Abstract
Objectives
Pyrazinamide (PZA) has a controversial safety profile in older patients. We aimed to assess the frequency and risk factors for adverse drug reactions (ADRs) in patients over 75 years of age treated for tuberculosis with or without PZA.
Methods
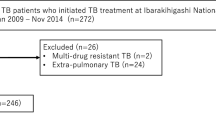
We conducted a retrospective monocentric study including patients aged over 75 years treated for active tuberculosis between 2008 and 2018. The frequency, type, seriousness, and causality assessment of ADRs to anti-tuberculosis treatment were compared between patients receiving PZA or not. Risk factors for ADRs were investigated using univariable and multivariable analyses by logistic regression.
Results
Among the 110 patients included, 54 (49.1%) received PZA (group 1) and 56 (50.9%) did not (group 2). ADRs to anti-tuberculosis drugs occurred in 31 patients (57.4%) in groups 1 and 15 (26.8%) in group 2 (p = 0.003). PZA-related ADRs occurred in 40.7% of exposed patients. Frequency of renal ADRs was higher in group 1 (9.3% vs 0%; p = 0.026). Rates of hepatic (18.5% vs 12.5%; p = 0.38), digestive (22.2% vs 8.9%; p = 0.054), and allergic (14.8% vs 5.4%; p = 0.12) ADRs were numerically higher in group 1 although the differences were not statistically significant. Serious ADRs occurred more frequently in group 1 (24.1% vs 8.9%; p = 0.03). The use of PZA was the only independent risk factor for ADRs to anti-tuberculosis drugs (odds ratio 3.75, 95% CI 1.5–9.6; p = 0.0056). No risk factors for PZA-related ADRs were identified.
Conclusion
In older French patients, the use of PZA was associated with more frequent ADRs to anti-tuberculosis drugs.
Similar content being viewed by others
References
Framework towards Tuberculosis Elimination in Low-Incidence Countries. Geneva: World Health Organization; 2014.
Davies PD. Tuberculosis in the elderly. Epidemiology and optimal management. Drugs Aging. 1996;8:436–44. https://doi.org/10.2165/00002512-199608060-00005.
Rajagopalan S. Tuberculosis and aging: a global health problem. Clin Infect Dis Off Publ Infect Dis Soc Am. 2001;33:1034–9. https://doi.org/10.1086/322671.
Santé Publique France. Tuberculose. 2020. https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/tuberculose/donnees/#tabs. Accessed 24 Jan 2020.
Yen Y-F, Feng J-Y, Pan S-W, Chuang P-H, Su VY-F, Su W-J. Determinants of mortality in elderly patients with tuberculosis: a population-based follow-up study. Epidemiol Infect. 2017;145:1374–81. https://doi.org/10.1017/S0950268817000152.
Zhang Y, Shi W, Zhang W, Mitchison D. Mechanisms of pyrazinamide action and resistance. Microbiol Spectr. 2014. https://doi.org/10.1128/microbiolspec.MGM2-0023-2013.
A controlled trial of 6 months’ chemotherapy in pulmonary tuberculosis. Final report: results during the 36 months after the end of chemotherapy and beyond. British Thoracic Society. Br J Dis Chest. 1984;78:330–6.
Schaberg T, Rebhan K, Lode H. Risk factors for side-effects of isoniazid, rifampin and pyrazinamide in patients hospitalized for pulmonary tuberculosis. Eur Respir J. 1996;9:2026–30.
Yee D, Valiquette C, Pelletier M, Parisien I, Rocher I, Menzies D. Incidence of serious side effects from first-line antituberculosis drugs among patients treated for active tuberculosis. Am J Respir Crit Care Med. 2003;167:1472–7. https://doi.org/10.1164/rccm.200206-626OC.
Di Gennaro F, Vittozzi P, Gualano G, Musso M, Mosti S, Mencarini P, et al. Active pulmonary tuberculosis in elderly patients: a 2016–2019 retrospective analysis from an Italian Referral Hospital. Antibiot Basel Switz. 2020. https://doi.org/10.3390/antibiotics9080489.
Kwon BS, Kim Y, Lee SH, Lim SY, Lee YJ, Park JS, et al. The high incidence of severe adverse events due to pyrazinamide in elderly patients with tuberculosis. PLoS ONE. 2020;15:e0236109. https://doi.org/10.1371/journal.pone.0236109.
Perriot J, Chambonnet E, Eschalier A. Managing the adverse events of antitubercular agents. Rev Mal Respir. 2011;28:542–55. https://doi.org/10.1016/j.rmr.2010.10.034.
