2016;316(19):2008–24. https://doi.org/10.1001/jama.2015.15629.
Ramkumar S, Raghunath A, Raghunath S. Statin therapy: review of safety and potential side effects. Acta Cardiol Sin. 2016;32(6):631–9. https://doi.org/10.6515/acs20160611a.
Acknowledgements
The authors thank Robert Goldberg, PhD, for his guidance with this manuscript. The work was supported by the National Center for Advancing Translational Sciences, National Institutes of Health (TL1 TR001454) and the Agency for Healthcare Research and Quality (R36 HS026840). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by the National Center for Advancing Translational Sciences, National Institutes of Health (TL1 TR001454, Principal Investigator [PI]: Lapane; K24AG068300, PI: Jennifer Tjia), and the Agency for Healthcare Research and Quality (R36 HS026840, PI: Mack). This project was supported by grant number R36 HS026840 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Conflicts of interest
Jennifer Tjia is a consultant for CVS Health and Omnicare Long Term Care Pharmacy. Deborah Mack, Anne L. Hume, and Kate L. Lapane have declared no conflicts of interest for this article.
Ethical approval
This study used a routinely collected administrative and claims dataset and was approved by the University of Massachusetts Medical School Institutional Review Board (protocol number H00016995).
Availability of data and material
The authors are unable to share the data used to conduct this study per their Data Use Agreement with the Centers for Medicare and Medicaid Services via RESDAC.
Code availability
The SAS code will be made available on request to the authors.
Author contributions
DM and KLL had full access to all data in the study and are responsible for the data integrity and accuracy of the data analysis. Study concept and design: DM, AH, JT, and KLL. Acquisition of data: KLL. Analysis and interpretation of data: DM, AH, JT, and KLL. Statistical analysis: DM and KLL. Preparation of the manuscript: DM and KLL. Critical revision of the manuscript for important intellectual content: DM, AH, JT, and KLL. Obtained funding: DM. Study supervision: KLL. The final manuscript submitted for publication was read and approved by all authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mack, D.S., Hume, A.L., Tjia, J. et al. National Trends in Statin Use among the United States Nursing Home Population (2011–2016). Drugs Aging 38, 427–439 (2021). https://doi.org/10.1007/s40266-021-00844-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-021-00844-8