Leung CC, Yew WW, Chan CK, Chau CH, Tam CM, Lam CW, et al. Tuberculosis in older people: a retrospective and comparative study from Hong Kong. J Am Geriatr Soc. 2002;50:1219–26. https://doi.org/10.1046/j.1532-5415.2002.50308.x.
Lin H-S, Cheng C-W, Lin M-S, Chou Y-L, Chang P-J, Lin J-C, et al. The clinical outcomes of oldest old patients with tuberculosis treated by regimens containing rifampicin, isoniazid, and pyrazinamide. Clin Interv Aging. 2016;11:299–306. https://doi.org/10.2147/CIA.S95411.
Bright-Thomas RJ, Gondker AR, Morris J, Ormerod LP. Drug-related hepatitis in patients treated with standard anti-tuberculosis chemotherapy over a 30-year period. Int J Tuberc Lung Dis Off J Int Union Tuberc Lung Dis. 2016;20:1621–4. https://doi.org/10.5588/ijtld.16.0370.
Kwon YS, Chi SY, Oh IJ, Kim KS, Kim YI, Lim SC, et al. Clinical characteristics and treatment outcomes of tuberculosis in the elderly: a case control study. BMC Infect Dis. 2013;13:121. https://doi.org/10.1186/1471-2334-13-121.
Miyazawa N, Horita N, Tomaru K, Tsukahara T, Takahashi R, Sasaki M, et al. Comparison of drug-induced hepatitis occurring in elderly and younger patients during anti-tuberculosis treatment with a regimen including pyrazinamide. Kekkaku. 2013;88:297–300.
Horita N, Miyazawa N, Yoshiyama T, Kojima R, Ishigatsubo Y, Kaneko T. Currently used low-dose pyrazinamide does not increase liver-injury in the first two months of tuberculosis treatment. Int Med Tokyo Jpn. 2015;54:2315–20. https://doi.org/10.2169/internalmedicine.54.5533.
Takaku T, Saito T, Nemoto K, Oisihi S, Hayashihara K. Comparison of adverse effects in tuberculosis patients over 80 years of age with and without pyrazinamide treatment. Eur Respir J. 2017;50:PA3045. https://doi.org/10.1183/1393003.congress-2017.PA3045.
Hagiwara E, Suido Y, Asaoka M, Katano T, Okuda R, Sekine A, et al. Safety of pyrazinamide-including regimen in late elderly patients with pulmonary tuberculosis: a prospective randomized open-label study. J Infect Chemother Off J Jpn Soc Chemother. 2019. https://doi.org/10.1016/j.jiac.2019.05.030.
Nahid P, Dorman SE, Alipanah N, Barry PM, Brozek JL, Cattamanchi A, et al. Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible Tuberculosis. Clin Infect Dis. 2016;63:e147–95. https://doi.org/10.1093/cid/ciw376.
Miller MD, Paradis CF, Houck PR, Mazumdar S, Stack JA, Rifai AH, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992;41:237–48. https://doi.org/10.1016/0165-1781(92)90005-n.
Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. the index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9. https://doi.org/10.1001/jama.1963.03060120024016.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649–55.
Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–63. https://doi.org/10.1001/jama.270.24.2957.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012.
MedDRA. 2020. https://www.meddra.org/. Accessed 28 Jan 2020.
Code de la santé publique—Article R5121-152. vol. R5121-152. 2020.
Bégaud B, Evreux JC, Jouglard J. Lagier G [Imputation of the unexpected or toxic effects of drugs. Actualization of the method used in France]. Therapie. 1985;40:111–8.
Huang Y-S. Genetic polymorphisms of drug-metabolizing enzymes and the susceptibility to antituberculosis drug-induced liver injury. Expert Opin Drug Metab Toxicol. 2007;3:1–8. https://doi.org/10.1517/17425255.3.1.1.
Sanwikarja S, Kauffmann RH, te Velde J, Serlie J. Tubulointerstitial nephritis associated with pyrazinamide. Neth J Med. 1989;34:40–6.
Namba S, Igari T, Nishiyama K, Hashimoto K, Takemura T, Kimura K. A case of pyrazinamide-associated myoglobinuric renal failure. Jpn J Med. 1991;30:468–72. https://doi.org/10.2169/internalmedicine1962.30.468.
Siddiqui AN, Khayyam KU, Sharma M. Effect of diabetes mellitus on tuberculosis treatment outcome and adverse reactions in patients receiving directly observed treatment strategy in India: a prospective study. BioMed Res Int. 2016;2016:7273935. https://doi.org/10.1155/2016/7273935.
Riza AL, Pearson F, Ugarte-Gil C, Alisjahbana B, van de Vijver S, Panduru NM, et al. Clinical management of concurrent diabetes and tuberculosis and the implications for patient services. Lancet Diabetes Endocrinol. 2014;2:740–53. https://doi.org/10.1016/S2213-8587(14)70110-X.
Morris CD. Pulmonary tuberculosis in the elderly: a different disease? Thorax. 1990;45:912–3. https://doi.org/10.1136/thx.45.12.912.
Pérez-Guzmán C, Vargas MH, Torres-Cruz A, Villarreal-Velarde H. Does aging modify pulmonary tuberculosis?: a meta-analytical review. Chest. 1999;116:961–7. https://doi.org/10.1378/chest.116.4.961.
Abbara A, Collin SM, Kon OM, Buell K, Sullivan A, Barrett J, et al. Time to diagnosis of tuberculosis is greater in older patients: a retrospective cohort review. ERJ Open Res. 2019. https://doi.org/10.1183/23120541.00228-2018.
Wang J-Y, Hsueh P-R, Jan I-S, Lee L-N, Liaw Y-S, Yang P-C, et al. Empirical treatment with a fluoroquinolone delays the treatment for tuberculosis and is associated with a poor prognosis in endemic areas. Thorax. 2006;61:903–8. https://doi.org/10.1136/thx.2005.056887.
Wang J-Y, Lee C-H, Yu M-C, Lee M-C, Lee L-N, Wang J-T. Fluoroquinolone use delays tuberculosis treatment despite immediate mycobacteriology study. Eur Respir J. 2015;46:567–70. https://doi.org/10.1183/09031936.00019915.
Wilkinson RJ, Rohlwink U, Misra UK, van Crevel R, Mai NTH, Dooley KE, et al. Tuberculous meningitis. Nat Rev Neurol. 2017;13:581–98. https://doi.org/10.1038/nrneurol.2017.120.
WHOcausality_assessment.pdf. 2020. https://www.who.int/medicines/areas/quality_safety/safety_efficacy/WHOcausality_assessment.pdf. Accessed 28 Jan 2020.
Acknowledgements
We warmly thank Mrs. Colleen Beck (Department of Infectious and Tropical Diseases, Toulouse University Hospital) for her proofreading. Preliminary results were previously presented as an abstract in the ECCMID 2020 congress abstract book in April 2020, and as a poster at the Journées Nationales d’Infectiologie (JNI) in September 2020 in Poitiers, France.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was not supported by any external funding.
Conflict of Interest
Stella Rousset, Margaux Lafaurie, Hélène Guet-Revillet, Caroline Protin, Jean Le Grusse, Hélène Derumeaux, Peggy Gandia, Fatemeh Nourhashemi, Laurent Sailler, Agnès Sommet, Pierre Delobel, and Guillaume Martin-Blondel declare that they have no conflict of interest.
Ethics Approval
This retrospective monocentric cohort study was approved by an institutional review board (RnIPH number 2020-51), in accordance with the French data protection authority (MR004, Commission Nationale de l’Informatique et des Libertés, CNIL number 2206723v0). Consultation of an Ethics Committee was not required as this was a non-interventional study that does not fall under the French Jardé law.
Consent to Participate and for Publication
According to French law on ethics, patients were informed that their codified data will be used for the study and for publication. Their non-opposition to the use of the data and to publication was collected.
Availability of Data and Material
Data are available upon reasonable request to Professor Guillaume Martin-Blondel.
Code Availability
Not applicable.
Author Contributions
Conceptualization: SR, GM-B, and PD; Methodology: SR, ML, AS, and GM-B; Software: SR; Investigation: SR, ML, HG-R, and HD; Data curation: SR; Writing–Original Draft: SR and GM-B; Writing–Review and editing: ML, HG-R, CP, JLG, PG, FN, LS, AS, and PD; Visualization: SR; Supervision: GM-B; Project administration: SR and GM-B.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rousset, S., Lafaurie, M., Guet-Revillet, H. et al. Safety of Pyrazinamide for the Treatment of Tuberculosis in Older Patients Over 75 Years of Age: A Retrospective Monocentric Cohort Study. Drugs Aging 38, 43–52 (2021). https://doi.org/10.1007/s40266-020-00811-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-020-00811-9